Lec 5- IV infusion Flashcards
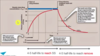
IV bolus / infusion
-
IV bolus dose
- When repeated doses are required or when you need to maintain drug concentrations in the patients, it’s not a very convenient approach
- Lots of sub-therapeutic time, small amount of therapeutic time
-
IV infusion
- Used within hospitals to provide a constant level of therapy to an individual
- Allows control and maintenance of plasma concentrations and is a precise and controlled systems
- Drug infusion can be stopped if there are adverse problems

STEADY STATE ACCUMULATION
- IV infusions balance the INFUSION RATE (going in) with the CLEARANCE of the drug (going out)
- When this is the balance you reach steady plasma concentrations and this is called steady state

IV infusion- background
- Our goal: to achieve a STEADY STATE concentration
- How long: 4-5 half-lives to reach STEADY STATE for every drug
- NB- Although counterintuitive, the half-life here refers to the elimination half-life
- NB-To reaches SS you need to infuse the drug for 4-5 half-lives to reach SS. The half-life is a function of each drug to the infusion time varies for each drug

IV infusion
- Assume you have started the infusion and what to know the concentration at ANY point during the infusion
- You would have a Css and you should know some information about the elimination (k) of your drug
- We can use the following equation to follow what is happening to the drug DURING the infusion

What type of drugs do you think are REQUIRED to be given by infusion?
- General anaesthetics
- Insulin pump (diabetic)
- Pain relieve- morphine infusion
- Narrow TI drugs (phenytoin, warfarin)
- Chemotherapy
- Antibiotics
Case study 1: Steady state concentrations

- If the infusion rate and dose are the same as before, why has the Css (steady state concentration) increased?
- Infusion rate- easy to manipulate
- CL of the drug- difficult to manipulate- in this example there is a change in elimination
- Time for drug to reach 0 is longer
- Can you estimate the half-life of this drug without doing any difficult maths?
- 2 hours to reach SS, it takes 4-5 half-lives to reach SS, therefore, we can estimate 0.4-0.5 Hrs

Case study 2: loading doses
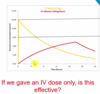
- In many clinical situations, we require rapid clinical onset
- In these cases we often LOAD the patient with a high dose of the drug, to begin with- this is called the LOADING DOSE
- This approach pre-loads the patients with the clinically active dose
- If we gave an IV dose only, is this effective?
- By pre-loading with a loading dose following by the maintenance (IV infusion) we achieve the profile above

Case study 2
Steady-state concentrations
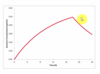
- What are your thoughts on this therapy
- Assume the target concentration is 6ng/mL
- This is poor because you need to infuse for 18 hrs and you still haven’t reached therapeutic window, so doesn’t have much effect
- This is caused by the fact the drug has a long half life
If you know the target Css if 6-10 ng/mL, how would you work out an appropriate loading dose
- The loading dose is an IV-bolus dose. We can USE
- Css = LD/Vd
- It can also be calculated by looking at
- LD = R<em>inf</em> / kel
- The choice depends on which type of information you have availability in the clinical situation
Case study 3: post infusion
- The graph opposite is a computer-generated profile where the red line is made up of hundreds of data points which represent hundreds of blood samples in one patient over the 24 hours
- This is not reflective of the clinical environment
- In some cases, we only have a few blood samples from a patient and may wish to calculate important PK of the drug
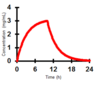
How can we work out the half-life of the drug in this patient
(Assume we didn’t know that 3 hours was Css)

- When we STOP the infusion it is the same as when we give a patient and IV-bolus dose at the exact moment
- The infusion is giving drug into the venous circulation and when we stop the infusion the only thing controlling the drug is it’s loss from the body
Case study 3: Post infusion
We can use the first order equation
- Ct=C0e-kt
- And assume C0 is actually Css
- You can then treat calculate the slope of an LN vs time
- OR Semi-log vs time graph to determine t1/2
- OR this can be done visually
- Treat as an IV bolus dose example
IV infusions: Changing parameter
- Mrs Smith has been admitted into a hospital ward
- She attends regular visits to be administered regular IV-infusions
- On the second visit to the clinical, she is now not clinically responding to her standard infusion setup
- Assuming that the rate of infusion and dose has not changed between the 2 visits, what has caused this change?
- Concentration
- CL
- Half-life has changed
IV infusion: changing parameters
- Css has decreased
- If the infusion rate hasn’t changed then this is a result of an increase in the clearance
- It was discovered that this patient was suffering from a DDI which enhanced the clearance of the infused drug, perhaps from a newly prescribed medication
- Drug-drug interactions, liver, kidney
- Css = Rinf / CL

Case study 5: full example
- A patient was given an IV infusion of drug X. The infusion was prepared by the addition of 5mL of a 25mg/mL solution of drug X to a 495mL of 0.9% w/v saline. The giving set was adjusted to deliver 40mL/h and this solution was infused for 10 hours
- Calculate the following parameter
- The dose the patient received
- The plasma concentration of the drug at the end of the infusion
- Elimination half-life
- Elimination rate constant
- Total body clearance of the drug
- A volume of distribution of the drug
- The steady state concentration that would have been achieved if the infusion had continued
IV infusions
- 5mL of 25mg/mL solution = 5*25mg of drug =125mg of drug
- Total volume= 495 + 5 = 500mL
- Overall concentration = 125mg/500mL = 0.25mg/mL
- Delivered at 40mL per hour for 10 hours
- Total volume = 400mL
- Total dose = 400*0.25 = 100mg
IV infusion
Calculated from graph, Estimated from data table
- Time is taken for 50% reductions in drug concentrations
- A more accurate way is to calculate the elimination rate constant (gradient) then convert to half-life

IV infusion calculation: Elimination rate constant
- k = ln2/ t1/2
- k= 0.17 h-1
- Remember, units for a rate constant are time-1 and units for half-life are time
IV infusion calculation- Total body clearance of the drug
- The concentration did not reach steady state, therefore, we cannot use
- Css = Rinf/CL
- You need to use an alternative method
- The relevance of this term is the discussion more in later lectures
IV infusions calculation
Area under the curve
- AUC- represents the residency of the drug in the body and is used to calculate the bioavailability
- It is also very useful in calculating the clearance of the drug, it is just the area under the curve
- AUC = Dose/ Clearance Units: mg.mL.hour
- By knowing the DOSE (see earlier) and AUC, we can calculate the CLEARANCE of the drug
IV infusion calculations- Volume of distribution
- Cl = k.Vd
- As CL and k are known we can calculate Vd
- Vd= 20.7 / 0.17
- Vd= 121 Litres
IV infusion calculation
The steady state concentration that would have been achieved if the infusion had continued
- Ct-inf = Css (1 - e-kt)
- Select a random time point, I’ve chosen 1 hour
- Using data point t=1; Ct-inf = 0.077
- 0.077 = Css (1-e-0.17*1)
- 0.077 = Css (1-0.84)
- Css = 0.077/(1-0.84)
- Css = 0.48 mg/L
- We have been give time and concentration and we have calculated k


