Histo: Respiratory Disease Flashcards
List some examples of airway diseases.
- Asthma
- COPD-chronic bronchitis
- Bronchiectasis
- Infections
List some examples of Parenchymal disease.
- Pulmonary oedema and diffuse alveolar damage (includes Acute respiratory distress syndrome and HMD)
- Infections
- COPD-Emphysema
- Granulomatous diseases
- Fibrosing interstitial lung disease and occupational lung disease
What is lung agenesis or hypoplasia?
- Low weight underdeveloped lungs
- Impaired fetal respiratory movements (movement is important in lung development)

List some examples of congenital lung disease.
- Lung agenesis or hypoplasia
- Tracheal & bronchial stenosis
- Congenital cysts
Define asthma.
A condition in which breathing is periodically rendered difficult by widespread narrowing of the airways that changes in severity over short periods of time.
NOTE: Prevalence increased in recent decades
What is the typical presentation of asthma?
- Presents with wheezing, acute SOB
- In a severe attack patients develop status asthmaticus
List some causes and associations of Asthma.
- Allergens and atopy (house dust mites)
- Pollution
- Drugs - NSAIDs
- Occupational - inhaled gases/fumes
- Diet
- Physical exertion - “cold”
- Intrinsic
- Underlying genetic factors
Describe the pathogenesis of asthma.
- Sensitisation to allergen
-
Immediate phase:
- Mast cells degranulate on contact with antigen
- Mediators released cause vascular permeability, eosinophil and mast cell recruitment and bronchospasm
-
Late phase:
- Tissue damage
- Increased mucus production
- Mucus hypertrophy

What are the macroscopic features of asthma?
- Mucus plug
- Overinflated lung

List the histological feeatures of asthma.
- Hyperaemia
- Eosinophilic inflammation and goblet cell hyperplasia - mucus
- Hypertrophic constricted muscle
- Mucus plugging and inflammation

Define COPD.
- Chronic cough productive of sputum
- Most days for at least 3 months over at least 2 consecutive years
Describe the pathophysiology of COPD.
Chronic injury to airways elicits local inflammation and reactive changes which predispose to further damage.
What are some common causes of COPD?
- Smoking
- Air pollution
- Occupational exposures
List some histological features of COPD.
- Dilatation of airways
- Hypertrophy mucous glands - Reid Index
- Goblet cell hyperplasia
What are some complications of chronic bronchitis?
- Repeated infections (most common cause of hospital admission and death)
- Chronic hypoxia and reduced exercise tolerance
- Chronic hypoxia results in pulmonary hypertension and right sided heart failure (cor pulmonale)
- Increased risk of lung cancer independent of smoking
Define Bronchiectasis.
Permanent abnormal dilatation of bronchi
What are common causes of bronchiectasis?
- Congenital
- Inflammatory
- Post-infectious (especially children or cystic fibrosis)
- Ciliary dyskinease 1° (Kartagener’s) and 2°
- Obstruction (extrinsic/intrinsic/middle lob syn.)
- Post-inflammatory (aspiration)
- Secondary to bronchiolar disease (OB) and interstitial fibrosis (CFA, sarcoidosis)
- Systemic disease (connective tissue disorders)
- Asthma
List some complications of bronchiectasis.
- Recurrent infections
- Haemoptysis
- Pulmonary hypertension and right sided HF
- Amyloidosis
Describe the inheritance pattern of Cystic Fibrosis.
- Autosomal recessive (approx 1/20 of population are heterozygous carriers)
- Affects 1 in 2,500 live births
Mutation in which gene causes Cystic Fibrosis?
- Chr 7q3 = CFTR gene (Cystic Fibrosis Transmembrane Conductance Regulator) = ion transporter protein
- Abnormality leads to defective ion transport and therefore excessive resorption of water from secretions of exocrine glands
- Results in abnormally thick mucus secretion - affects all organ systems
How does CF affect various organs?
- Lung: airway obstruction, respiratory failure, recurrent infection
- GI tract: meconium ileus, malabsorption
- Pancreas: pancreatitis, secondary malabsorption
- Liver: cirrhosis
- Male reproductive system: infertility
What is the management of cystic fibrosis?
- Improved treatment (physio, antibiotics, enzyme supplements, parenteral nutrition) has led to survival often into fourth decade
- Lung transplantation offers longer survival
What are the main consequences of CF?
- Over 90% of patients have lung involvement: patter of bronchiectasis
- Recurrent infections (S. aureus, H. influenzae, P. aeruginosa, B. cepacia)
- Other complications:
- Haemoptysis
- Pneumothorax
- Chronic respiratory failure and cor pulmonale
- Allergic bronchopulmonary aspergillosis (ABPA)
- Lung collapse
- Small airway disease
Define pulmonay oedema.
Accumulation of fluid in alveolar spaces as consequence of ‘leaky capillaries’ or ‘backpressure’ from failing left ventricle.
What are the main causes of pulmonary oedema?
- Left heart failure
- Alveolar injury
- Neurogenic
- High altitude
Describe the pathology of pulmonary oedema.
- Heavy watery lungs, intra-alveolar fluid on histology
- Poor gas exchange therefore hypoxia and respiratory failure

