Lecture 4 - Medical Cardiac Conditions Flashcards
what are the clinical manifestations of CAD?
1 = a partial blockage
2 = complete blockage
3 and 4 = Damage to the vessels of the heart (complication to a heart attack)

describe the myocardial ischemia chart (main points)

describe the demand side of the myocardial ischemia chart
Wall tension - obstruction downstream, or invcreased volume to heart = heart working more, and incr workload
Exercise can increase contractility but so can anxiety, stress, increased temperature etc

describe the supply side of the myocardial ischemia chart
Gas exchange problems will also affect 1 and 2 – there is a systemic as well as a direct heart effect
Aortic driving pressure = blood pressure
Hypotension decr oxygen supply, hyper increases demand (look at afterload)

describe transient vs prolonged ischemia
Greater wall tension = greater collapse of coronary artieries (decr afteload, incr pre-load)
4 = complete occlusion (over period of time), causing damage to heart

angina pectoris symptoms?

where is angina located?
Precordial = a bit to the left over heart
Sensation not the same btw men and women
Basically anywhere over the waist can be angina!!

precipitating factors and associated conditions of angina?

what are the 3 types of angina?
1) stable angina
2) unstable angina
3) prinzmetals (atypical or variant) angina
describe stable angina
2 = the same level of effort/stress triggers it
3 = ie stop exercising and goes away after some time
4 = nitroglycerine mentioned before helps with heart muscle
If someone is exercising and hr or bp increases = rate pressure product, closely related to demand of the heart
Angina will eb reproduced at the SAME RPP in stable angina

describe unstable angina
Ie if now less effort is needed to have angina, may be indicative to disease progression
If pain not relieved by 3 nitro tablets and after 15 mins is not being relieved, should go to hospital asap - bc may be having a heart attack at that point

describe prinzmetals angina
Cocaine triggers vasospasm for example
Angina will see a depression, with heart attack, depression (ST segment)
Last point: Dilates blood vessels and decr heart workload, afterload decreases

describe asymptomatic (silent) myocardial ischemia
Diabetes bc reduced sensation
Some patients never complain of chest pain or have symptoms, but you can see it on ECG etc


Whether jaw pain was there before treadmil
Measure RPP - See if you stop the exercise if it decreases, if you increase workload to same point and it returns = make sure you don’t go past that point
If it is a new symptom and havent had angina before, stop treatement and refer back to Dr before continuing exercise with this pt.

Increase in venus return (blood going to heart) – increased preload which increases wall tension and increases myocardial oxygen demand
therefore angina wont be decreased when supine
Someone with angina should rest in an upright position
*nitro takes 10 mins to work roughly
describe myocardial infarction and causes
MI = actual damage that occurs to heart
Coronary artery spasm could shut down entire vessel
Longer block = greater necrosis risk
Hypovolemia = bleeding out due to major trauma etc
Leukocytes get rid of dead tissue and then fibroblasts are layed down = scarring tissue in the dead area
2 = greater blockage (ie more distal vessels = smaller)
3 = this is how its diagnosed

what are the major areas og MI and their implications?
1 = primarily RightVentricle affected
2 = lowest ejection fractions associated with this, worst one to have, widow-makers

clinical symptoms of acute MI?
If the 3 tablets after 15 mins doesn’t releive
Diaphoresis is imvolved bc heart is not functioning, and tissue not getting oxygenated
3rd last point – blood not going to brain
Last point – compensatory response

describe STEMI vs non-STEMI MI
Determined by extent of damage (full thickness or transmural = stemi or non-full thickness – non-stemi)
Q waves – pts font usually have them, but they appear in stemis
Non-stemi: Sub-endocardial MI – not full thickness – less damage overall to heart

describe the ST segment in ECGs (how to find it)
A = increase in T wave
C = elevation of ST segment (no longet at isoelectric point)
D = q-wave forms
E = t-wave comes down and becomes inverted
F = goes back to what it was originally (starts looking normal again – but Q wave remains)
The permanence of this Q-wave indicates this pesonhas had a STEMI
Note you can have a Q wave but if it is large enough, this is what is the sign
this is caused by dead tissue in the heart bc dead tissue doesn’t conduct and contract

what are cardiac biomarkers associated with MIs?
With cell death, these enxymes are released into the blood
Each enzyme has a specific rise and fall
Ck-MM = in the muscle
Ck-BB = in the brain
Troponin is used mostly now
The larger the troponin level measured, the larger the infarct

how to treat uncomplicated MIs
Will pts benefit from supplimental o2? Yes – it brings more o2 to heart (via blood)
Beta blockers decreases hr and decr contractility and therefore decr demand of heart
Channel blockers decr spasm, decr bp (afterload) and decr hr therefore decr demand to the heart

describe arrythmias as a MI complication
A fib or flutter greater than 120 have to be careful with
Bradycardia associated with symptoms, should be careful with
Symptoms = hypotension, loss of consciousness, and angna if it suddenly appears etc
Cardioversion = defibrillation (shocking the heart basically)
Last point – device senses arrhythmia and delivers shock when necessary

