Lower GI: Stomach to Anus Flashcards
1
Q

A
Stomach
-
mucosa (epithelium, lamina propria and muscularis mucosae)
- large folds → rugae
- flatten out as the stomach fills/stretches with foodstuffs
- adult stomach expand from ~1.5L of space in physiologically empty state to ~3L in full (distended) state
- large folds → rugae
2
Q

A
Stomach
3
Q

A
Stomach Mucosa
-
Mucous cells line the lumen (surface) of the stomach
- simple columnar cells
- filled with mucin granules → pale, washed-out
- dips down at regular intervals and these in-foldings form gastric pits
- lined by tall simple columnar cells
- dip further down into gastric glands → secret mucus, acid and digestive enzymes
4
Q

A
Gastric Gland Schematic
- parietal cells
- chief cells
3 Parts of Gastric Glands
-
upper part (isthmus)
- opens into gastric pit
-
midregion (neck)
- contains mixture of mucous neck cells and parietal cells
-
bottom (fundus or body/base)
- mixture of parietal cells and chief cells
- lower base mostly chief cells
5
Q

A
Stomach Mucosa - Parietal Cells
- aka oxyntic cells
- most numerous in body of a gastric gland but may also be found in neck and base
- large, round, pale-staining, eosinophilic cells
- secrete high concentrations of HCl into lumen of gastric glands
- also secrete intrinsic factor → facilitates vitamin B12 absorption in proximal small intestines
6
Q

A
Stomach Mucosa - Chief Cells
- mostly found at base of gastric glands
- round, basally located nucleus, and apical part of cells appears granular due to presence of secretory (zymogenic) granules
- Compared to parietal cells, chief cells much more basophilic
- produce pepsinogen I and II (inactive proenzymes)
- work with parietal cells
- HCl secreted by parietal cells → intraluminal pH of gastric glands low → converts released pepsinogen I and II to pepsin (protein breakdown)
- produce lipase
Try to locate muscularis mucosae
- underneath gastric glands
- band of smooth muscle
7
Q

A
Stomach Submucosa
- underlying muscularis mucosae
- highly vascularized and innervated CT layer
- lymphatic vessels present
8
Q

A
Stomach Muscularis Externa
- 3 layers of smooth muscle
- inner oblique
- middle circular
- outer longitudinal
- randomly oriented layers depending on what part of stomach → random arrangement is typical for organs that expel their contents
- muscle layers work to mix chyme and expel into small intestine
9
Q

A
Stomach Serosa
- moist, slippery surface
- mesothelial cells
- produce a thin film of serous fluid
- readily identified if using electron microscopy.
10
Q

A
Duodenum
11
Q

A
Duodenum Mucosa
- epithelium, lamina propria and muscularis mucosae
- duodenal villi
- projections of epithelium and lamina propria
- broad and leaf-shaped
- huge surface area
- simple columnar epithelial cells (enterocytes) and goblet cells
- epithelium dips down → intestinal glands or crypts of Lieberkühn
- extend to muscularis mucosae
12
Q

A
Duodenum Submucosa
- protective mechanism against HCl from stomach
-
glands of Brunner
- mucus-secreting
- unique to submucosa of duodenum → key identification feature
- can clearly see underlying muscularis mucosae of duodenum
- secrete alkaline glycoprotein → buffers HCl
-
glands of Brunner
13
Q

A
Duodenum Muscularis Mucosae
- 2 muscle layers
Duodenum Adventitia/Serosa
- depending on location, either serosa or adventitia
- some aspects of duodenum are lined by a serosa while others are lined by an adventitia
14
Q

A
Jejunum Mucosa
- epithelium, lamina propria and muscularis mucosae
-
villi
- projections of epithelium and lamina propria
- quite tall and finger-shaped
- simple columnar epithelial cells (enterocytes) with goblet cells
- number of goblet cells increases as move through small intestine
15
Q

A
Jejunum Mucosa - Lacteal
- core of each villus contains a lamina propria that is cellular and vascularized
- each villus contains one large lymphatic lacteal
-
lacteal
- large lymphatic capillary that absorbs dietary fat from small intestine
- fat is combined with lymph in lacteals → chyle
- individual lacteals merge → larger lymphatic vessels → transport fats to thoracic duct → empties into left subclavian vein
- capillaries and smooth muscle cells surround lacteals
- muscularis mucosae of mucosa well defined
16
Q
Jejunum
A
Mucosa
Submucosa
- typical supportive CT layer underlying muscularis mucosae
- blood vessels, lymphatics and nerves
Muscularis externa
- inner circular and outer longitudinal muscle layer
Serosa
- covers jejunum externally
17
Q

