Lecture 7: Antacids and Anti-Ulcer Agents Flashcards
Antacids are used only for what?
Short-term, temporary relief of mild pain and sx’s of PUD/GERD
What are the 3 low-systemic agents used as antacids?
- Aluminum-based
- Calcium-based
- Magnesium-based
What is the high-systemic agent used as an antacid?
Sodium salts
What is the MOA of antacids?
Do they inhibit secreton or production of acid?
- Combine chemically w/ H+ ions and make byproducts (i.e., H2O, CO2..)
- They DON’T reduce acid secretion or production
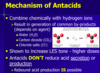
With chronic use of antacids what may be seen with acid production?
Rebound acid production
Which 2 antacids have rapid onset, a long duration of action, and good/very good acid neutralizing capacity?
1) Calcium = very good ANC
2) Magnesium = good ANC

What is the onset, duration of action, and acid neutralizing capacity of sodium-based antacids?
- Onset = rapid
- DOA = short
- ANC = fair/good

What is a supplemental compound that is often co-administered with antacids?
MOA and use?
- Simethicone
- A surfactant - decreases surface tension
- Aids in the expulsion of gas

What are two dose-related adverse effects associated with aluminum-based antacids?
- Constipation
- Hypophosphatemia –> acute tx for hyperphosphatemia
What are two dose-related adverse effects associated with magnesium-based antacids?
- Diarrhea (stool-softening/laxative-like activity)
- Hypermagnesemia
What are four dose-related adverse effects associated with calcium-based antacids?
May produce what syndrome?
- Constipation (‘C’ for Calcium)
- Hypercalcemia –> ‘Milk-Alkali Syndrome’ = nephropathy and metabolic alkalosis
- Hypophosphatemia
- Calcium-based kidney stones
What are three dose-related adverse effects associated with sodium-based antacids?
- Gas/flatulence (‘bicarb. burp’)
- Hypernatremia
- Metabolic alkalosis
Are there drug interactions that need to be considered when taking antacids?
What is the recommendation for dosage timing in a patient taking other meds + antacids?
- TONS!
- Take all antacids 1-2 hours BEFORE other meds OR
- 2-4 hours AFTER other meds
What is the suffix for the H2 Receptor Antagonists used as Anti-Ulcer drugs?
List the 4 most common
-tidine

- Cimetidine
- Famotidine
- Nizatidine
- Ranitidine
What is the suffix for the PPI’s used as Anti-Ulcer drugs?
List the 6 most common
-prazole

- Lansoprazole
- Dexlansoprazole
- Omeprazole
- Esomeprazole
- Pantoprazole
- Rabeprazole
What is the surface acting agent used as an anti-ulcer drug?
Sucralfate
What is the PGE1 analog used as an anti-ulcer drug?
Misoprostol
Some of the H2 receptor antagonists used as anti-ulcer drugs are formulated with what?
Antacids –> calcium + magnesium

What is the MOA of the H2-receptor antagonists used as anti-ulcer drugs?
Reversibly inhibit H2-receptors on baso-lateral membrane of parietal cells

The adverse effects associated with H2-receptors antagonists are primarily of what 2 type?
- GI-related –> Nausea/Diarrhea/Constipation
- CNS-related –> Headache

The H2-receptor antagonist, Cimetidine, has been associated with what rare side-effects with long-term high doses?
- Decreases testosterone binding to androgen receptors
- Gynecomastia in men
- Galactorrhea in women

Which H2-receptor antagonist used as an anti-ulcer drug is a prototypical inhibitor of several CYP450 isoenzymes?
Why is this bad?
- Cimetidine
- LOTS of drug-drug interactions

H2-receptor antagonists as anti-ulcer drugs are relatively contraindicated during pregnancy, but which drugs in this class can be used if absolutely necessary?
- Ranitidine (most data) or
- Famotidine
What is the MOA of the PPI’s (-prazoles) used as anti-ulcer drugs?
- Covalently bind sulfhydryl groups of H+/K+-ATPase at parietal cells secretory sites
- Inhibit gastric acid secretion by irreversibly inhibiting “-ase” pumps










