Hand and Wrist (Complete) Flashcards
What are the extensor compartments of the wrist and associated pathology?
- EPB + APL = De Quervain’s tenosynovitis
- ECRB + ECRL = intersection syndrome
- EPL = drummer’s wrist, traumatic rupture with DR #
- EDC + extensor indicis = extensor tenosynovitis
- EDM = Vaughn-Jackson syndrome
- ECU = snapping ECU

What are the extrinsic ligaments of the wrist?
[Rockwood and Green 8th ed. 2015]
- Volar ligaments (radial to ulnar)
- Radial collateral ligament
- Radioscaphocapitate
- Radioscapholunate
- AKA Ligament of Testut
- Actually a n.v. bundle
- No contribution to carpal stability
- Long radiolunate ligament
- Short radiolunate ligament
- Ulnolunate ligament
- Ulnotriquetral ligament
- Ulnocapitate ligament
2. Dorsal ligaments - Dorsal radiocarpal ligament (DRC)
- Dorsal intercarpal ligament (DIC)

What is normal wrist ROM?
[JBJS REVIEWS 2015;3(1):e1]
- Flexion = 80o
- Extension = 70o
- Pronation = 90o
- Supination = 90o
What is the differential diagnosis for radial sided wrist pain?
- Soft tissue
- De Quervains tenosynovitis
- FCR tendonitis/rupture
- Bone
- Radial styloid fracture
- Scaphoid fracture
- Joint
- CMC joint arthritis
- Radio-scaphoid arthritis
- Scapholunate instability

What is the differential diagnosis for ulnar sided wrist pain?
[JAAOS 2017;25:e150-e156]
- Soft tissue
- Snapping ECU/ECU tendonitis
- EDM tendinitis
- FCU tendinitis
- Bone
- Pisiform fracture
- Triquetral fracture
- Hamate fracture
- Ulnar styloid fracture
- Base of 5th metacarpal fracture
- Kienbock disease
3. Joint - Ulnar impaction syndrome
- Ulnar styloid triquetral impaction (USTI)
- TFCC tear
- Triquetrolunate instability
- Pisotriquetral arthritis
- DRUJ arthritis
- DRUJ instability
- LT ligament tear
- Ulnotriquetral ligament tear
4. Vascular - Ulnar artery thrombosis
5. Neurologic - Ulnar tunnel syndrome

Describe the SL ligament?
[JAAOS 2015;23:691-703]
Intra-articular C-shaped ligament with 3 components
- Dorsal – thickest, primary stabilizer
- Volar
- Proximal - thin, membranous

What is the motion of the scaphoid from ulnar to radial deviation ?
[JAAOS 2015;23:691-703]
Position of flexion and radial deviation to extension and ulnar deviation
What wrist motion minimizes motion between the scaphoid and lunate and minimizes tension on the SL ligament?
Dart throwers motion
- Radial-extension to ulnar-flexion
What percentage of patients with a DISI progress to SLAC wrist?
[JAAOS 2015;23:691-703]
<5-10%
Describe the Watson Scaphoid Shift test?
[JAAOS 2015;23:691-703]
Examiner provides dorsally directed pressure on the scaphoid tubercle while ranging the wrist from a position of ulnar deviation with slight extension to radial deviation with slight flexion
- If SLIL is injured:
- Dorsal pressure subluxates the scaphoid onto the dorsal rim of the radius
- When pressure is released, a palpable clunk and reproduction of dorsal wrist pain occur as the scaphoid relocates into the radioscaphoid fossa.

What are the radiographic classifications of SL ligament injury?
[JAAOS 2015;23:691-703]
- Static instability
* SL instability evident on plain film - Dynamic instability
- SL instability evident on stress views
- Stress view = AP clenched fist with 30° ulnar deviation
- Predynamic instability
* SL injury evident on advanced imaging or arthroscopy
What are the radiographic features of a SL ligament injury?
[JAAOS 2015;23:691-703]
- Widened SL distance
- Cortical ring sign
- Shortening of the scaphoid
- Scapholunate angle >70° (normal = 30-60)
- Lunate extension
- DISI defined by radiolunate angle >15°

What arthroscopic portal is the SL ligament best visualized from?
[JAAOS 2015;23:691-703]
Visualized from the radiocarpal space through the 3-4 portal
- Probe in the 4-5 or 6R portal

