Lecture 7: Connective Tissue Diseases Flashcards
(74 cards)
Homogenous/diffuse ANA staining patterns may be associated with what 3 underlying conditions?
- Drug-induced SLE**
- Sjogren’s syndrome
- SLE

What does the centromere pattern of ANA staining refer to and what condition is it seen in?
- Presence of 30-60 uniform speckles distributed throughout the nucleus of resting cells
- Limited systemic sclerosis (CREST)

A nucleolar pattern of ANA staining may be seen in which 2 conditions?
- Diffuse systemic sclerosis
- SLE

What are 3 positive serology findings seen in SLE; which is most specific and correlates with disease activity?
- (+) ANA
- (+) anti-ds DNA –> correlates w/ disease activity; most specific
- (+) Sm (Smith)

What will be seen with complement activity during active SLE?
↓ C3 or C4 due to ↑ consumption

Anti-Phospholipid Antibody Syndrome (APS) arises in association with what?
- 1/3 of SLE pt’s (secondary APS)
- Can also be present w/o a dx of SLE (primary APS)
Of the 3 types of antiphospholipid antibodies, what is the significance of Type One?
Causes biologic false-(+) tests for syphilis

Of the 3 types of antiphospholipid antibodies, what is the significance of Type Two; how is it detected?
- Lupus anticoagulant
- Risk factor for venous and arterial thrombosis and miscarriage
- Causes prolongation of aPTT
- Presence is confrmed by an abnormal dilute Russell viper venom time (DRVVT)

Of the 3 types of antiphospholipid antibodies, what is the significance of Type Three?
- Anti-cardiolipin antibodies
- Directed at a serum co-factor Beta2GPI

Which 2 serology findings if positive correlates with lupus-like syndrome/drug-induced?
- (+) ANA
- (+) Anti-histone antibodies (95%)

Neonatal lupus affects children born of mothers with which serum antibodies?
Anti Ro (SSA) or La (SSB) Abs

Which complication may arise in children with neonatal lupus?
Permanent complete heart block
What are 4 treatment strategies/drugs used for SLE?
- Avoid sun exposure, wear sunscreen
- NSAIDs
- Corticosteroids (topical or systemic)
- Hydroxychloroquine

What is the hallmark finding of Scleroderma (systemic sclerosis)?
- Thickening and hardening of the skin
- Microangiopathy and fibrosis of the skin and visceral organs

Which antibodies are specific to diffuse cutaneous scleroderma?
- (+) Anti-Scl 70 –> aka Anti-(DNA) topoisomerase I
- Anti-RNA polymerase III

Which antibody is specific to the limited cutaneous type of scleroderma?
(+) Anti-centromere

Which type of imaging may be appropriate for working up Scleroderma?
- CXR
- Barium swallow if indicated
- Hand x-rays may show distal tuft resorption and calcinosis

Which manifestations of disease are more pronounced in the limited cutaneous type of Scleroderma?
- Vascular manifestations i.e., digital ischemia and progressive Pulmonary artery HTN
- Think is limited to pulmonary a.; while diffuse is all over and caused interstitial lung disease

A patient with diffuse cutaneous systemic sclerosis (scleroderma) in renal crisis may have what lab finding?
Hemolytic anemia
What is localized scleroderma and most often affects whom?
- Benign skin conditions; most often affects children
- Discreet areas of discolored skin induration; patches = morphea

Deficiency of which nutrients is common in systemic sclerosis patients with GI involvement?
Fat + protein + B12 + vitamin D

Which esophageal manifestations may be seen with systemic sclerosis?
Strictures, Barret esophagus –> ↑ risk of esophagal adenocarcinoma

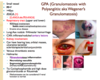
Which disease manifestations of the stomach may be seen in systemic sclerosis?
- Gastric Antral Vascular Ectasia (GAVE) aka Watermelon stomach
- Gastroparesis

Which biliary disease manifestation may be seen with systemic sclerosis; what is the associated antibody?
Primary biliary cirrhosis –> anti-Mitochondrial Ab