Immunology Flashcards
What is immunopathology?
Damage to the host cause by the immune response

What are autoimmune or autoinflammatory diseases?
Immunopathology in the absence of infection
Innate IR -> autoinflammatory
- Local factors at sites predisposed to disease lead to activation of innate immune cells such as macrophages and neutrophils, with resulting tissue damage
Mixed innate/adaptive -> mixed
Adaptive IR -> autoimmune
- Aberrant T cell and B cell responses in primary and secondary lymphoid organs lead to breaking of tolerance with development of immune reactivity towards self-antigens
- Adaptive immune response plays the
- predominant role in clinical expression of disease
- Organ-specific antibodies may predate clinical
- disease by years

What are the rare monogenic autoinflammatory disease?
Mutations in a gene encoding a protein involved in a pathway associated with innate immune cell function
Abnormal signalling via key cytokine pathways involving TNF and/or IL-1 is common
Familial Mediterranean fever is the more common one out of these
MEFV – loss of function mutation, which encodes pyrin marenostrin which is a negative regulator of the ASC – procaspase 1 inflammatory process; so increases inflammation

What is the inflammasome complex and its role in FMF?
Mechanism of pathogenesis in Familial mediterranean fever:
- Autosomal recessive condition
- Mutation in MEFV gene
- Gene encodes pyrin-marenostrin
- Pyrin-marenostrin expressed mainly in neutrophils
- Failure to regulate cryopyrin driven activation of neutrophils

What is FMF?
Pathogenesis
- Autosomal recessive condition
- Mutation in MEFV gene
- Gene encodes pyrin-marenostrin
- Pyrin-marenostrin expressed mainly in neutrophils
- Failure to regulate cryopyrin driven activation of neutrophils
Clinical presentation
- Periodic fevers lasting 48-96 hours associated with:
- Abdominal pain due to peritonitis
- Chest pain due to pleurisy and pericarditis
- Arthritis
- Rash
Amyloid risk:
- Long term risk of AA amyloidosis
- Liver produces serum amyloid A as acute phase protein
- Serum amyloid A deposits in kidneys, liver, spleen
- Deposition in kidney often most clinically important
- Proteinuria - nephrotic syndrome
- Renal failure
Treatment:
- Colchicine 500ug bd - binds to tubulin in neutrophils and disrupts neutrophil functions including migration and chemokine secretion; hence why it also works for gout
- Anakinra (Interleukin 1 receptor antagonist)
- Etanercept (TNF alpha inhibitor)
What are monogenic autoimmune diseases?
Mutation in a gene encoding a protein involved in a pathway associated with adaptive immune cell function
- Abnormality in tolerance – APS-1 /APECED
- Abnormality of regulatory T cells - IPEX
- Abnormality of lymphocyte apoptosis - ALPS
What is APS1 and APECED?
Monogenic Auto-immune Disease
- Auto-immune polyendocrine syndrome type 1 (APS1)
- Auto-immune polyendocrinopathy-candidiasis-ectodermal dystrophy syndrome / APECED
Pathology:
- Autosomal recessive disorder
- Defect in ‘auto-immune regulator’ – AIRE
- Transcription factor involved in development of T cell tolerance in the thymus
- Upregulates expression of self-antigens by thymic cells
- Promotes T cell apoptosis
- Transcription factor involved in development of T cell tolerance in the thymus
- Defect in AIRE leads to failure of central tolerance
- Autoreactive T cells
- Autoreactive B cells
- aspect of B cell tolerance is T cell dependent
- limited repertoire of autoreactive B cells
Clinical presentation:
- Multiple auto-immune diseases
- Hypoparathyroidism
- Addisons
- Hypothyroidism
- Diabetes
- Vitiligo
- Enteropathy
- Antibodies vs IL17 and IL22
- Candidiasis
What is IPEX?
Monogenic Auto-immune Disease
- Immune dysregulation, polyendocrinopathy, enteropathy, X- linked syndrome
Mutations in Foxp3 (Forkhead box p3) which is required for development of Treg cells
- Failure to negatively regulate T cell responses
- Autoreactive B cells
- limited repertoire of autoreactive B cells
- Autoreactive B cells
- Ipex08 – no foxp3 positive, endocrine primarily, with eczema type disease and peripheral t cell tolerance
Clinical presentation:
- Autoimmune diseases
- Diabetes Mellitus
- Hypothyroidism
- Enteropathy
- ‘Diarrhoea, diabetes and dermatitis’
What is ALPS?
Monogenic Auto-immune Disease
- Auto-immune lymphoproliferative syndrome
Pathogenesis
- Mutations within FAS pathway
- Eg mutations in TNFRSF6 which encodes FAS
- Disease is heterogeneous depending on the mutation
- Defect in apoptosis of lymphocytes
- Failure of tolerance
- Failure of lymphocyte ‘homeostasis’
Clinical presentation:
- High lymphocyte numbers with large spleen and lymph nodes
- double negative (CD4-CD8-) T cells
- Auto-immune disease
- commonly auto-immune cytopenias
- Lymphoma
What are polygenic autoinflammatory diseases?
Mutations in genes encoding proteins involved in pathways associated with innate immune cell function
Local factors at sites predisposed to disease lead to activation of innate immune cells such as macrophages and neutrophils, with resulting tissue damage
HLA associations are usually less strong
In general these disease are not characterised by presence of auto-antibodies
What is IBD?
Polygenic autoinflammatory disease
- Genetic polymorphisms
- Familial association studies and twin studies suggested genetic predisposition to disease
- 15% patients have an affected family member
- 50% vs <10% disease concordance in monozygotic vs dizygotic twins
- >200 disease susceptibility loci found
- IBD1 gene on chromosome 16 identified as NOD2 (CARD-15, caspase activating recruitment domain -15).
- Three different mutations of this gene have each been shown to be associated with Crohn’s disease.
- NOD2 gene mutations are present in 30% patients (ie not necessary)
- Abnormal allele of NOD2 increases risk of Crohn’s disease by 1.5-3x if one copy and 14-44x if two copies (ie not sufficient)
- NOD2 expressed in cytoplasm of myeloid cells - macrophages, neutrophils, dendritic cells
- Intracellular receptor for bacterial products - recognises muramyl dipeptide – and stimulates NFKb
- Activation induces autophagy (orderly degradation of cellular components) in dendritic cells
- Mutations also found in patients with Blau syndrome and some forms of sarcoidosis
Crohn’s disease:
Clinical features
- Abdominal pain and tenderness
- Diarrhoea (blood, pus, mucous)
- Fevers, malaise
Treatment
- Corticosteroid
- Anti-TNF alpha antibody

