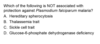
Hematology Path Flashcards
(220 cards)
Explain the process of maturation of T cells and NK cells.
What receptors are expressed by them?
Both have a common precursor.
Hint: All receptors expressed by T cells are below 10.

Explain where B cell mature and where naive B cells develop into plasma cells.

Where does the Ig rearrangement and Ig rearranged somatic mutation takes place?
Ig rearrangement takes place during B cell maturation which happens in the bone marrow whereas somatic mutation takes place in the presence of an antigen in the lymph nodes.

Explain the structure of a lymph node.
Paracortex consists of T cells, cortex contains B cells.

Enumerate common CD markers for different hematopoietic cell lines

Enumerate the function of the red pulp and white pulp of the spleen.
Spleen consists of white pulp and red pulp areas, white pulp has a function similar to lymph nodes as it contains B and T cells with germinal centers and mantle zone.
Red pulp has stromal cords and vascular sinuses so it allows the spleen to perform its blood filtering function by bringing the RBCs in close proximity with macrophages. Older erythrocytes are phagocytozed here.

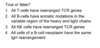
Explain the process of immunoglobulin gene rearrangement in B lymphocyte development.
How can we detect if a B cell has undergone Ig gene rearrangement? What is its significance?
- ‘Ig Somatic Mutation’ occurs in antigenically stimulated B-cells in both heavy and light chain hypervariable regions.
- Cells with increased affinity for antigen survive.
- Cells with decreased affinity for antigen removed through apoptosis
We can detect this by amplification and sequencing of V region which can then be compared with known germline V genes (which have not undergoine Ig somatic mutation).
This is important for treating some B cell neoplasms

Define hypersplenism and list causes of splenomegaly
Enlargement of spleen, could be due
- Infections and inflammatory conditions Infectious mononucleosis, malaria, typhoid fever, leishmaniasis, rheumatoid arthritis, SLE
- Congestive – expansion of red pulp
- Portal hypertension, splenic or portal vein thrombosis, cardiac failure
- Infiltrative Amyloidosis, hemolytic anemia, immune thrombocytopenia, storage diseases, neoplasms
List important causes of thymic hyperplasia
It is due to follicular hyperplasia. This can be for several reasons such as:
- Increased B-lymphocytes
- Myasthenia gravis
- SLE
- Graves disease and other autoimmune disorders
List important paraneoplastic syndromes observed with thymic neoplasms.
Myasthenia Gravis and Pure Red Cell Aplasia are 2 common paraneoplastic manifestations of thymic neoplasms.
What are some of the important things to remember from this hematologic lineage flow chart?

- All the recognizable precursors end with ‘blast’
- Cell division only occurs in multipotent stem cells, committed stem cells and recognizable precursors i.e ‘in the top half of the chart’
- These actively dividing cells are morphologically identical, only maturing and mature myeloid cells can be recognized based on their appearence.
- All the myeloid stem cells have limited life span, whereas the lymphoid cells can survive for many years and they can divide at any phase of cell cycle, even during the mature phase.
- All hematologic neoplasms originate from dividing cells, hence the cells in the top half of the chart.
What are the different growth factors involved in cell maturation and development?

What are the sites of hematopoiesis from prenatal life to adulthood?
Yolk sac: 3 weeks
Mesoderm of intraembryonic aorta, gonads, mesonephros region: 3 weeks to 3 months
Liver: 3 months to birth
Bone marrow: 4 month to death

How does hematopoiesis change with age?
Shifts to flat bones of axial skeleton, most common location to do a bone marrow biopsy is from the iliac crest of an adult or sometimes it can be done at the sternum
What is extramedullary hematopoiesis?
When the demand of hematopoiesis is high and the bone marrow can not keep up there is reactivation of hematopoiesis outside the bone marrow such as in liver, spleen, lymph nodes etc
The most common reason for this is hemolytic anemia or neoplasm
Explain the steps of Neutrophil development starting from Myeloblast.
Don’t need to know the names but it is important to know the morphological changes that occur during different stages of development

Explain the steps of erythroid maturation starting from Proerythroblast.
How does RBCs get rid of their nucleus?
Via pyknosis and ‘removal’ of the remaining nucleus

What are the different components of blood?

Explain the phenomena of left shift.
What is the significance of toxic granulation and Dohle bodies?
- Left shift refers to increased circulation of band neutrophils or even further stages of immature neutrophils that can be seen on a blood smear.
- Left shift is almost always induced by an inflammatory process
- Toxic granulations and Dohle bodies are morphological changes that are seen on neutrophils in left shift
- Presence of toxic granulations and Dohle bodies signifies the fact that the increase in neutrophils is due to an inflammatory etiology instead of a neoplastic etiology

What are the different components of bone marrow?
Sinusoids, hematopoietic cells and fat.
It is important to know that the blood is not continuous with the hematopoietic space.
What is the myeloid:erythrocyte normal ratio in the bone marrow?
3:1 in favor of Myeloid cells, which makes sense as myeloid cells like neutrophils have a life span max of 5 days, so there is a greater turnover
What cells are classified as granulocytes?
Neutrophils, basophils and eosinophils, primary function of these cells is phagocytosis
What is the function of basophils?
What does their granules contain?
IgE mediated allergic reactions.
Granule contain histamine, chondroitin sulfate and tryptase