What is the arthroscopic classification of SL ligament injury?
[JAAOS 2015;23:691-703]
Geissler Classification
- Stage I
- 1mm probe cannot enter SL space from midcarpal joint
- Stage II
- 1mm probe can enter SL space from midcarpal joint but not rotate 90°
- Stage III
- 1mm probe can enter SL space from midcarpal joint and rotate 90°
- Stage IV
- 2.7mm scope can drive through the SL space from the midcarpal and radiocarpal joint
What are the surgical options for managing SL ligament injury?
[JAAOS 2015;23:691-703]
- Primary repair
- Repaired with two horizontal mattress sutures through bone tunnel or suture anchor
- Protected with K-wire or screw augmentation
- +/- capsulodesis augmentation
- Indicated for acute tears
2. Arthroscopic debridement - Indicated for symptomatic partial tears
3. Reconstructive procedures - Indicated for high grade tears with no arthritis
- Blatt capsulodesis
- Capsular flap is attached to the distal scaphoid to prevent flexion
- Recommend using the DIC ligament
- ***Note – does not address the SL gap or lunate extension
- Capsular flap is attached to the distal scaphoid to prevent flexion
- Modified Brunelli procedure
- Portion of the FCR from the base of the 2nd metacarpal is passed through the distal scaphoid and attached to the dorsal lunate
- Ligament reconstruction
- Most common donor site is retinaculum of the third dorsal compartment of the wrist with bone blocks from the distal radius
- RASL
- ‘Reduction and association of the scaphoid and lunate’
- Herbert screw fixes the scaphoid and lunate to create a fibrous union (‘neoligament’)
- Salvage Procedures
- Indicated for high grade tears with arthritis
- Arthroscopic debridement
- Radial styloidectomy
- Wrist denervation
- PRC
- 4-corner fusion
- Limited carpal fusion
- Arthroplasty
- Total wrist fusion

What is the technique for a Blatt capsulodesis?
- Original technique
- Utilized a strip of dorsal wrist capsule attached to the distal radius and inserted onto the distal pole of the scaphoid preventing scaphoid flexion
- Disadvantage
- Wrist flexion limited by ~20° due to crossing of the radiocarpal joint
- Modified DIC capsulodesis
* Detaches the proximal portion of the DIC from the triquetrum and after reduction of the scaphoid flexion it is attached to the lunate

What is the technique for the Brunelli procedure?
- Dual volar and dorsal incisions
- A portion of the FCR is passed through the scaphoid tuberosity and sutured to the remnants of the SLIL on the dorsal aspect of the scaphoid.
* The remaining portion of the FCR slip is anchored to the dorsal ulnar corner of the distal radius

What is the technique for the modified Brunelli procedure?
Triligament tenodesis described by Garcia-Elias
- A strip of FCR tendon is passed from the volar scaphoid tuberosity to the dorsal ridge to reconstruct the scaphotrapezial ligament
- The tendon is fixed dorsally to the lunate, passed through a slit in the dorsal radiotriquetral ligament, and sutured back on itself to recreate the SL ligament.

What is the most common pattern of wrist arthritis?
SLAC (55%)
What is the pathomechanics of SLAC and SNAC wrist development?
- In the normal wrist:
- Scaphoid links the proximal and distal carpal rows
- Proximal row moves with the scaphoid
- Scaphoid has a tendency to assume a flexed posture
- Capitate longitudinal load on the lunate is eccentric causing the lunate and triquetrum to extend
- These forces are balanced as long as the link between the scaphoid and lunate are intact
2. With SL ligament disruption: - The scaphoid flexes and lunate/triquetrum extend independently
- Radiolunate joint remains congruent with lunate extension
- Radiolunate joint preserved
- Radioscaphoid joint becomes incongruent with scaphoid flexion
- Radioscaphoid degeneration progresses
- With scaphoid nonunion
- The distal scaphoid flexes
- The proximal scaphoid extends with the lunate and triquetrum
What are the radiographic stages of SLAC wrist?
Stage I - radial styloid
Stage II - radioscaphoid joint
Stage III - capitolunate joint
[Stage IV - pancarpal involvment (controversial)]
***Radiolunate typically spared
Initially, degeneration occurs between the radial styloid and radial side of scaphoid near the waist
- Degeneration progresses to the proximal pole involving the entire radioscaphoid joint
- With scaphoid flexion and loss of the link between the distal and proximal rows increase load occurs in the midcarpal joints (loss of buttress)
- Capitolunate degeneration develops with eventual migration of the capitate proximally between the scaphoid and lunate