What are mixed pattern diseases?
Mutations in genes encoding proteins involved in pathways associated with innate immune cell function
And
Mutations in genes encoding proteins involved in pathways associated with adaptive immune cell function
HLA associations may be present
Auto-antibodies are not usually a feature
What is ankylosing spondylitis?
Mixed pattern diseases
Genetic polymorphisms – heritability >90%
Enhanced inflammation occurs at specific sites where there are high tensile forces (entheses - sites of insertions of ligaments or tendons)
Presentation
- Low back pain and stiffness
- Enthesitis
- Large joint arthritis
Treatment
- Non-steroidal anti-inflammatory drugs
- Immunosuppression
- Anti-TNF alpha – usually works very well, but if not can use:
- Anti-IL17

What are polygenic autoimmune diseases?
- Mutations in genes encoding proteins involved in pathways associated with adaptive immune cell function
- HLA associations are common
- HLA presentation of antigen is required for development of T cell and T cell-dependent B cell responses
- Aberrant B cell and T cell responses in primary and secondary lymphoid organs lead to breaking of tolerance with development of immune reactivity towards self-antigens
- Auto-antibodies are found
Pathogenesis:
- Genetic polymorphisms -> loss of tolerance -> auto-reactive T cells (which can affect) auto antibody formation -> immunopathology -> disease
- Environmental factors can affect loss of tolerance, the formation of auto ab and immunopathology

What are the genetic polymorphisms in polygenic autoimmune disease which lead to T cell activation?

