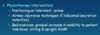
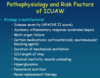
Midterm 2 - Lecture 7a/8a (Critical Care) Flashcards
what are reasons for ICU admission?

describe the periphral intervenous line
IV pumps can control rate of meds more percisely (newer)
Can mobilize with IV, just make sure not traction on iv etc
Could cause vein damage/dislodge it

describe an arterial line

what is mean arterial pressure?
- Waveform you see on prev machine
- Mean arterial pressure = systolic blood pressure, diastolic blood pressure formula
- MAP>60 ie for end organs (peripheral)

what are arterial line possible complications?

what are arterial line implications for PT?
- Make sure enough slack on arterial line (for pt’s) – people can bleed out (bc higher pressure arterial than venous) – grab gauze right away and apply pressure if happens!!
- First thing you look at when you enter a room is what equipment they have
- Catheter = source of infection, same with other lines – change it weekly otherwise infecion or pt can become septic
- Femoral line: before, pts were on bed rest but now not a problem with mobilization of these pts (see 2 studies) – even supine cyling is ok – however some people in some places will still not feel comfortable with it
- There is a pressure wave on monitor (for femoral) to watch – make sure it is intact

what is a central venous line?
-Pressure measurement and pressure waveform is given with hemodynamic monitoring = Central venous pressure

what is central venous pressure? - what 2 things does it give you information about?
- Cathiter goes just before R atrium therefore same as R atrium pressure
- Volume contributes to blood pressure overall and BP being measured right there
- Info about:
- 1) cardiac function
- 2) vascular volume

what factors increase and what decrease central venous pressure?
2) Pulmonary hypertension, COPD, right sided heart failure = backup pressure
3) Backup of pressure through the system
5) If tone increases, brings more blood to heart
6) Posiitve end expiratory pressure: when ventilator pushes air into lungs it is a + pressure at end of exp – lngs kept inflated a bit (+ pressure maintained) bc lungs encircle heart, + pressure is felt in that location where CVP is being measured (incr CVP bc of incr thoraccic pressure)
1) Decrease in vadcular volume (bleeding out)
2) If someone is lying down and they are sat up (legs down) or stand up (legs down) – bc blood goes w gravity and pools in legs
3) Bc opposite of peep – negative interthoracic pressure generated when breath in (incr with expiration – opposite)

what are possible complications and PT implications for a central venous line?
- Cellulitis = infection/inflammation of skin/tissues around cathiter
- Cathiter infect: Within the vessel/vein
- Sepsis: infection of blood
-
-Can mobilize with line!

what is a PICC line?
- Like central venus line, but location inserted more distally
- Often used for home care – can stay in for weeks or month – less complications bc inserted more distally
- If wet = increased infection risk
- Still a central venous line, just inserrted distally
- More for delivery of meds, not pressure – can be more damage for vessels when beds delivered this way

what is a port-a-cath?
- Seen with systic fibrosis pts
- Can administer meds on a regular basis

what is a pumonary artery catheter (swan ganz catheter)?
- Still inserted into a vein
- Diff from central venus line – this one goes further into R atrium – see slide – a vessel in the lungs (small balloon at the end – blocks off that vessel – cant be inflated for long – is only momentarily inflated to measure the pressure = wedge pressure)
- When balloon not inflated – measureing pulmonary artery pressure (increase pulm art pressure with: anything that is a problem in the L side of heart, due to back pressure – stenosis of mitral valve (L side) – incr resistance against which heart must contract, L sided heart pressure, also anythign increa vasc resistance in lungs (pulm hypertension, pulm embolis) = back pressure – increase pulm art pressure)
- 1) due to heart, 2) due to lungs = pulm art pressure increase

describe the pulmonary artery catheter pressure measurement
- Pressures generated in each chamber when catheter passed through
- 1) Looking at central venus pressure
- 2) Ventricle much more muscular, contracts harder therefore pressures higher – diastole = right atrial pressure
- 3) diastolic higher
- 4) small vessel (balloon inflated) we have the PA wedge pressure = much smaller pressure bc it is measure of end diastolic pressure in left ventricle
- Recall what increases pulm art pressure – pulmonary hypertension can also incr. – when balloon closes off the vessel – no more blood pushed from behind – but blood still draining from it, so it is sensing the blood that went away and the blood that stays behind end diastolic pressure caused by left side of heart – relaxation pressure of left side of heard when little balloon is inflated (gives info about the heart now)

how do you take pulmonary artery wedge pressure?
- Ie does not measure pulm hypertension
- Recall this is like pulmonary edema
- Cardeogenic pulm edema due to a heart prob, non-cardiogeninc = in absence of a heart problem
- Cardiogenic means you have L sided heart failure, cant pump blood out of heart, incr in hydrostatic pressure refleten in lung vasculature – pushes fluid into pulm interstitium and into alveoli (colour =pink and frothy, no protein in it, it is just the fluid)
- Wedge pressure gives the measure of heart failure

what are normal/abnormal values of PAWP?
Optimal filling bc of starling curve of heart – if put a bit more pressure (from blood) , can contract a bit more
Optimal fp is still normal
Alveolar ed = fluid in alveoli

what would elevate PAWP?
Overhyration bc of Incre end diastolic pr

what are possible complications and PT implications for a pulmonary artery catheter?
- Can stimulate arrythmia – bc it is passing through heart
- Pt implications
- People used to be very reluctant to move people with cath – used to be more people with this type of catheter
- Now not being as cautious, important to mobilize pts

