Hard cards from BRS Flashcards
What occurs due to reduction in stretch detected by baroreceptors?
.This reduces the stretch on the baroceptors, reduced stimulation is immediately responded by the cardiac control centre- Sends signals to the sympathetic nerve, through the medulla oblongata to stimulate the heart rate and increase the blood pressure by vasoconstriction. Increased electrical stimulation results in release of noradrenaline onto the sino-atrial node, increases frequency of waves of excitation and thus contraction (systole).
Lung innervation
Doesn’t have a sympathetic nerve, but instead releases adrenaline to cause bronchodilation of the airways
Corticospinal tract

Which dorsal column travels ipsilaterally transmitting signals from the upper limb (T6 and above)?
Along the cuneate tract
Which dorsal column t transmits modalities of sensation from lower limbs (below T6)?
gracile tract
Where does the right adrenal vein drain into?
inferior vena cava
a phagocytic cell which forms the lining of the sinusoids of the liver and is involved in the breakdown of red blood cells.
kupffer cell
What effect does angiotensin II have on the zone glomerulosa?
Stimulates the production of aldosterone
How come patients with Addison disease have hyperpigmented skin?
Addison disease is an autoimmune disorder in which the body attacks the adrenal glands, effectively shutting them down. Patients end up with a whole host of problems, including hypotension (from the lack of mineralocorticoids) and hypoglycemia (from the lack of cortisol).
As the disease progresses, the adrenals put out less and less cortisol. The pituitary sees that drop in cortisol levels and responds by making more ACTH. ACTH is derived from a bigger precursor molecule called pro-opiomelanocortin (POMC). POMC is also a precursor for beta endorphin and melanocyte stimulating hormone (MSH)…so if you make more POMC (in order to make more ACTH), you’ll make more beta endorphin and MSH.
The beta endorphin doesn’t do much, as far as I know, but the MSH stimulates melanocytes, giving the skin a bronze color. Sometimes it’s an all-over bronze, like a tan (as in the photo above), and sometimes it’s more localized (in the gums, or in areas subjected to increased pressure, like over the knuckles or in skin folds).
However the bronze color manifests, it’s a telltale sign that the patient’s adrenal failure is primary (localized to the adrenal) and not secondary (due to hypopituitarism). In adrenal failure due to hypopituitarism, the whole problem is that the patient isn’t making ACTH (and thus the adrenals aren’t putting out their products) – so there’s no increase in MSH production and no hyperpigmentation.
hypoglycaemia

hyperglycaemia

hormone levels in menstrual cycle

what does each hormone do in the menstrual cycle?

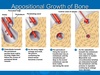
Picture of labelled cortical bone
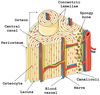
long bone showing enodsteum and periosteum