What is the Gel and Coombs classification?
Gel and Coombs effector mechanisms of immunopathology
- •Gel and Coombs (1960s) classified skin test ‘hypersensitivity’ reactions according to the type of immune response observed
- •Antibody or T cell mediated
- •Effector mechanisms for immunopathology
Classification:
- •Type I: Immediate hypersensitivity which is IgE mediated
- •Type II: Antibody reacts with cellular antigen
- Ab binds to cell associated Ag
- Ab dependent destruction:
- NK cells -> Ig Fc receptor binds onto Ab which causes release of cytolytic granules and membrane attack
- Phagocytes -> Phagocyte binds to the Ab and the cell is phagocytosed
- Complement -> Complement is activated - classical pathway C1,2,4 which activates C3 and then final common pathway C5-9 forms the membrane attack complex and causes Cell lysis
- Receptor activation or blockade
- •Type III: Antibody reacts with soluble antigen to form an immune complex
- Immune complex driven autoimmune disease -> Ab binds to soluble antigen to form circulating immune complex
- Immune complex formation and deposition in blood vessels
- Complement activation and infiltration of macrophages and neutrophils
- cytokine and chemokine expression, granule release fromm neutrophils and increased vascular permeability
- inflammation and damage to vessels -> cutaenous vasculitis, glomerulonephritis, arthirits
- •Type IV: Delayed type hypersensitivity, T-cell mediated response
- HLA class I molecules present Ag to CD8 T cells, onto the TCR-CD3 and CD8 receptors; causes cytolytic granule release from primed T cell -> cell lysis occurs
- HLA Class II molecules present Ag to CD4 T cells to the CD4 TCR-CD3 receptor, with interaction between the CD80/86 on APC and the CD28 on Th1; then primed Th1 cell releases IFN-g, signalling to macrophage to cause TNF induction, lymphotoxin and HLA upregulation which leads to inflammation and tissue damage

What are the examples of type II antibody driven autoimmune diseases?

What are examples of Type III immune complex driven autoimmune diseases?

What are examples of type IV t-cell mediated diseases?

What are the 2 types of polygenic auto-immune diseases?

What is Graves disease?
Clinical presentation
- •Nervous
- •Palpitations
- •Heat intolerant
- •Diarrhoea
Pathogenesis:
- •Excessive production of thyroid hormones
- •Mediated by IgG antibodies which stimulate the TSH receptor
- –Evidence
- •Antibodies stimulate thyrocytes in vitro
- •Passive transfer of IgG from patients to rats often produces similar symptoms (!)
- •Babies born to mothers with Graves’ may show transient hyperthyroidism
- •Stimulating autoantibodies against TSH-receptor bind to receptor
- •Act as TSH agonists
- •Induce uncontrolled overproduction of thyroid hormones
- •Negative feedback cannot override antibody stimulation
What is Hashimoto’s thyroiditis?
Clinical presentation:
- •Lethargic
- •Dry skin and hair
- •Constipation
- •Cold intolerant
- Commonest cause of hypothyroidism in iodine-replete areas
- Goitre – enlarged thyroid infiltrated by T and B cells
- Associated with anti-thyroid peroxidase antibodies
- –Presence correlates with thyroid damage and lymphocyte inflammation
- –Some shown to induce damage to thyrocytes
•Associated with presence of anti-thyroglobulin antibodies
But measuring these antibodies might not be useful:
- Many women >65 have anti-thyroid abs
- some postmenopausal women with anti-thyroid ab have subclinical hypothyroidism
- small proportion of postmenopausal women with anti-thyroid ab have overt hypothyroidism
- Few indications for testing for these thyroid antibodies because high prevalence in normal individuals. Just do thyroid biochemistry
What is T1DM?
Clinical presentation:
- •Thirsty
- •Polyuria
- •Malaise
- •Urine dipstick confirms glycosuria
- •Insulin dependent diabetes mellitus
Non obese diabetes (NOD) mouse model for type 1 diabetes
- CD8+ T-cell infiltration of pancreas
- T cell clones have specificity for islet antigens
- Progressive increase in lymphocyte infiltration and islet destruction in the non-obese diabetic (NOD) mouse
Antibodies pre-date development of disease
- Anti-islet cell antibodies
- Anti-insulin antibodies
- Anti-GAD antibodies
- Anti-IA-2 antibodies
- May be secondary to islet cell destruction
- Individuals with 3-4 of the above are highly likely to develop type I diabetes
- Detection of antibodies does not currently play a role in diagnosis

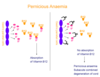
What is pernicious anaemia?
Clinical presentation
- •Tired
- •Pale
- •Mild numbness of feet
- Anaemic Hb 8.4
- Macrocytosis MCV 108
- Urine dipstick –ve
- Folate normal
- Vitamin B12 very low
Need to think about whether they are actually vit b12 deficient or because they can’t absorb it
- Failure of vitamin B12 absorption
- Vitamin B12 deficiency
- Macrocytic anaemia
- Neurological features with subacute combined degeneration of cord (posterior and lateral columns), peripheral neuropathy, optic neuropathy
- Antibodies to gastric parietal cells or intrinsic factor - are useful in diagnosis
What is myasthenia gravis?