List some causes of acute respiratory distress syndrome in adults.
- Infection
- Aspiration
- Trauma
- Inhaled irritant gases
- Shock
- DIC
What causes hyaline membrane disease in newborns?
Lack of surfactant (mainly in premature babies)
On a cellular level, what insult results in ARDS?
- Acute damage to the endothelium and/or alveolar epithelium
- The basic pathology is the same regardless of cause: diffuse alveolar damage
Describe the appearance of the lungs on post-mortem examination in a patient who died from ARDS.
- Plum-coloured
- Heavy
- Airless

Outline the pathophysiology of ARDS.
- Exudative phase - the lungs become congested and leaky
- Hyaline membranes - form when serum protein that is leaked out of vessels end up lining the alveoli
- Organising phase - organisation of the exudates to form granulation tissue sitting within the alveolar spaces

What are the outcomes of ARDS?
- Death
- Superimposed infection
- Resolution (restoration of normal lung function)
- Residual fibrosis (leads to chronic respiratory impairment)
What are the various patterns of bacterial pneumonia?
- Bronchopneumonia
- Lobar pneumonia
- Abscess formation
- Granulomatous inflammation
List some causes of community-acquired bacterial pneumonia.
- Streptococcus pneumoniae
- Haemophilus influenzae
- Mycoplasma
List some causes of hospital-acquired bacterial pneumonia.
Gram-negatives (Klebsiella, Pseudomonas)
Which types of bacteria tend to eb implicated in aspiration pneumonia?
Mixture of aerobic and anaerobic
What is bronchopneumonia?
- Infection is centred around the airways
- Tends to be associated with compromised host defence (mainly the elderly) and is caused by low virulence organisms (e.g. Staphylococcus, Haemophilus, Pneumococcus)
- It will show patcy bronchial and peribronchial distribution often involving the lower lobes
What is lobar pneumonia?
- Infection is focused in a lobe of the lung
- 90-95% caused by S. pneumoniae
- Widespread fibrinosuppurative consolidation
What are the histopathological stages of lobar pneumonia?
- Stage 1: congestion (hyperaemia and intra-alveolar fluid)
- Stage 2: red hepatisation (hyperaemia, intra-alveolar neutrophils)
- Stage 3: grey hepatisation (intra-alveolar connective tissue)
- Stage 4: resolution (restoration of normal tissue architecture)

List some complications of pneumonia.
- Abscess formation
- Pleural effusion
- Empyema
- Fibrous scarring
- Septicaemia
What is a granuloma?
Collection of macrophages and multi-nucleate giant cells
Describe the histological appearance of atypical pneumonia.
- Interstitial inflammation (pneumonitis) without accumlation of intra-alveolar inflammatory cells
NOTE: causes include Mycoplasma, viruses, Coxiella and Chlamydia

What is a long term consequence of repeated small pulmonary emboli?
Pulmonary hypertension
List some types of non-thrombotic emboli.
- Bone marrow
- Amniotic fluid
- Trophoblast
- Tumour
- Foreign body
- Air
- Fat
Define COPD.
Emphysema is a permanent loss of alveolar parenchyma distal to the terminal bronchiole
What are the main causes of COPD?
Damage to alveolar epithelium
- Smoking
- Alpha-1 antitrypsin deficiency
- Rare - IVDU, connective tissue disease
Describe the pathogenesis of emphysema.
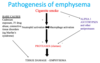
How does pathogenesis of COPD differ depending on cause?
- Smoking: Loss centred on bronchiole → CENTRILOBULAR
- Alpha 1 antitrypsin deficiency: Diffuse loss of alveolae → PANACINAR

