MI: Opportunistic Viral Infections Flashcards
Describe some key overarching features of opportunistic viral infections.
- Occurs more frequently in immunocompromised patients
- More severe presentations that normal viral infections
- May be an absence of signs of infection (e.g. afebrile) and a lack of localising signs
- Fevers may have non-infectious causes
List some causes of immune compromise.
Metabolic/endocrine
- Alcohol abuse
- Diabetes mellitus
- Uraemia
- Malnutrition
Impaired barrier to infection
- Burns
- Haemodialysis
- IVDU
Pregnancy
Extremes of age
List some primary causes of immune compromise
- UNC93B deficiency and TLR deficiency (associated with predisposition to herpes simplex encephalitis)
- Epidermodysplasia verruciformis
- SCID
- Haemophagocytic lymphohistiocytosis in perforin deficiency
- HHV8 is associated with STIM1 mutation
NOTE: perforin deficiency is also assocaited with increased incidence of EBV
List some acquired causes of immune compromise
- Solid organ transplantation
- Bone marrow transplantation
- Immunosuppressive drugs
- Advanced HIV
- Measles can cause a prolonged immunodeficient state
Outline the natural history of HIV infection
- There is an early dramatic decline in CD4+ count accompanied by a sharp increase in viral load
- The CD4+ count then rises and viral load declines as the immune system brings it under control
- After a period of years, viral load climbs again and CD4+ count drops leading to AIDS

Describe the difference in immunosuppression with solid organ transplants compared to haematological transplants.
Solid organ transplantation - life-long immunosuppression
Haematological transplant - intense immunosuppression for a relatively short time
List the major classes of immunosuppressive drugs.
- Glucocorticoids
- Calcineurin inhibitors (cyclosporin, tacrolimus)
- Anti-proliferative agents (azathioprine, mycophenolate mofetil, sirolimus)
- Antibodies (e.g. rituximab)
- Co-stimulation blockers
List some iatrogenic causes of immunosuppression in order of increasing risk of opportunistic viral infection
- DMARDs and steroids (LOWEST RISK)
- Cytotoxic chemotherapy
- Monoclonal antibodies
- Solid organ transplant
- Advanced HIV
- Allogeneic stem cell transplant (HIGHEST RISK)
Outline the typic timeline of viral infections following solid organ transplant.
Reactive viral infections don’t tend to happen until >1 month after transplant
Early infections (<1 month) tend to be transmitted from the donor
How is the typical timeline of viral infections following solid organ transplan different from bone marrow transplants?
In bone marrow transplants, viral infections tend to to occur early (<1 month)
This is because bone marrow transplant patients receive intense immunosuppression
List some sources of infection in transplant patients.
Virus acquired from graft (e.g. HBV)
- Assessed by serology and donor risk assessment
Virus reactivated from the host (e.g. HSV)
- Tracked by monitoring serostatus, prophylaxis and pre-emptive therapy
New infection (e.g. VZV)
- Isolate, advise and vaccinate contacts and post-exposure prophylaxis
List some diseases that it is important to monitor for in post-transplant patients.
- CMV monitoring and prophylaxis
- EBV monitoring
- Adenovirus monitoring (in paediatric BMT)
- HSV prophylaxis if indicated
List the human herpes viruses
- HSV1
- HSV2
- VZV
- EBV
- CMV
- HHV6
- HHV7
- HHV8
What is the characteristic common feature of herpes viruses?
Latent infection (only a small subset of genes are expressed)
List the sites of latent infection of:
- VZV
- CMV
- EBV
- VZV = dorsal root ganglion
- CMV = monocytes
- EBV = B cells
In bone marrow transplant patients, describe the timescale in which the herpes infections tend to occur.
HSV, HHV6 and HHV7 tend to occur <1 month after transplant
CMV, VZV and EBV tend to reactive later
For herpes simplex virus, list:
- Symptoms
- Complications
- Treatment
- Symptoms
- Cold sores
- Stomatitis
- Mouth ulcers
- Recurrent genital disease
- Complications
- Cutaneous disseminated
- Oesophagitis
- Hepatitis
- Viraemia
- Treatment
- Aciclovir or valaciclovir
- Foscarnet
List some manifestations of VZV infection.
- Skin lesions
- Pneumonitis
- Encephalitis
- Hepatitis
- Purpura fulminans (neonates)
- Acute retinal necrosis
- VZV-associated vasculopathy
Describe the onset of shingles in post-transplant patients compared to HIV patients.
Shingles is an early manifestation in HIV
Shingles is a late manifestation post-transplant
Which features of zoster infection are associated with a high mortality?
Multi-dermatomal or disseminated infection
How can VZV infection be prevented post-transplant?
Aciclovir prophylaxis
Post-exposure prophylaxis with VZIG
List some manifestations of CMV infection.
- Retinitis
- Encephalitis
- Pneumonia
- Gastroenteritis
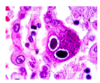
What is the pathological hallmark of CMV infection?
Owl’s eye appearance of lung pneumocytes due to the presence of inclusion bodies
How long after a transplant does CMV infection tend to occur?
Tends to develop <6 months after transplant