Clinical presentation:
- •Drooping eyelids
- •Weakness, particularly on repetitive activity
- •Symptoms worse at end of day
Anti-acetylcholine receptor antibodies present in ~75% patients and are useful in diagnosis
Offspring of affected mothers may experience transient neonatal myaesthenia

Case:
- •48 year old man
- •Haemoptysis with widespread crackles in lungs
- •Swelling of legs
- •Reduced urine output
- •Creatinine 472
- •Microscopic haematuria and proteinuria
- •CXR – widespread shadowing
- •Elevated TLCO (gas transfer factor) suggesting pulmonary haemorrhage
Ijnvestigations:
- •Anti-basement membrane antibody positive
- •Crescentic nephritis on biopsy
- •Antibodies specific for glomerular basement membrane disease underpin the pathology and are useful in diagnosis of anti-glomerular basement membrane disease (Goodpasture’s disease)
- Circulating antibodies specific for GBM are useful in diagnosis
- Also important in pathogenesis (Type II)
Pt has Goodpasture’s
Detection of auto-ab in kidneys:
- Fluorescein conjugated polyclonal anti-human immunoglobulin, need a UV source, fluorescence microscope
- Smooth linear deposition of antibody along the glomerular basement membrane
- Type II hypersensitivity
- Antibodies may also be detected in tissue sections.
- Antibodies have been deposited along the basement membrane to give ‘smooth linear staining’ visible when the secondary fluorescein conjugated anti-human immunoglobuline is added.
What is Rheumatoid arthritis?
Clinical presentation:
- •Pain, stiffness and swelling of multiple small joints within hands
- •Normochromic anaemia
- •High ESR and CRP
Genetic predisposition
- •HLA DR4 (DRB1 0401, 0404, 0405) and HLA DR1 (DRB1 0101) alleles
- •Susceptible alleles share a sequence at positions 70-74 of the HLA DR beta chain
- •These alleles may bind ‘arthritogenic peptides’ and have been shown to bind to citrullinated peptides with high affinity
- •Peptidyl arginine diminase (PAD)2 and PAD4 polymorphisms
- Peptidylarginine deiminases PAD type 2 and 4
- Enzymes involved in deimination of arginine to create citrulline
- Polymorphisms are associated with increased citrullination
- This creates a high load of citrullinated proteins
- •PTPN22 polymorphism (activates T cells if abnormality)
Environmental factors:
- •Smoking associated with development of erosive disease
- –Smoking associated with increased citrullination
- •Gum infection with Porphyromonas gingivalis associated with rheumatoid arthritis
- –P gingivalis is only bacterium known to express PAD enzyme and thus promote citrullination
Antibodies:
- •Antibodies to cyclic citrullinated peptide
- –Bind to peptides in which arginine has been converted to citrulline by peptidylarginine deiminase (PAD)
- –Around 95% specificity for diagnosis of rheumatoid arthritis
- –Around 60-70% sensitivity for diagnosis of rheumatoid arthritis
- •A rheumatoid factor is an antibody directed against the common (Fc) region of human IgG
- •IgM anti-IgG antibody is most commonly tested although IgA and IgG rheumatoid factors may also be present in some individuals
- •Around 60-70% specificity and sensitivity for diagnosis of rheumatoid arthritis
What are ANA?
Anti-nulcear antibodies
- Group of antibodies that bind to nuclear proteins
- Test by staining of Hep-2 cells (human epidermoid cancer line)
- Very common
- –Low titre antibodies (<1:80) often found in normal individuals (esp older women)

