Midterm Flashcards
1st generation H1 antagonist anticholinergic adverse effects
dry mouth, blurred vision, urinary retention, impotence
1st generation H1 antagonist cardiovascular adverse effects
tachycardia, prolonged QTc, heart blocks, arrhythmias
1st generation H1 antagonist CNS adverse effects
somnolence, diminished alertness, slowed reaction time, impaired cognitive function (take in PM)
4 concepts of pharmacodynamics
absorption, distribution, biotransformation, elimination
Additive effects
1+1=2 summation of drugs taken concurrently (same receptor)
Antagonistic effects
1+1=0 one drug cancels/blocks effects of another
Antagonistic effects
1+1=0 one drug cancels/blocks effects of another
Are NSAIDs highly protein bound?
yes
Benadryl is prescribed as:
antiemetic, sedative, antipruritic
Benefits of benzos
less risk of tolerance and abuse, large margin of safety
Benzos are used for:
antianxiety, sedatives, anticonvulsants, muscle relaxants
Binding of glutamate to NMDA receptors allows
influx of Na and Ca
Cardiovascular Adverse Effects of NSAIDs
HTN, HF exacerbation, thrombotic events
Clearance
volume of plasma cleared of drug per unit time
Clinical uses for SSRIs
depression, panic disorders, OCD, PTSD, social phobias
Clonidine
selective partial alpha 2 agonist
CNS adverse effects of NSAIDs
headache, aseptic meningitis, hearing disturbances
conjugation
makes lipid soluble drugs water soluble (with glucoronic acid)
conjugation leads to:
a more polar compound that is more highly ionized at physiologic pH and therefore more easily extractable by the kidney via glomerular filtration
Consideration of patient taking lithium and anesthesia
decreased anesthetic requirements- may delay CNS recovery from barbiturates, response to NMBs may be prolonged
contraindication of benzo use for anxiety
history of alcohol or other substance abuse
Corticosteroids
naturally occurring from adrenal glands (hydrocortisone)
dermatologic adverse effects of NSAIDs
urticaria, rash, erythema multiforme
Does succinylcholine affect CP450?
no
Dosage of benzos for generalized anxiety
low dose, 2-5 mg (diazepam) up to 3 times daily
Effects of clonidine
antihypertensive, potentiate analgesic effects post-op induced by LA
End products of biotransformation are…
usually inactive and water soluble (easier excretion)
example of microsomal enzymes
cytochrome P450
Examples of 1st generation H1 antagonists
benadryl, chlorpheniramine, atarax
Examples of drugs that undergo zero order kinetics
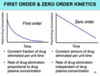
alcohol, phenytoin (dilantin)
Examples of drugs that undergo zero order kinetics
alcohol, phenytoin (dilantin), fluoxetine, salicylates
Examples of H2 receptor antagonists
ranitidine, famotidine, nizatidine, cimeditine
Examples of MAOIs
phenelzine, tranylcypromine, isocarboxazid
Examples of SSRIs
fluoxetine, paroxetine, sertraline, fluvoxamine, citalopram, escitalopram
First Order Kinetics
constant FRACTION of drug eliminated/unit time
First pass effect
drugs absorbed through GI tract enter portal venous blood and pass through liver before entering systemic circulation
GABA anion
chloride
GI adverse effects of NSAIDs
gastrophy, gastric bleeding, esophageal disease, pancreatitis
Goal lithium plasma concentration
1.0-1.2 mEq/L
GU adverse effects of NSAIDs
renal insufficiency (use with caution with renal disease), Na/fluid retention, papillary necrosis, interstitial nephritis
Half life
period of time required for the concentration/amount of drug to be reduced by half
hematologic adverse effects of NSAIDS
increased risk of intraop bleeding (platelet inhibition/dysfunction)
Hepatic clearance depends on
hepatic blood flow and hepatic extraction ratio
hepatic extraction ratio
drug removed from blood- limited by enzyme activity
How do benzos work?
facilitating actions of GABA (y-aminobutyric acid)- major inhibitory NT of nervous system
How long does it take for lithium to be effective?
several weeks
hydrolysis
split apart with water
In 1st order kinetics, rate of drug elimination is ? to drug plasma concentration
proportional (rate increases as drug concentration increases)
In order to be eliminated by the kidneys, can the drug still be bound to proteins?
no- must be non protein bound to cross into glomerular filtrate
In zero order kinetics, the rate of drug elimination is ? of drug plasma concentration
independent (rate does not increase as drug concentration increases)