What are the complications of COPD?
- Bullae - large air spaces
- Rupture → pneumothorax
- Respiratory failure
- Loss of area for gas exchange
- Compression of adjacent normal lung
- Pulmonary hypertension and cor pulmonale
What is a granuloma?
- Collection of histiocytes/macrophages +/- multinucleate giant cells
- Necrotising or non-necrotising

List some causes of Granulomatous disease.
- Infection
- Sarcoidosis
- Foregin body - aspiration or IVDU
- Drugs
- Occupational lung disease
What must be excluded when considering causes of granulomatous infection?
- TB must be excluded before considering other causes of granulomatous inflammation
- TB is fairly common in urban community and immunosuppressed

List some causes of granulomatous infections.
- Fungal (IS or foreign travel)
- Histoplasma
- Cryptococcus
- Coccidioides
- Aspergillus
- Mucor
- Other
- Pneumocystis
- Parasites
What is sarcoidosis?
Idiopathic granulomatous disease that most commonly affects lungs, skin, lympho nodes and eyes (may affect any organ)
What is the presumed pathogenesis of sarcoidosis?
An abnormal host immunological response to a variety of commonly encountered antigens, probably of environmental origin
Describe the lung involvement by sarcoid.
- Discrete epitheloid and giant cell granulomas, preferential distribution in upper zones with tendency to be perilymphatic, peribronchial
- Advanced disease may be fibrotic and peribronchial

How is diagnosis of sarcoidosis in the lung made?
- Biopsy (Bronchial/OLB) - Non-necrotising granulomas, either singly or coalescent. May undergo fibrosis.
- Elevated serum ACE
What are other causes of non-infectious granulomas?
- Intravascular talc granulomas in IV drug users
- Aspirated food

What are the different types of fibrosing lung disease?
- Idiopathic pulmonary fibrosis (Cryptogenic fibrosing alveolitis)
- Extrinsic allergic alveolitis - “farmers lung”
- Industrial lung disease - “pneumoconiosis”
What is idiopathic pulmonary fibrosis also known as?
Cryptogenic fibrosing alveolitis
What are the macro and microscopic features of idiopathic pulmonary fibrosis?
- Macro = basal and peripheral fibrosis and cyst formation
- Micro = interstitial fibrosis at varying stages
NOTE: It is a progressive disease with over 50% mortality in 2-3 years

What are the features of asbestosis?
- Fine subpleural basal fibrosis with asbestos bodies in tissue
- May also see pleural disease - fibrosis, pleural plaques
- Increased risk of lung cancer in the presence of asbestosis

What are some common pulmonary vascular diseases?
- Pulmonary hypertension
- Pulmonary thromboembolism
- Pulmonary vasculitis
What is the requirement for pulmonary hypertension diagnosis?
PHBP = mean pulmonary arterial pressure > 25 mmHg at rest
What are the main causes of pulmonary hypertension?
Precapillary:
- Vasoconstrictive
- Chronic hypoxia
- Hyperkinetic congenital heart disease
- Unknown (Primary pulmonary hypertension)
- Chronic liver disease, HIV infection, connective tissue disease
- Embolic
- Thromboembolic
- Parasitic (schistosomal)
- Tumour emboli
Capillary
- Widespread pulmonary fibrosis - mechanical distortion and chronic hypoxia
Postcapillary
- Veno-occlusive disease
- Lef-stided heart disease

What does chronic hypoxia result in?
- Normal response of lung is to reduce blood supply to hypoxic areas of lung and divert it to aerated zones
- Chronic hypoxia results in chronic vasoconstriction pulmonary arterioles
- COPD
- Fibrosing lung disease
What morphological changes in the lung does chronic hypoxia cause?
- Morphological changes in vessels
- Eccentric intimal fibrosis
- Thickening muscle wall

Where is the most common site of embolisism formation in pulmonary thromboembolism?
- Deep veins of leg (95%)
- Present with swelling leg (DVT)
- Present with symptoms of spread to lung (pulmonary embolism)
What determines risk of thrombus formation?
Virchow’s Triad:
- Factors promoting blood stasis
- Damage to endothelium
- Increased coagulation
List some risk factors of pulmonary thromboembolism.
- Advanced age
- Femal sex
- Obesity
- Immobility
- Cardiac failure
- Malignancy
- Trauma
- Surgery
- Childbirth
- Haemoconcentration
- Polycythaemia
- DIC
- Contraceptive pill
- Cannulation
- Anti-phospholipid syndrome
How might patients with small pulmonary emboli present?
- Patients present with pleuritic chest pain or chronic progressive shortness of breath
How does repeated emboli cause pulmonary hypertension?
- Small peripheral pulmonary arterial occlusion
- Haemorrhagic infarct
- Repeated emboli cause increasing occlusion of pulmonary vascular bed and pulmonary hypertension