What is SLE?
Clinical presentation:
- –4 month history of fatigue
- –Generalised arthralgia, particularly of small joints of hands
- –Hair fall
- –Mouth ulcers
- –Butterfly rash
Genetic predisposition:
- Abnormalities in clearance of apoptotic cells
- –Polymyorphisms in genes encoding complement, MBL, CRP – increase load of dying and dead cell
- Abnormalities in cellular activation
- Polymorphisms in genes encoding/controlling expression of cytokines, chemokines, co-stimulatory molecules, intracellular signalling molecules; CTLA4 mutation
- B cell hyperactivity and loss of b cell tolerance
- All lead to:
- Antibodies directed particularly at intracellular proteins
- ? Debris from apoptotic cells that have not been cleared
- Nuclear antigens - DNA, histones, snRNP
- Cytoplasmic antigens - Ribosome, scRNP
- Antibodies directed particularly at intracellular proteins
Pathogenesis:
- •Antibodies bind to antigen to form immune complexes
- •Immune complexes deposit in tissues
- –Skin, joints, kidney
- •Immune complexes activate complement (classical pathway)
- •Immune complexes stimulate cells expressing Fc and complement receptors
Immunological tests:
- ANA levels, normal <1:80;
- •Measured by titre (the minimal dilution at which the antibody can be detected) or by concentration in standardised units -> the higher the dilution, the higher the number of antibodies
- Other Ab;
- ANA
- •Homogeneous staining associated with specificity for dsDNA
- •Confirmation of specificity with ELISA
- dsDNA
- •Measures antibodies against double stranded DNA
- –Are highly specific for SLE (95%)
- –Occur in ~60-70% of SLE patients at some time in their disease
- –Very high titres are often associated with more severe disease, including renal or central nervous system involvement.
- –Useful in disease monitoring
- •an increase in antibody titre is associated with disease activity and may precede disease relapse.
- •False positive results unusual (<3%)
- •Measures antibodies against double stranded DNA
- Ro, La, Sm, U1RNP (ribonucleoproteins)
- •Speckled antibody
- •Associated with antibodies to extractable nuclear antigens
- •Specificity is for some ribonucleoproteins (Ro, La, Sm, U1RNP) – confirm with ELISA
- Anti-ENA ab
- •Ro, La, Sm, RNP (all are ribonucleoproteins)
- –Antibodies may occur in SLE
- –Anti-Ro and La are also characteristically found in Sjogren’s syndrome
- –Titres not helpful in monitoring disease activity
- •Speckled antibody
- SCL70 (topoisomerase)
- Centromere
Other tests:
Complement
- •Formation of antibody-antigen immune complexes
- –activate complement cascade via classical pathway (C1,4,2)
- –complement components become depleted if constantly consumed
- •Quantitation of C3 and C4 acts as a surrogate marker of disease activity
- [NB we measure UNACTIVATED complement proteins, not activated forms]
- Inactive disease: C3 is normal, C4 is normal
- Active disease: C3 is normal, C4 is depleted
- Severe active disease: C3 and C4 are depleted
•Anti-phospholipid syndrome
- –Recurrent venous or arterial thrombosis (check Ab in young men/women which get these)
- –Recurrent miscarriage – mainly 2nd trimester
- –May occur alone (primary) or in conjunction with autoimmune disease (secondary)
- •Two major types of antibody tests
- –Anti-cardiolipin antibody
- •immunoglobulins directed against phospholipids, and β2 glycoprotein-1
- –Lupus anti-coagulant
- •Prolongation of phospholipid-dependent coagulation tests – looked at in isolation
- •cannot be assessed if the patient is on anticoagulant therapy
- •Looks at the prolonged clotting time and adds phospholipid to help it clot – but in vivo these patients have high clotting risk
- Note that 40% of patients have discordant antibodies
- If there is a clinical suspicion of the antiphospholipid syndrome, both tests should be performed.
- –Anti-cardiolipin antibody
What is systemic sclerosis?
•Limited Cutaneous Systemic Sclerosis (CREST)
- Skin involvement does not progress beyond forearms, or lower leg and feet (although it may involve peri-oral skin)
- –Calcinosis
- –Raynauds
- –Oesophageal dysmotility
- –Sclerodactyly
- –Telangectasia
- –Primary pulmonary hypertension – most severe, need to monitor this very closely
•Diffuse Cutaneous Systemic Sclerosis
- Skin involvement does progress beyond forearms
- CREST features
- More extensive gastrointestinal disease
- Interstitial pulmonary disease
- Scleroderma kidney (vascular, endothelial cells prolif, lumen gets small and decreased blood flow to kidneys) / present with hypertensive renal crisis
ANA is prognostic indicator for SS
- Diffuse:
- Nucleolar pattern
- Anti-topoisomerase antibodies (Scl70)
- RNA polymerase
- Fibrillarin
- Limited:
- Anti-centromere Ab
What is idiopathic inflammatory myopathy?
Clinical presentation:
- Weakness
- Malaise
- Rash
•Dermatomyositis
- •Within muscle – perivascular CD4 T cells and B cells
- •Immune complex mediated vasculitis
•Polymositis
- •Within muscle – CD8 T cells surround HLA Class I expressing myofibres
- •CD8 T cells kill myofibres via perforin / granzymes
Investigations:
- •Positive ANA (in some patients)
- – extended myositis panel
- Anti-aminoacyl transfer RNA synthetase antibody eg Jo-1 (cytoplasmic) important!
- Anti-signal recognition peptide antibody (nuclear and cytoplasmic) (PM)
- Anti-Mi2 (nuclear) (DM>PM)
How do we investigate connective tissue diseases?

