midterm photos Flashcards
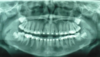
what type of PA is this

maxillary PM PA
want to see the contacts of D of C/PM, PM/PM, and 2ndPM/M
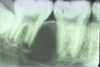
what type of pa is this

mx canine
you want to see the mesial contact of canine
what do we have here

an exta tooth lined up with adjacent teeth
we can tell due to a radiopacity in a tooth shape.
what do we see here

superimposed CI
it moves with beam movement so we can tell its palatal.

alveolar crest

floor/wall of mx sinus

zygomatic bone (inf. border)

zygomatic process of the maxilla

floor of nasal fossa

nasolabial fold
becomes more evident with age.

nasolabial fold

alveolar crest

external oblique line

internal oblique line

internal oblique line

inf alveolar canal

inf mandibular border
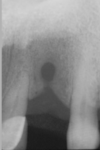
what do we see here
and is it buccal or lingual, and why:

we can tell its a mesioderm because of location (mx incisor)
Midline view, structure is covering mesial half of apex of LI, as the beam moves away from the midline the position moves to the mid of the root, more further away from midline can tell bc see the cuspid in there, now we see it covering the whole apex
As the beam moves to the right so did the structure, so SLOB, it is lingual/palatal.

what do we have here

- mesioderm
Plaque accumulation an extra probing pocket maybe
Esthetics
Crowding
Phonetics (maybe)
Spacing issues
-
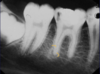
what do we see here
buccal, lingual and why?

- mesiodens- its a tiny tooth, doesnt necesarilly have the shape of a tooth though.
- superimposed at CI and then shift shot see it superimposed with LI, so it has moved to the right
- it is lingual/palatal to the erupting teeth because of SLOB
what do we have here
buccal, lingual and why:

we have a mesiodens
didnt give anothe view so cant tell if it is buccal or lingual lol
what do we see here?
buccal, lingual and why?

we have another mesiodens - on this xray we can kinda see a DEJ, with a change of radiolucencies.
can also see that the follicle is shrunken around the crown of the supernumerary tooth so probably WILL NOT cause a cyst, really is having no problems. If they have no problems, could actually maybe resorb.
no other XR given, cannot tell if B or L

what do we see here

supernumerary tooth

what do we have here?

can see a supernumerary tooth, identified and just monitored because not causing any problems could cause resorbption.