NG tubes - what is the purpose, concerns, and PT implications
A feeding tube mainly, but can also be used as a suction to decompress stomach (remove air)
No problems with mobilization – can be disconnedted for walks
Aspiration – angle helps decr risk of vomiting/aspiration

name O2 low flow systems and high flow systems
Low Flow:
1) nasal prongs/nasal cannula
2) face mask
3) partial rebreathing mask
4) non rebreathing mask
High Flow:
1) air entrainment devices: venturi mask
describe nasal prongs - how much flow is delivered?
When you increased flow by 1l/minutes, FiO2 (oxygen flow) increases by 4%
Room air fio2 = 21%
If it is incr 1L/min, increased to 25%, etc
6L/min Beyond that not helpful for nasal prongs
Fraction of inspired oxygen depeds on breathign pattern – if inhaing faster, just get more air bc flow is fixed. Increase the flow if they are breathing faster

describe the face mask
- Goes over both mouth and nose – better for mouth breathers
- Higher faction of inspired oxygen – bc it is a resevoire now
- Rebreathing co2 if lowerflow
- Openings on side of the mask – flushes out fio2 – if you increase flow of system, o2 can be flushed out of holes – if you don’t want this, next slide

describe the partial rebreathing mask
- Still a partial rebreathign system
- 1/3 goes into resevoir (bag) 0 when they inhale they get that mized air, then additional exhale ….
- Bast bullet: Non-rebreathing mask to get higher

describe the non-rebreathing mask
Prevents exhaled air going into bag
- All depdt on breathing pattern

describe the air entrainment devices/venturi mask - advantages?
There are NOT dependant on persons breahting pattern!!!
Diameter smaller at one end, opening on edges = bigger for 100%, entrained by air mixing with valve – valve will say flow rate – ensurers that get precisely that amount of oxygen (%)
These Enable more precise delivery of FIO2 not dependant on pts breahting pattern!!
- Good to not deliver excess o2 etc
- can be Bubbled through sterile water to have humidity

what are complications of supplimental oxygen?
- Pressure that oxygen breathed in increased (divers/hyperberic chambers) affects CNS
- Premature babies – eye problems can lead to blindness

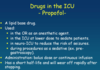
what is respiratory failure?
-What if they are receiving high levels of o2, but blood gasses not good? = that defines respitarory failure
-
- Supply vs demand that can be achieved
- Think of COPD pts (if they end up with infection) demand can exceed ability to provicde work necesaary for breathing – brings them to resp failure

what are 2 types of respiratory failure?
2 types of resp failure
Pump failure = resp muscles problem (infection, hyperinflated, ms and system can do it and system goes into fatigue – will have incr co2 bc cant ventilate adequately and retain co2)
Lung failure – more a gas exchange problem (diffusion prob, interstitial pneumonia impairs gas exchange, severe hypoxemia)
In either circumstance if appropriate blood gas is not achieved with supplimental o2, have to have mech ventilation.

what are the types of noninvasive mechanical ventilation? what are the advantages?
There is also invasive vent.
Iron lung – negative pressure ventilation (polio days) – pull out lung, having negative pressure – don’t use that anymore – not as effective
Positive pressure ventilation now used
CPAP used for people with sleep apnea
Bipap = delivered positive, then maintained at end of exp (like PEP)
More difficult to ween people of ventilators
No intubation = better (less resistance)

what are complications of noninvasive mechanical ventilation?
Asynchony – from effort of patient vs what machine is doing – sensors don’t pick p effort by pt
- Air can go into stomach, not directed through tube
- Hemodynamic: positive interthoracic pressure causes decrease in venous return to heart

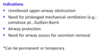
what are indications for intubation?
2) Ie links, asynghorny, blood gasses still bad
4) If they cant protect their airway – increased risk of aspirating
5) If having facal surgery/maxilla etc (cant apply face mask) etc

what are endotracheal intubation approaches?
- That’s why they have ng tube too for feeding when they are intubated

how is the endotracheal tube positioned?
End of tube: Carina = bifercation
There is a cuff on tube

describe what the endotracheal tube is like
Cuff with ballon at end that is in patient – cuff is inflated with sryinge to close off space btw endotracheal tube and trachea – this is a way that ensures that air doesn’t seep out around tube and out pts mouth – now positive pressure can come inflate the lungs – when person exhales passively lungs deflate (deflates on expiration)
- Some complications can arrive from cuff – it can herniate etc
- Prevents aspiration (fluid sectretion etc) – prevent infection
- Suctioning = pass catheter down endotracheal tube, applying neg pressure to be able to clear suction (people with tube canot clear without suction) – must be sterile!!
Top part = connected to ventilator tubing

describe the nasal vs oral ET tube
More difficult to insert bc narrower passage

describe a tracheostomy
If they anticipate longer recovery (over 10 days to get off ventilator) will do trach.
Suctioning is different

what are the indications for a tracheostomy?
Pt 1) tumor etc
Trach easier to manage secretions, don’t have to go as far and don’t involve the mouth
Cancer with airway removed may need permanent, ALS may have trach (progressive condition)
Can be progressively weened off – stoma heals over