What are the different systemic vasculitis?
Small vessel vasculitis associated with ANCA – 3 types
Microscopic polyangiitis / Microscopic polyarteritis / MPA
Granulomatosis with polyangiitis / Wegener’s granulomatosis / GPA
Eosinophilic granulomatosis with polyangiitis / Churg-Strauss syndrome / eGPA

What is ANCA?
ANCA:
- Antibodies specific for antigens located in primary granules within cytoplasm of neutrophils
- Inflammation may lead to expression of these antigens on cell surface of neutrophils
- Antibody engagement with cell surface antigens may lead to neutrophil activation (type II hypersensitivity)
- Activated neutrophils interact with endothelial cells causing damage to vessels - vasculitis
•cANCA
- –Cytoplasmic fluorescence
- –Associated with antibodies to enzyme proteinase 3
- –Occurs in > 90% of patients with granulomatous polyangiitis with renal involvement – Wegner’s
p-ANCA
- Perinuclear staining pattern
- Associated with antibodies to myeloperoxidase
- Less sensitive and specific than cANCA
- Associated with microscopic polyangiitis and eosinophilic granulomatous polyangiitis (churg-strauss)
What is HIV 1?
Retrovirus
- Genes composed of RNA molecules.
- Replicates inside cells using an enzyme called Reverse Transcriptase (RT) to convert RNA into DNA which can be integrated into host cell’s genes.
- Primarily infects immune system cells causing immunodeficiency and AIDS.
Organisation of the virion:
- Retrovirus with CD4+ T helper cells (& CD4+ MO) as preferred host targets.
- Icosahedral (20-faced tr).
- Slow developing disease (up to 10 years before major symptoms seen).
- Genome is diploid, Plus (+) ssRNA genome.
- 9 genes (e.g. env, gag, pol) (tat, rev, nef) (vif, vpr, vpu) encoding: 15 Structural, Regulatory & Auxiliary Proteins.
- Proteins e.g. gp120 & gp41; p17,p24 – for the capsid,p9,p7; RT, IN, PR – viral enzymes which are important as most drugs target these enzymes.
Targets:
- •Infects cells of the immune system.
- •Uses the cells to replicate and move cell to cell.
- •In doing so changes the function of those cells.
- •Induces a selective loss of CD4+ T helper cells.
Protection
- •Effective immunity requires antibodies (B cells) to prevent infection and neutralize virus, and sufficient CD8+ T cells (CTL) to eliminate (kill) latently infected cells.
- CD4+ T helper cells & CD4+ MO/DC.
- HIV-1 can also be trapped by Follicular dendritic cells when enters the Lymph Node.
- One reason that the immune system fails to control HIV-1 infection is that the CD4+ T helper cells are the target of the virus. Progressive decline in CD4 T-cell function & numbers, decline in a specific order: HIV-specific, Recall (vaccinated Ab like typhoid etc), Allo, and Mitogen (and even IL-2).
What is the receptor for HIV-1?
CD4 molecule/Ag is the Receptor for HIV-1.
Most infecting strains of HIV-1 use co-receptor molecules (CCR5 and CXCR4) in addition to CD4 to enter target cells.
CCR5 mutation leads to protection and curing of HIV
More appears to be necessary for entry: A chemokine receptor on the surface of MO and activated T helper CD4+ cells was targeted by researchers as co-receptor for HIV because of its known binding to three chemokines that block infection.
How is HIV transmitted?
Sexually. The virus enters through mucosal surfaces. Increased by factors which damage such surfaces. Infects CD4+ cells, but also DC in the mucosa may bind to and carry the virus from the site of infection to the LNs where other immune cells become infected.
Infected blood - transfusion, sharing needles, blood products.
Mother to child before or during birth or via breast milk.
What is the immune response once infected?
Natural immunity:
- Mobilised within hours of infection and involves:
- Inflammation.
- Non-specific activation of macrophages.
- Non-specific activation of NK cells and complement.
- Release of cytokines and chemokines.
- Stimulation of pDCs via toll-like receptors.
Acquired immunity:
- Specific humoral responses where neutralising antibodies are produced.
- Anti-gp120 and anti-gp41 (Nt) antibodies are thought to be important in protective immunity.
- Non-neutralising anti-p24 gag IgG also produced. – not known the role or function of these antibodies;
- HIV remains infectious even when coated with antibodies. can get into immune cell through Fc receptor anyway
- CD4+ T cells
- White blood cells that orchestrate the immune response, signalling other cells in the immune system to perform their special functions.
- Recognise processed antigen - especially Gag p24 (peptides) - in the context of class II HLA molecules.
- Also known as T helper (Th) cells, these cells are infected, killed or disabled during HIV-1 infection.
- Selective loss of CD4+ T cells.
- CD8+ T cells
- White blood cells that kill cells infected with HIV or other viruses, or transformed by cancer (CTL). Also able to suppress viral replication.
- Secrete soluble molecules (cytokines and chemokines such as MIP-1a, MIP-1b, and RANTES) which are able to prevent infection by blocking entry of virus into CD4+ T cells.
- Recognise processed antigen - (peptides) - in the context of class I HLA molecules.
- Cd4 molecules binds to class ii and strengthens the interaction; cd4 t cell recognizes antigenic peptides in class 1 molecule, with antigenic peptides are very small; binds to class 1 molecules and strengthens the reaction; gag is affected and able to control the hidden virus in the host?