What are the radiographic stages of SNAC wrist?
Stage I - radial styloid
Stage II - proximal scaphocapitate joint
Stage III - capitolunate joint
Initially, degeneration occurs between the radial styloid and radial side of the distal scaphoid fragment
- Degeneration does not progress proximally in the radioscaphoid joint because the proximal scaphoid relationship with the lunate is maintained
- Degeneration progresses to the midcarpal joint starting with the proximal scaphocapitate joint then the capitolunate joint

What are the treatment options for SLAC and SNAC wrist?
Stage I
- Radial styloidectomy
- Distal pole excision (SNAC)
- Wrist denervation (AIN and PIN)
Stage II
- Proximal row carpectomy (PRC)
- Four corner fusion
Stage III
- Four corner fusion
- [PRC with capsular flap interposition]
(Stage IV – pancarpal)
- Total wrist fusion
- Total wrist arthroplasty
What is the most common complication following PRC?
[JHS (Eur Vol) 2015,40E(5) 450–457]
Synovitis and significant edema
What is the most common complication following 4-corner fusion?
[JHS (Eur Vol) 2015,40E(5) 450–457]
Nonunion
What are the advantages and disadvantages of a PRC and Four corner fusion?
[JHS (Eur Vol) 2015,40E(5) 450–457]
- PRC
- Advantages
- Greater postoperative ROM
- Flexion, extension, total flexion/extension arc
- Lower complication rate
- Others
- Earlier ROM
- No hardware
- Greater postoperative ROM
- 4-corner fusion
- Advantages
- Greater radial deviation ROM
- Greater grip strength
What are the technical steps in performing a PRC?
- Longitudinal incision centred over Lister’s tubercle
- Flaps are elevated off the extensor retinaculum
- Extensor retinaculum is opened over the 3rd compartment and EPL is retracted radial
- 2nd and 4th compartments are elevated off the dorsal capsule
- PIN is identified and transected
- Ligament-sparing capsulotomy is performed
- Longitudinal split of the DRC and DIC
- Described by Berger, Bishop and Bettinger 1995
- Scaphoid, lunate and triquetrum are excised
- Preserve the volar radioscaphocapitate
- Capitate is seated in the lunate fossa
- Radial styloidectomy is performed if there is impingement noted with radial deviation
- Capsule is closed
- Extensor retinaculum is closed leaving the EPL subcutaneous
What are the technical steps in performing a 4-corner fusion?
- Longitudinal incision centred over Lister’s tubercle
- Flaps are elevated off the extensor retinaculum
- Extensor retinaculum is opened over the 3rd compartment and EPL is retracted radial
- 2nd and 4th compartments are elevated off the dorsal capsule
- PIN is identified and transected
- Ligament-sparing capsulotomy is performed
- Scaphoid is excised
- Lunate, capitate, hamate, triquetrum are prepared for fusion
* Articular cartilage and subchondral bone are removed along the dorsal 75% - Lunate extension is corrected and provisional fixation with K-wires between the carpal bones
- Bone graft options include excised scaphoid, local distal radius and ICBG
- Definitive fixation options include K-wire, staples, headless compression screws, circular plates

What is the DRUJ articulation?
[JAAOS 2012;20:623-632] [The Journal of Hand Surgery (European) 2014, 39E(7) 727–738]
- Ulnar head and sigmoid notch of distal radius
- Asymmetric
- Sigmoid notch has a 4- to 7-mm greater radius of curvature than the ulnar head
- Bony contribution to DRUJ stability is 20%
- TFCC primary soft tissue stabilizer

What motions does the DRUJ allow?
[JAAOS 2012;20:623-632]
- Rotation
- Translation (dorsal and volar)
- Dynamic translation
- Pronation = 2.8mm of dorsal translation
- Supination = 5.4mm of volar translation
- Longitudinal
- Dynamic ulnar variance
- Pronation = relative positive
- Supination = relative negative

What are the stabilizing structures of the DRUJ?
[JAAOS 2012;20:623-632]
- TFCC
- Pronator quadratus
- Interosseous membrane
- Joint capsule
From anatomy notes:
1) Triangular fibrocartilage complex (TFCC)
2) Joint capsule
3) IO membrane
4) Pronator quadratus
5) ECU tendon & sheath

What is the effect of forearm rotation on the volar and dorsal radioulnar ligaments?
- Pronation = dorsal superficial and volar deep ligaments tighten
- Supination = volar superficial and dorsal deep ligaments tighten

