Lecture 3: Afferent Visual System and Visual Fields Flashcards
Visual field is represented in the retina __ and __
- Upside down and reversed
- Superior field is represented by inferior retina
- Nasal field is represented by temporal retina

What is the approximate extent monocular VF?
Nasal
Superior
Inferior
Temporal
Temporal blind spot
- Nasal 60 degrees
- Superior 60 degrees
- Inferior 70-75 degrees
- Temporal 100-110 degrees
- Temporal blind spot (nasal optic nerve)

What is the extent of the binocular visual field
- approximately 180 degrees
- No blind spots!
- Stereo!

Interpreting the VF

- Place the fields side-by-side
- Place right field on your right
- You appreciate pt’s view point
- Interpret fields as a pair
- Look for normal blind spots
- Look for reliability
- Look for general depression
- Look for patterns!
- Pre-chiasmal vs. Post-chiasmal
List the 13 classification of VF loss?
- Density (severity)
- Relative: depressed sensitivity
- Absolute: no visual sensitivity
- Area
- Local-areas of the field are affected
- General - entire field affected
- Extent
- Total (total hemianopia)
- Partial (partial hemianopia)
- Macular sparing/splitting
- Shape
- Sectorial (hemianopic or quadrantanopic)
- Non sectorial (regular or irregular shaped)
- Type
- Scotomatous (enclosed seeing areas)
- Non-scotomatous
- Position
- Which quadrants are affected?
- Superior-nasal, or inferior-temporal
- Which quadrants are affected?
- Location
- Central
- Peripheral
- Size
- Large
- Small
- Laterality
- Unilateral or bilateral
- Homonymous, heteronymous
- Equalness
- Congruous
- similarity in defect between the 2 eyes
- Incongruous
- The defect is not similar between the 2 eyes
- Congruous
- Awareness
- Positive
- The pt is aware of the field loss
- Negative
- Cause
- Organic
- Functional
- Positive

Dividing the visual pathways into what 4 territories?

What is territory 1?
- Outer retina and choroid
- Monocular VF affected
- Not localized to a fiber bundle (horizontal midline)
- Does not respect the vertical midline
What is territory 2?
- Includes
- Ganglion cell layer
- NFL
- Optic nerve
- Corresponds to the distribution of the nerve fiber layer
- Defect appear above or below the midline.. think glaucoma
Schematic representation of the NFL


Describe the blood supply to the laminar optic nerve
- Retinal vasculature supplies
- Surface NFL
- Short Posterior Ciliary Arteries feed
- Circle of Zinn-Haller
- Which supplies:
- Pre-laminar ONH
- Laminar ONH
- Which supplies:
- Circle of Zinn-Haller
-
Acute obstruction of the branches of short posterior ciliary arteries that supply the
- Pre-laminar optic nerve
- Laminar optic nerve
- Cause disc edema
- Subsequent atrophy
- Common in elderly
- Anterior ischemic optic neuropathy (AION)
- Typical visual field loss is altitudinal
- Cause disc edema

What occurs if there stasis of axoplasmic flow?

Study the image

Study the image

What does this image show?

Papilledema
Describe orbital optic nerve
- Describes nerve from globe to optic foramen
- 20 mm long
- Redundant to accommodate mvmt
- Diameter of the nerve doubles
- Myelin sheath
- Papillo-macular fibers migrate into the center of the nerve
- Superior and inferior fiber fill the space left by papillo-macular fibers
Retrobulbar optic nerve
- Location of the retinal nerve fiber bundles within the retrobulbar nerve

Describe optic nerve disease and VF loss
- Glaucoma
- Paracentral, arcuate, nasal step, temporal wedge
- AION
- Segmental, usu inferior altitudinal
- Optic neuritis
- Macular fibers primarily affected - central or centrocecal scotomas, arcuate defects
- Toxic/Nutritional and Hereditary
- Central and centrocecal
- Inflammation behind the globe
- Retrobulbar
- Pt sees nothing and the doctor sees nothing
- Compressive masses
- Nerve fiber defects breaking through into the periphery
- Most common optic nerve retrobulbar masses are gliomas and meningiomas
- Intra-orbital tumors cause non-pulsatile proptosis
intracanalicular portion is accompanied by…? (3)
- Enters the optic canal at the apex of the orbit
- Optic nerve (CN II) is within optic canal
- Accompanied only by
- Ophthalmic artery
- Meningeal sheaths of the optic nerve
- Sympathetic twigs

Describe the middle cranial activity? What is adjacent to it?
- Enters the middle cranial cavity
- Adjacent to its the superior orbital fissure
- Superior orbital fissure brings
- CN III
- CN IV
- CN VI
- CN V1
- Ophthalmic vein to and from globe
- MR, LR and SR muscles can experience pain from inflammation in this area
- Mass lesion in this area leads to multiple neurological issues
- Superior orbital fissure brings
Describe the intracranial optic nerve
- Extends from optic canal to chiasm
- 10 mm long
- Frontal lobes are located superiorly
- Internal carotids are located laterally
Describe intracranial optic nerve tumors
- Optic nerve gliomas and meningiomas
- In this region and if large enough may disturb hypothalamic and pituitary function
- Meningiomas originate from optic nerve sheath arachnoid cap cells
- Gliomas are slow growing pilocytic astrocytic neoplasms associated with neurofibromatosis
- Usu benign but can transform into malignancy
- Larger tumors are disruptive due to mass effect

Intracranial optic nerve lesions affect __ field
one

Describe (4) frontal cortex lesions
- Left cortex
- Broca’s aphasia
- difficulty with speech
- Understand speech well
- Upper motor neuron motor weakness
- Contralateral
- Depends on homunculus
- Frontal eye fields affected
- If irriated: looks away from the side with the lesion
- If destroyed: looks toward the side with the lesion
- Personality and behavior abnormalities
- Broca’s aphasia

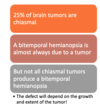
Describe territory 3: optic chiasm
- The optic nerves project backwards and upwards
- The optic nerves converge and meet over the sella turcica