At which points of CD8+ activation does HIV-1 infection interfere?
Immune activation and disease progression
- Activated infected CD4+ helper T cells die and are lost
- Infected CD4+ T cells are also disabled (ANERGISED) by the virus
- MO/DC are not activated by the CD4+ T cells and can not prime naïve CD8+ CTL
- CD8+ T cell and B cell responses are diminished without help
- CD4+ T cell memory is lost
- Infected MO/DC are killed by virus or CTL
- Defect in antigen presentation
- Failure to activate memory CTL

How does HIV-1 acquire variation and mutations?
Replication of the retroviral genome depends on 2 steps - Reverse Transcriptase lacks the proof reading mechanisms associated with cellular DNA polymerases and therefore genomes of retroviruses are copied into DNA with low fidelity. Transcription of integrated viral DNA into RNA copies is also of low fidelity.
BOTH lack proof-reading steps which are needed for these, hence the mutations
Therefore HIV can accumulate many mutations and numerous variants or quasispecies.
- Escape from neutralising antibodies.
- Escape from HIV-1-specific T cells.
- Resistance and escape from antiretroviral drugs.
What is the life cycle of HIV?
Steps in Viral Replication
- Attachment/Entry
- Reverse Transcription & DNA Synthesis
- Integration
- Viral Transcription
- Viral Protein Synthesis
- Assembly of Virus & Release of Virus
- Maturation
What are the therapies for HIV-1 infections based on the life-cycle?
- Attachment getting into the cell
- Attachment inhibitors
- fusion inhibitors
- Reverse transcription for viral RNA to cDNA
- RT inhibitors
- Integration and transcription: viral DNA joins host DNA and makes mutliple viral RNAs
- Integrase inhibitors
- Translation producing viral proteins - none
- Viral protease cleaving viral proteins
- Protease Inhibitors
- Assembly and budding - getting out