What are the consequences of large pulmonary embolism?
- Large emboli can occlude the main pulmonary trunk (saddle embolus)
- Can cause:
- Sudden death
- Acute right heart failure
- Cardiovascular shock occurs in 5% of cases when >60% of pulmonary bed is occluded
- If patient survives, the embolus usually resolves
- 30% develop second or more emboli

List some causes of non-thrombotic emboli.
- Bone marrow
- Amniotic fluid
- Trophoblast
- Tumour
- Foreign body
- Air
What is pulmonary veno-occlusive disease? List some causes.
Fibrotic occlusion of pulmonary veins
Causes:
- IDIOPATHIC
- Some “herbal” teas and diet pills
- Chemotherapy
- Radiotherapy
- Bone marrow transplantation
- Renal transplantation
- HIV infection
- Systemic sclerosis

What are the complications of pulmonary hypertension?
Right sided heart failure
- Venous cngestion of visceral organs - “nutmeg liver”
- Peripheral oedema
- Pleural effusions and ascites
- Poorl lung perfusion and hypoxia

How may pulmonary vasculitis present?
Present as life threatening haemorrhage, chronic haemoptysis, mass lesion, interstitial lung disease
NOTE: it is uncommon
What are the different patterns of pulmonary vasculitis?
Variety of patterns from granulomatous vasculitis involving small-medium sized vessels (GPA) through to a leukocytoplastic vasculitis involving capillaries (e.g. with Rheumatoid arthritis)
What are the main types of lung cancer?
Non-small cell carcinoma
- Squamous cell carcinoma (30%)
- Adenocarcinoma (20%)
- Large cell carcinoma (20%)
Small cell carcinoma
What components of cigarette smoke are responsible for its carcinogenicity?
- Tumour initiators (polycyclic aromatic hydrocarbons)
- Tumour promoters (nicotine)
- Complete carcinogens (nickel, arsenic)
Which types of lung cancer are most strongly associated with smoking?
- Squamous cell carcinoma
- Small cell carcinoma
Which type of lung cancer tends to occur in non-smokers?
Adenocarcinoma
List some risk factors for lung cancer.
- Smoking
- Asbestos
- Radiation
- Air pollution
- Heavy metals
- Susceptibility genes (e.g. nicotine addiction)
Describe the sequence of histological changes that results in lung cancer.
Metaplasia → dysplasia → carcinoma in situ → invasive carcinoma

What feature of squamous epithelium makes it vulnerable to undergoing malignant changes?
It does not have cilia leading to a build-up of mucus
Within the mucus carcinogens accumulate
Where do squamous cell carcinomas tend to arise?
Centrally - arising from the bronchial epithelium
NOTE: there is an increasing incidence of peripheral squamous cell carcinomas (possibly due to deeper inhalation of modern cigarette smoke)
Where does adenocarcinoma of the lung tend to arise?
Peripherally - around the terminal airways
NOTE: it tends to be multi-centric and extra-thoracic metastases are common and occur early
What is the precursor lesion for adenocarcinoma of the lung?
Atypical adenomatous hyperplasia (proliferation of atypical cells lining the alveolar walls)
Which mutations are associated with adenocarcinoma in smokers?
Kras
Issues with DNA methylation
P53
Which mutation is associated with adenocarcinoma in non-smokers?
EGFR
What is large cell carcinoma of the lung?
- Poorly differentiated tumour composed of large cells
- There is no evidence of squamous or glandular differentiation
- It has a poor prognosis
Where does small cell lung cancer tend to arise?
Central - around the bronchi
NOTE: 80% present with advanced disease and it carries a poor prognosis
List some common mutations seen in small cell lung cancer.
P53
RB1
What is the difference in the chemosensitivity of small cell lung cancer and non-small cell lung cancer?
- Small cell - sensitive
- Non-small cell - not very chemosensitive
Which molecular changes are important to test for in adenocarcinoma?
- EGFR (responder or resistance)
- ALK translocation
- Ros1 translocation
Why is it important to know the tumour type precisely?
Some treatments can be fatal if the cancer is misdiagnosed
E.g. bevacizumab can cause fatal haemorrhage if used for squamous cell carcinoma
What is cancer of the pleura?
Mesothelioma