What is the effect of neutral, positive and negative ulnar variance on load transmission?
[JAAOS 2012;20:623-632]
- Neutral – 20% load through the distal ulna
- Positive – lengthening 1mm increases ulnocarpal loading by 50%
* 2.5mm lengthening increases load to 42% - Negative – decrease ulnocarpal load transmission
- 2.5mm shortening decreases load to 4%
- Also increases pressure in DRUJ and stabilizes DRUJ by increasing tension on TFCC
What is radioulnar convergence?
[JAAOS 2012;20:623-632]
- Ulnar head functions to maintain radioulnar distance during forearm rotation
- Loss of ulnar head leads to convergence of the radius and ulna

What are the causes of DRUJ arthritis?
[JAAOS 2012;20:623-632]
- Post-traumatic
- Distal radius malunion
- Distal radius fracture with extension into sigmoid notch
- Inflammatory arthritis (RA)
- Madelung deformity
- Tumor
* Osteochondroma
What are the surgical management options for DRUJ arthritis?
[JAAOS 2012;20:623-632]
- Darrach procedure
- Indications
- Low demand and non-reconstructable joint
- Technique
- Subperiosteal distal ulna exposure
- Distal ulna resection just proximal to sigmoid notch
- Preserve soft tissue
- TFCC
- ECU sheath
- Periosteum
- Hemiresection
- Indications
- Requires intact TFCC
- Technique
- Classic
- Resection of articular distal ulna with remainder left insitu including TFCC attachment
- Hemiresection interposition technique (HIT)
- Resection as classic
- Soft tissue interposition into void to prevent radioulnar convergence
- Capsular flap or free tendon
- Classic
- Sauve-Kapandji procedure
- Indications
- Young, active patient with nonreconstructable joint
- Technique
- Dorsal or ulnar approach preserving soft tissue
- Identify and protect the dorsal cutaneous branch of the ulnar nerve
- Ulnar neck resection just proximal to sigmoid (~10-15mm)
- Sigmoid notch and ulnar head prepared for fusion (cancellous bone)
- DRUJ fusion with 2 k-wires or 3.5mm screw
- Neutral ulnar variance
- Pronator quadratus interposed in osteotomy site (prevents re-ossification)
- FCU slip can be tenodesed through drill hole in ulnar stump to prevent instability
- Partial ulnar head arthroplasty
- Indications
- Isolated DRUJ arthritis without instability
- Failed HIT
- Total ulnar head arthroplasty
- Indications
- Painful instability after failed resection
- Isolated instability
- Requires stability from native soft tissues
- Total DRUJ arthroplasty
- Indications
- Incompetent native soft tissues
- Salvage option after failed distal ulnar resection

What are complications of resection arthroplasty (Darrach, HIT, S-K procedure)?
[JAAOS 2012;20:623-632]
- Pain
- Ulnar stump instability
- Ulnar translation of carpus
- Radioulnar convergence
- Re-ossification of resection (S-K procedure)
What are surgical options to manage a residual ulnar stump instability?
[JAAOS 2012;20:623-632]
- ECU and FCU tenodesis
- Tendon allografts
- Achilles allograft in interosseous space between radius and ulna
- 2 slips of BR through distal radius and then around ulna stump

What are the types of DRUJ instability?
[The Journal of Hand Surgery (European) 2014, 39E(7) 727–738]
- Pathology
- Primary
- Relatively rare
- Usually due to inflammatory/connective tissue disease (eg. RA, Ehlers-Danlos)
- Posttraumatic
- Most common (11% of distal radius fractures)
- Worse DRUJ instability with increasing dorsal angulation of distal radius (signif beyond 20o)
- Post-surgical
- I.E. Darrach, Sauve-Kapandji
- Presents with pain/clicking with rotation
- Direction
- Dorsal
- Volar
- Bidirectional
- Severity
* Asymptomatic
* Symptomatic - Static vs dynamic
- Acute vs. chronic
What are the associated injuries with DRUJ instability?
- Distal radius fracture
- Ulnar styloid fracture
- Galeazzi fracture
- Essex-Lopresti lesion
- Both bone forearm fracture
- TFFC tear
- Capsule/ligament tear
What is included in the physical exam when assessing DRUJ instability?
- Inspection
* Prominent distal ulna - Palpation
* Ulnar styloid tenderness - ROM
- Observe for loss of supination/pronation compared to contralateral side
- Dorsal ulnar dislocation = preferential loss of supination (locked pronation)
- Volar ulnar dislocation = preferential loss of pronation (locked supination)
- Pain or subluxation
4. ‘Shuck test’ (Ulnar Ballotment) - Attempt volar and dorsal subluxation of distal ulna with forearm in pronation, neutral and supination
- Compare to contralateral side
- ‘Press test’
- Ask patient to arise from a chair using the wrists
- Focal pain at the distal ulna can indicate a TFCC injury
What imaging is indicated when evaluating DRUJ instability?
- Radiographs with forearm in neutral rotation
- CT
***Consider MRI if instability associated with intermittent ulnar neuropathy
- DRUJ subluxation can mechanically irritate the ulnar nerve at the wrist
- “Subluxation-related ulnar neuropathy”
What are 3 imaging findings with radioulnar impingement syndrome following distal ulnar resection?
- Shortened distal ulna ending proximal to the sigmoid notch
- Scalloping of the distal radius along its ulnar border
- Radioulnar convergence
* Narrowing between radius and ulna