MI complications: describe heart failure
Systemic = right sided heart failure
Left = more conjestion in pulmonary vasculature
Could have problems with both if big enough problem
Tissue starts to stretch (image 3) and end up with reduced CO

what is the etiology of heart failure?
Cardiomyopathy = problem with the heart muscle
Systolic failure = heart cant out out the blood
Diastolic – heart can’t contract
When heart works really hard against afterload, it hypertrophies and starts to fail – thickens and decreases the size of the chambers in it (co reduced bc less filling of that failure) – eventually ventricle will fail
When Co low, not putting out enough blood – body compensates with stimulation of sympathetic N.S. (incr HR and contractility)
Incr vascular tone – clamps down on peripheral B.V.s
Kidney – trying to increase vascular volume, and maintain CO (compensatory strategy)

describe acute vs chronic heart failure
1 = coronary artery disease, MI, etc
2 = due to compensating mechanisms – takes longer

describe compensated vs uncompensated heart failure
Compensated – may have symptoms of heart failure when you stress the system – ie upon exercise etc
Uncompensated -

what are the signs and symptoms of heart failure?
Nocturnal dyspnia = bc volume incr venus return in supine heart unable to deal with this incr volume etc
Muscle cramping/weakness = bc of edema
Weight gain bc of fluid retention
Nocturia bc when pts supine, more blood flow to kidneys

new york heart association conjestive heart failure classifications


THR = total hip replacement
Typically when you go supine to standing, bp goes down and hr goes up – this pt hr cant go up bc of all the meds she is on
Congestive heart failure could be triggered during exercise – so symptoms related to heart failure
Irregular beats = due to the arrhythmia (maybe PVCs etc)
etiology/pathophysiology of R sided heart failure
- L sided heart failure can lead to R sided HF!!

etiology/pathophysiology of L sided heart failure
If you cant relax, blood cant go to heart and its gonna back up – EF can be normal or decreased depending on how much its able to relax
Cardiomyopothies – stretch of heart ms
Afterload – heart cannot contract against resistance

what is pericarditis?
Takes several weeks to occur
Scar is formed in the sac and this causes restiriction of the heart

etiology of pericarditis?
CAPG = Coronary artery bipass graphs
Systemic diseases = lupus or hypothyroidism

signs and symptoms of pericarditis?

medical treatment of pericarditis?
Colchicine = used for gout

what is a cardiac tamponade?
If there is a lot of fluid there!

etiology of valvular heart disease
Ie a thrombus to artery supplying the valves = valve problems
Some weight reducing drugs have caused this

describe valvular heart disease and stenosis
= increased resistance

describe valvular heart disease and insufficiency/regurgitation
Leaflets unable to stay closed and therefore regurgitation into atrium

describe valvular heart disease and prolapse
More common in mitral valve bc pressure in that side of heart is higher

s and s of valvular heart disease and what causes them?

what is myocarditis and the causes?
lammation of actual heart muscle

what are the signs and symptoms of myocarditis?
Red bullet 2 bc have some infection overall in heart

infective endocarditis: definition, etiology, and clinical presentation
Vegitations growing on valve

how to detect infective endocarditis and what is the treatment?
Can have a piece break off and cause a stroke etc
Pts - Typically need valve replacement
Vegitatins can break off etc

define cardiomyopathies and what is their classification?

etiology of cardiomyopathies?
dont memorize!

clinical presentation of cardiomyopathies?
JVD = jugular venus distension = indication of r sided failure (same with pitting edema)
Hepatomegaly = enlargement of liver

treatment of cardiomyopathies
Physical = exercise program
Surgical - may need heart transplant if severe


What is indicative of ruling out MI or acute problem = no bad troponin level, no angina (but may be silent MI), ecg just sinus tachy (no arrythmias), no risk factors (non smokers, no cardiac history, etc), he has signs of r sided heart failure (jugular distension and ankle edema)
indications for cardiac rehab?
2 = threshold changes for people with cardiac rehab exercises (studies)
3 = corony artery bypass graft
Denervation of the heard = careful exercise for those with heart transplant

contraindications for cardiac rehab?
1 = progressed slowly
6 = stenosis bc high resistance

exercise prescription wrt each of the phases in cardiac rehab?
Phase 1 = phase within the hospital – exercise should be performed more often in these pts
Phase 2 = 6 weeks to 6 months, doesn’t have to be done several times during the day, but intensity can be higher
Phase 3 = as intensity of exercise increases, don’t have to do it as much
phase 4 = more than 12 months

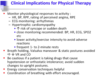
indications for stopping exercise/activities?
3 – symptonms = dizziness, ischemia, etc
Exercise should be 10 bmp lower than what would stimulate angina
St segment – why we need to monitor pts

clinical implications in PT for cardiac patients
3rd last point: don’t stop exercise abruptly, have cooldown!