A
Ileum Mucosa
- epithelium, lamina propria and muscularis mucosae
-
villi
- stubby and club-shaped
- simple columnar epithelial cells (enterocytes) with goblet cells
- each villus has a single, large lacteal → absorption of dietary fats
- lacteals are not evident, as they were in the jejunum
- distinct muscularis mucosae is easily identified
18
Q

A
Ileum Mucosa - Paneth cells
- base of crypts immediately adjacent to muscularis mucosae
- deeply eosinophilic cells
- found throughout small intestine → especially numerous in crypts of ileum → identify ileum
- secretory cells → antimicrobial agents (e.g. lysozyme) into the crypts
19
Q

A
Ileum Submucosa
- typical CT layer with nerves, blood vessels and lymphatic channels
-
Peyer’s patches
- histological landmark of the ileum
- aggregates of lymphoid tissue that are important in immunity
- organized and permanent structures
- often contain germinal centres, while transient lymphocyte aggregations in other parts of the GIT will not have germinal centres
Ileum Muscularis externa
- inner circular muscle layer and outer longitudinal muscle layer
Ileum Serosa
- covers ileum externally
20
Q

A
Ileum Submucosa - Peyer’s Patches
21
Q

A
Ileum-Duodenum-Jejunum
- ileum → Peyers patches
- duodenum → glands in its sub-mucosa (the glands of Brunner)
- jejunum → neither.
22
Q

A
Colon
- includes cecum, appendix, ascending colon, transverse colon, descending colon, sigmoid colon and rectum
-
function
- stores intestinal contents before discharge
- absorbs water and electrolytes
- secretes mucus for protection and lubrication
23
Q

A
Colon Mucosa
- epithelium, lamina propria and muscularis mucosae
- lacks villi
-
simple columnar epithelium
- forms deep intestinal glands/crypts 2x-3x as long as crypts of small intestine
- epithelium contains many more goblet cells than small intestine
- number of goblet cells increases from cecum to rectum
-
lamina propria
- highly cellular and also contains GALT (gut-associated lymphatic tissue) and many defined lymphoid follicles → may or may not pierce
underlying muscularis mucosae to penetrate the submucosa
- highly cellular and also contains GALT (gut-associated lymphatic tissue) and many defined lymphoid follicles → may or may not pierce
24
Q

A
Colon
25

**Colon Submucosa**
* typical but does contain more **adipose tissue** than small intestine submucosa
**Colon Muscularis externa**
* inner circular layer and an **incomplete outer longitudinal layer that is not of uniform thickness**
* **Meissner’s and Auerbach’s plexuses**
* **Meissner's**
* inner surface of muscularis externa
* **Auerbach's**
* between the 2 layers of muscularis externa
**Colon Serosa and adventitia**
* covered externally by a serosa, incomplete serosa or adventitia
* depends on its location in abdomen
26
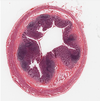
**Appendix**
* very much same structure as rest of colon with major difference being **larger numbers of lymphoid follicles**
* nodules are located in lamina propria of appendix and may protrude into lumen → stellate appearance in inflamed condition
* nodules also frequently pierce muscularis mucosae and protrude into submucosa
* abundance of lymphoid tissue (GALT) and defined lymphoid follicles → immunological function
27

Acute Appendicitis
28

Esophagogastric Junction
29

**Esophagogastric Junction**
* junction between esophagus and stomach
* epithelium abruptly changes from **nonkeratinized stratified squamous epithelium** (in the esophagus) to **simple columnar epithelium** (in the stomach) → serrated border = **Z line**
* easily recognized during endoscopy
* esophagus → pale
* stomach → deep red
* **Clinical significance**
* **Barrett’s esophagus**
* simple columnar epithelium of stomach replace stratified squamous epithelium in inferior portion of esophagus
* epithelium adapting to acid exposure (over a long period of time) from **reflux esophagitis**
* epithelial changes → strong association as premalignant condition of **esophageal adenocarcinoma**, particularly lethal
* **Mallory-Weiss Syndrome**
30

Gastroduodenal Junction
31

**Gastroduodenal Junction**
* transition from gastric mucosa to villous epithelium of duodenum occurs much more gradually
* has portions of gastric epithelium that extend up into duodenum → there are regions of gastric epithelium in duodenum and regions of duodenal mucosa in stomach
* implemented in one of types of Crohn’s disease
32

Anorectal Junction
33

**Anorectal Junction**
* epithelium changes from **simple columnar epithelium** (rectum) → **transitional zone of stratified columnar epithelium** → **nonkeratinized stratified squamous epithelium** (anal canal)
* boundary between rectum and anus = **pectinate** **line**
* common site of neoplastic changes


