Lecture 4: Types of Necrosis Flashcards
(47 cards)
What are the five main types of necrosis?
- Coagulative necrosis
- Liquefactive necrosis
- Caseous necrosis
- Gangrenous necrosis (both wet and dry)
- Fat necrosis
What will the cytoplasm of a necrotic tissue look like?
- Hypereosinophilic (or, more pink)
- Homogenous
- Smudged (really hard to see cell detail)
- Swollen, then shrunken (depending on the phase of necrosis)
- Pale/ghost-like
What are the gross indications of necrosis?
- Pale, unless there are vascular changes, hemmorhage, or inflammation
- Sharp line of demarcation
- Friable - loss of tensile strength
What happens to tissue once it’s necrotic?
There are 4 main fates…
Fates of necrotic areas:
- Liquefied (drains into lymphatics)
- Calcified (dystrophic calcification)
- Phagocytosis (thanks macrophages!)
- Encapsulated (fibrous encapsulation as protection)
The _______ is a good indicator of necrosis.
The nucleus is a good indicator of necrosis.
The appearance of necrosis depends on….?
The appearance of necrosis depends on the type of cell, the cause of the lesion, and the length of duration
What is pyknosis?
Pyknosis is the irreversible condensation of chromatin in the nucleus of a cell undergoing necrosis or apoptosis. It is followed by karyorrhexis, or fragmentation of the nucleus.
The nucleus has shrunken to a small, dark structure
Extra, from Wikipedia: Pyknosis is also observed in the maturation of erythrocytes (a red blood cell) and the neutrophil (a type of white blood cell). The maturing metarubricyte (a stage in RBC maturation) will condense its nucleus before expelling it to become a reticulocyte. The maturing neutrophil will condense its nucleus into several connected lobes that stay in the cell until the end of its cell life.
What is karyorrhexis?
Karyorrhexis is the destructive fragmentation of the nucleus of a dying cell, whereby its chromatin is distributed irregularly throughout the cytoplasm. It is usually preceded by pyknosis and can occur as a result of either programmed cell death (apoptosis), senescence, or necrosis.
Dr. F-W stated in the review that she views Kayorrhexis and Karyolysis as essentially synonyms.
What is karyolysis?
Karyolysis is the complete dissolution of the chromatin of a dying cell due to the enzymatic degradation by endonucleases. The whole cell will eventually stain uniformly with eosin after karyolysis. It is usually preceded by karyorrhexis and occurs mainly as a result of necrosis, while in apoptosis after karyorrhexis the nucleus usually dissolves into apoptotic bodies.
Again, synonymous with karyorrhexis.
What does the absence of a nuclei mean for an RBC?
Nothing, that’s the RBC’s normal state of affairs.
RBC are long-lived, but as they don’t have a nucleus, they can’t replicate
Coagulation necrosis:
- Most typically occurs in the CNS
- Appears as dry, layered exudate
- Features preservation of cell outlines
Coagulation necrosis:
- Features preservation of cell outlines
Liquefactive necrosis:
- Most typically occurs in the CNS
- Appears as dry, layered exudate
- Features preservation of cell outlines
Liquefactive necrosis:
- Most typically occurs in the CNS
Caseation necrosis:
- Most typically occurs in the CNS
- Appears as dry, layered exudate
- Features preservation of cell outlines
Caseation necrosis:
- Appears as dry, layered exudate
Define anisocytosis
This is from her “unknowns” word cloud, from Lab 2 CCAs. Not sure if we need to know these for this class, but better safe than sorry.
Anisocytosis means that cells are of unequal size. Typically used in reference to RBC’s

Define hemosiderosis
This is from her “unknowns” word cloud, from Lab 2 CCAs. Not sure if we need to know these for this class, but better safe than sorry.
Hemosiderosis is a form of iron overload disorder resulting in the accumulation of hemosiderin.
Hemosiderin is an iron-storage complex. It is always found within cells (as opposed to circulating in blood) and appears to be a complex of ferritin, denatured ferritin and other material. The iron within deposits of hemosiderin is very poorly available to supply iron when needed. Hemosiderin can be identified histologically with “Perls’ Prussian-blue” stain. In normal animals, hemosiderin deposits are small and commonly inapparent without special stains. Excessive accumulation of hemosiderin is usually detected within cells of the mononuclear phagocyte system (MPS) or occasionally within epithelial cells of liver and kidney.
Define cholestasis
This is from her “unknowns” word cloud, from Lab 2 CCAs. Not sure if we need to know these for this class, but better safe than sorry.
Cholestasis is a condition where bile cannot flow from the liver to the duodenum. The two basic distinctions are an obstructive type of cholestasis where there is a mechanical blockage in the duct system that can occur from a gallstone or malignancy, and metabolic types of cholestasis which are disturbances in bile formation that can occur because of genetic defects or acquired as a side effect of many medications.
Define petechial
This is from her “unknowns” word cloud, from Lab 2 CCAs. Not sure if we need to know these for this class, but better safe than sorry.
A petechia is a small (1 - 2 mm) red or purple spot on the skin, caused by a minor hemorrhage (broken capillary blood vessels).

Are the circled cells in good health? If not, what’s going on?

If the blue line were an epithelial surface, the epi cells are attached to a basement membrane in health.
But if those cells undergo acute cell swelling and/or die, they tend to round up; there’s a change to the cytoskeleton. They may eventually detach from the basement membrane, and you may see them floating off into space like we see here.
So, another indicator that epithelial cells are dead or dying, is that they detach from the basement membrane
What is a zone of hyperemia?
A zone of hyperemia is a bright red zone around an area of necrosis. It’s a vascular change in response to that necrosis, and is an indication that the body has responded/reacted to it.
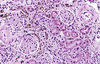
What you see, histologically, on a cell undergoing coagulation necrosis?
Coagulation necrosis:
- Cell and tissue are still identifiable
- Delayed autolysis, due to decreased pH
- Nuclear change: There probably won’t be a nucleus, but if there is, it’s pyknotic
- Cytoplasm: Homogenous hypereosinophilic
What are the main causes of coagulation necrosis?
The main causes of coagulation necrosis are:
- Hypoxia
- Cell membrane injury
- Toxins
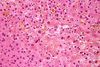
What tissues are most commonly affected by coagulation necrosis?
Most commonly affected tissues from coagulation necrosis:
- Liver
- Kidney
- Muscle
- Neurons
What do you see here? (circled in blue)

The circled area is an example of dystrophic calcification.
Not uncommon, even early on in coagulation necrosis
This would not be why the dog died, but it’s important to recognize it as a feature of coagulation necrosis
Zenker’s necrosis is synonymous with…?
Zenker’s necrosis is synonymous with coagulation necrosis (of skeletal or cardiac muscle, not really smooth)






