Lipids 1-3 Flashcards
What are the functions of lipids?
1) E-storage
2) biological membranes
3) messenger molecules
4) building blocks for hormones
5) covalent modification on protiens
What are the classes of lipids?
1) FAs
2) Neutral glycerides
3) phospholipids
4) sphingolipids
5) cholesterol & derivatives
What is the structure of FAs in humans?
- Even numbered
- 12-24 carbons long
- all DBs are cis, DBs separated by exactly 1 methylene group, unbranched

What is the naming/numbering of lipid’s carbons?

What is the importance of the cis-double bond?
It prevents stacking, so fatty acids have lower melting temperature. More double bonds, the most likely a FA is in liquid state at room temperature.
What are essential FAs?
- FAs that we cannot synthesize; those with omega 3 bonds
- Ex. Linoleic acid & a-Linolenic acid
Which fats are healthier?
- Unstaurated fats
- Less packed
What are the differences beween mediterranean. wester, and low-fat diet?
- Mediterranean diet: 38% fat (mainly monosaturated) , 42% carbs, 20& protien
- Western diet: 38% fat (mainly saturated)
- Low-fat diet: 20% fat, 65% carbs, 15% protein
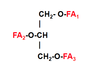
What are neutral glycerides?
- Glycerol, mono-di-tri-glycerides
What is the structure of phospholipids?

- The alcohol can be: serine, ethanolamine, choline, inositol, glycerol
- Name: Phosphatidyl serine

What is cardiolipin?
- Its is phospholipid in mitochondrial inner membrane
- Also named Diphosphatidyl glycerol
What are sphingolipids?
- Lipids containing a backbone of sphingoid bases, a set of aliphatic amino alcohols that includes sphingosine.

What is the structure of Sphingomyelin?

What is the structure of Glycosphingolipids?

What is the importance of cholesterol?
- Membrane component
- Bile salts
- Steroid hormones (progesterone, estrogen, aldosterone, cortisol, androgens)
- Vitamin D
*Chylomicrons release contents in cell surface
*Dietary cholesterol has little influence on plasma cholesterol in healthy people
*HMGcoA reductase is always active in patients with high cholesterol. It synthesizes cholesterol always.
What are lipoproteins?
–>Assembly of proteins & lipids, which allow fats to move through the water inside and outside cells. Proteins serve to emulsify fat molecules.
–> Ex) chylomicron, LDL(β;-lipoprotein), VLDL (Pre β-lipoprotein), HDL (α-lipoprotein)
–> LDL

What apoprotein in LDL is related to heart disease?
B100
What generates the main lipoproteins?
1) HDL is generated by liver & intestine, (lowest TAG, high cholesterol)
2) LDL is generated by VLDL, (LDL has low TAG and highest cholesterol)
3) VLDL is generated by liver, (high TAG, low cholesterol)
4) Chylomicrons are generated by the intestines, (highest TAG, lowest cholesterol)
What are the functions of the main lipoproteins?
- HDL: deliver cholesterol from peripheral tissues to the liver for elimination or for ssteroid synthesis
- LDL: deliver cholesterol to the peripheral tissues and to the liver
- VLDL: deliver endogenous TAG to peripheral tissues
- Chylomicrons: deliver dietary TAG to peripheral tissues (adipose tissue, muscle, lung)
How are lipids broken down in the body?
- Lipids degradation primarily occurs in the small intestine, where bile salts emulsify & pancreatic enzymes degrade these 3 releasing FAs:
CE–cholesterol esterase–> cholesterol + FA
PL –Lipases–> Glyceryl-P-ryl-choline + 2FAs
TAG – pancreatic lipase–> 2-monoacyl-glycerol + 2FAs
- In the form of chylomicrons, lipids are taken to the lymph & then to the blood
What are some characteristics of bile salts?
- Needed in small intestine to emulsify fats
- The bile duct connects the liver to the intestines
- Made in the liver
- ~25g used during digestion/day
- Most bile salts are re-absorbed in the intestines
- Made out of cholesterol (0.5/day) to replace bile salts that were excreted
What are the types of gallstones?
1) Cholesterol stones: light yellow to dark green or brown, 80% cholesterol by weight
2) Pigment stones: small and dark. Bilirubin and calcium salts found in bile. >20% cholesterol
3) Mixed stones: 20-80% cholesterol. Calcium carbonate, palmitate phosphate, bilirubin, & other bile pigments
What is PTL?
Pancreatic triglyceride lipase: from pancreas, only cleaves at position 1 and 3
–> In the intestinal lumen, with bile salts, it converts:
TAG --\> two FAs + one 2-monoacylglycerol
–> Become mixed miscelles
–>Transported through FATP4 to i_ntestinal mucosa_
What happens with fats at the intestinal mucosa (enterocytes)?
1) Reform triglycerides: 2 FAs+ 1 2-MAG —> TAG
2) P-lipids & apoB-48/C/E make TAGs into chylomicrons (only carry fat from diet)
3) Chylomicrons also contain: phospholipids, fat-soluble vitamins, apolipoprotein B-48 from AAs, & cholesteryl ester
4) Chylomicrons go into the lymphatic system and then the blood stream


