L19-20: Cervical muscle and sensorimotor treatment Flashcards
(38 cards)
What are 7 impairments in muscle function in neck pain?
- Altered relationships within
- neck flexor synergy
- neck extensor synergy (probable)
- axioscapular muscles
- Loss of feedforward response
- Muscles are delayed (acting in feedback pattern–> more risk of injury)
- Morphological changes
- Loss of muscle support in posture and movement
- Loss of endurance at different contraction intensities
- Loss of strength/ endurance
- Fatigability
What are 5 exercise mode(s) best for neck pain disorders?
- Motor relearning
- Flexibility training
- Endurance training
- Strength training
- Cardiovascular training
All beneficial for pain management: Depends on primary outcome
What are 2 exercises if pain is the primary outcome for neck pain disorders?
Evidence:
- both motor learning
- strength training
What are exercises if prevention/prevention of recurrent neck pain is the primary outcome?
Suggest exercise must restore normal muscle behaviour and function
What type of exercise should be prescribed?

What are 5 outcomes tested in motor relearning and strength training?
- CCFT
- Functional tasks
- Posture
- Feedforward
- Strength/ fatigue of the SCM and AS
What is the ouctome of CCFT for strength training?
Strength Training ✖
General head lift exercise failed to address altered muscle behaviour
Strength training did not improve in CCF (therefore must target management)

What is the ouctome of CCFT for motor relearning?
Motor relearning ✔
Specific low load exercise successfully addressed altered muscle behaviour
Both deep and superficial muscles improved with CCF low load training (motor control)

What is the variations between individuals (idiopathic neck pain) in initial presentation related to pain intensity?
High levels of pain = less effect of training (might take longer)

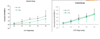
What is the relationship between change in pain and magnitude of improvement in deep cervical flexor activation after training?
Once deep flexors are changed –> some changes are seen

What are 2 ways that very high pain states can affect motor relearning?
- Chronic WAD- No change SCM activity in CCFT after 10 weeks training
- in higher NDI and widespread mechanical and cold hyperalgesia
- No sensory change threshold (cold..etc) = improved better
- Sensory changes = less improvements

What is outcome for the functional task (tapping task)? What does does the outcome mean?
- no significant change activity post-intervention for either exercise group✖
- Similar results trapezius ✖
Suggests task specificity is also required in training
- Eg. scapular while adding functional task
What is the outcome of posture change? What does does the outcome mean?
Change in cervical angle during the computer task in response to training?
- motor relearning program ✔
- strengthening program ✖
To postures (since they are low load endurance muscles)

What is the outcome of feed forward? What does does the outcome mean?
Improved timing of the deep cervical flexors motor learning program better

What is the outcome of strength? What does does the outcome mean?
Higher load exercise required to improve strength

What is the outcome of fatiguability? What does does the outcome mean?
Higher load exercise required to improve SCM and AS fatigability

What are 2 types of tasks?
- Formal
- Functional –task specific
What are 5 tasks for muscle system in neck pain disorders?
- Some evidence that improvements following exercise translate to improvements in automatic function of the cervical muscles
- Similar changes observed with specific training of the deep trunk muscles (TrA)
- Better response to low load craniocervical flexion training which emphases a motor learning approach
- More work to be done on dose of training
- Specific training of the DCF is associated with improvements in control of working posture
What are 4 ways to correct postures?
- Higher neck extensor muscle activity in slumped posture
- Comparison of correction with thoracic extension versus lumbopelvic neutral technique
- Both Th Ext and L/P correction → more neutral head neck posture (but thoracic extension → high thoracic erector spinae activity)
- Neither changed activity in the upper trapezius (ie scapular posture)**
What is the study: request to sit up straight versus facilitation of neutral upright posture?
Higher activation levels in DCF and lumbar multifidus
- Facilitation (activating muscles) is more effective then instructing to sit up

Does task specific exercise help muscle control?
- Conscious elongation of cervical spine facilitates longus colli
- Outcome of CCFT after two weeks of training with posture correction with ‘occipital lift’ (not retraction)
- Most effective for activating CCF
Can exercise assist fatty infiltrate extensors ?
- Current data suggests that fat index can be changed with exercise
- Further development of measure
Does therapeutic exercise- change pain?
- RCT cervicogenic headache
- RCT in the management of chronic whiplash
What are 4 characteristics of scapular retraining?
- Motor control perspective: can change pattern of activation the three portions of trapezius with a scapular postural correction exercise
- Can address control, strength and endurance of axio-scapular muscles with specific exercise (evidence in shoulder disorders)
- Case studies neck pain - efficacy of treating scapular dysfunction
- No RCTs as yet looking uniquely at the effect of re-educating scapular in neck pain