What is the clinical course of HIV disease?
- Median time from infection with HIV to development of AIDS is 8 - 10 years.
- Viral burden (set point) predicts disease progression.
- Rapid progressors (10%) in 2 - 3 years.
- LTNP (<5%) stable CD4 counts and no symptoms after 10 years.
- ESN
- Effect of HAART.
- Elite controllers can suppress the progression and the disease below the currently detectable levels of HIV
- Long term non-progressors: can maintain a stable count with no symptoms for many years
- 3 different parameters used to monitor the disease progression:
Plasma viral load = causes a steep decline of CD4 lymphocytes – also seeing an increase in CD8 lymphocytes which appear to try and combat the virus, but the virus slowly progresses and the cd8 can’t continue protecting
Depletion of CD4+ helper/inducer subset of T-lymphocytes. Risk of opportunistic infections & neoplasms.
Patterns of progression:
Typical progressors- 85% -> 8-10yrs
Rapid progressors - 10% -> <3yrs
Long term non-progressors - >10-15yrs (normal, stable CD4; virgorous CD4 and CD8 anti-HIV responses

What are the possible mechanisms of long-term non-progression with HIV infection?
•Host genetic factors
- 1.Slow progressor HLA profile
- 2.Heterozygosity for 32-bp deletion in chemokine receptor CCR5
- 3.Mannose binding lectin alleles
- 4.Tumor necrosis factor c2 microsatellite alleles
- 5.Gc vitamin D-binding factor alleles
•Host immune response factors
- 1.Effective CTL & HTL responses
- 2.Secretion of CD8 antiviral factor
- 3.Secretion of chemokines that block HIV entry co-receptors CCR5 (e.g., MIP-1a, MIP-1b, and RANTES) and CXCR4 (e.g., SDF-1)
- 4.Secretion of IL-16
- 5.Effective humoral immune response
- 6.Maintenance of functional lymphoid tissue architecture
•Virologic factors
- 1.Infection with attenuated strains of HIV
How do we detect HIV-1?
- •HIV is found in all cases of AIDS.
- •In the infected patient, it can be detected by the presence of anti-HIV antibodies (ELISA) or by the presence of the virus itself (viral load) using polymerase chain reaction (PCR) which detects viral RNA. The latter is very sensitive and can show HIV in situations in which it is not detectable immunologically.
- •The HIV antibody ELISA is a screening test and the HIV antibody Western blot is a confirmatory test.
- •The initial baseline plasma viral load (that is when the patient is first monitored for virus number) is a good predictor of the time it will take for disease to appear.
Can use:
- Anti-HIV ELISA
- Anti-HIV Ab western blot
- VL PCR
•The course of HIV-1 disease in the patient is also followed by monitoring CD4+ T cell levels (Flow cytometry).
Cell surface markers: anti human: CD3,4,8,19,56 and CD57, 158b
•The onset of AIDS correlates with the diminution of the number of CD4+ T cells.
How do we do HIV-1 resistance testing?
Two established assays for measuring resistance to antiretroviral drugs
- •Phenotypic: Viral replication is measured in cell cultures under selective pressure of increasing concentrations of antiretroviral drugs – compared to wild-type
- •Genotypic: Mutations determined by direct sequencing of the amplified HIV genome (so far limited to sequencing of RT and P and/or In)
Both assays are available commercially (expensive)
What is HAART?
- Highly active antiretroviral therapy
- Substantial control of viral replication
- Increase in CD4 T cell counts
- Improvement in their host defences (dramatic decline in opportunistic infections (AIDS-related disease) & deaths (mortality))
- It was thought that a few years of treatment with potent drugs might eradicate HIV from a person’s body.
- If HAART stopped, then the viral load jumps back to baseline level
- HAART does not eliminate the virus from the patient (reservoir in resting CD4 T cells).
Effect on viral load and CD4 counts:
- Suppression of VL
- Initial CD4 rise – memory T-cells redistributed/increased
- Later CD4 rise is thymic naïve T-cells in younger patients, which means they can reconstitute the previous levels
- Need to be continued for life as no cure for HIV
Regimen:
- Combination of 3 or more drugs:
- two drug backbone + one or more binding agents
- Nuceloside reverse transcriptase inhibitors
- Non-NRTI
- Integrase inhibitors
- Attachement inhibitors
- Fusion inhibitors
- When to start:
- All symptomatic patients
- All CD4 <200 cells/ml
- START: CD4 200-350 cells/ml
- (All offered immediate treatment)
- Choices: 2NRTIs + NNRTI or boosted PI
Limitations:
- Effective HAART does not eradicate latent HIV-1 in the host
- Fails to restore HIV-specific T-cell responses
- Is dogged by the threat of drug resistance
- Significant Toxicities
- High pill burden
- Adherence problems
- Quality of life issues
- Cost (>40%)