What is the management of DRUJ instability?
[The Journal of Hand Surgery (European) 2014, 39E(7) 727–738][ASSH Manual of Hand Surgery]
- Nonoperative
- Acute dislocation
- Closed reduction and splinting in stable position for 6 weeks
- Dorsal radioulnar ligament injury
- Splint midsupination
- Volar radioulnar ligament injury
- Splint midpronation
2. Operative
- Splint midpronation
- Dorsal radioulnar ligament injury
- Closed reduction and splinting in stable position for 6 weeks
- Acute DRUJ instability indications
- Irreducible
- Open reduction
- +/- DRUJ pinning
- +/- TFCC repair
- +/- ulnar styloid fracture fixation
- Associated fractures
- ORIF of associated fractures often resolves the instability
- If remains unstable pin in reduced position
- TFCC tear
- Open or arthroscopic repair
- Open
- Dorsal interval between 5+6 compartment
- TFCC repaired to distal ulna with anchor or suture tunnels
- Open
- Reconstruction if repair fails
- Open or arthroscopic repair
- Irreducible
- Chronic DRUJ instability
- In Absence of arthritis
- Distal radius malunion
- Correction indicated if >20° of dorsal angulation (controversial)
- Correct distal radius malunion then assess DRUJ stability
- If still unstable reconstruct the DRUJ
- Reconstruction
- Indications
- TFCC or radioulnar ligament repair failure
- Unrepairable
- Adams procedure +/- notchplasty (if flat lesser sigmoid) [HAND (2007) 2:123–126]
- Dorsal approach between 5-6 compartments
- L-shaped capsulotomy
- Elevate 4th compartment off distal radius
- Drill 3.5mm from dorsal to volar just radial to lesser sigmoid notch (distal radius)
- 3.5mm drill hole from ulnar neck to fovea
- Harvest palmaris longus (alternative plantaris or slip of FCU)
- Small volar approach between ulnar nerve and flexor tendons
- Suture passer from dorsal to volar retrieves graft from volar side
- Limbs are then passed through ulnar tunnel, wrapped around ulnar neck then sutured to each other
- Indications
- Distal radius malunion
- In Presence of arthritis
- Darrach with ulnar stump stabilization
- Sauve-Kapandji
- In Absence of arthritis

What is the management of radioulnar impingement syndrome (failed Darrach or Sauve-Kapandji)?
- ECU and FCU tenodesis
- Tendon allografts
- Achilles allograft in interosseous space between radius and ulna
- 2 slips of BR through distal radius and then around ulna stump
- Ulnar head replacement
* Require some degree of native soft tissue - Total DRUJ replacement
* Does not require native soft tissue - Salvage
- One-bone forearm (radioulnar synostosis)
- Wide excision (25-50% of distal ulna)

What are the patterns of wrist arthritis and causes of each?
[Bone Joint 2015;97-B:1303–8]
- Pancarpal arthritis
* Advanced inflammatory or post-traumatic arthritis - Radioscapholunate arthritis
- Intra-articular distal radius fractures
- Kienbock’s
- Inflammatory arthritis
- Radioscaphoid arthritis
* SLAC, SNAC - Radiolunate arthritis
* Intra-articular lunate facet fracture

What are the treatment options for each pattern of wrist arthritis?
[Bone Joint 2015;97-B:1303–8]
- Pancarpal arthritis
- Low demand = wrist arthroplasty
- High demand = total wrist fusion
- Radiolunate arthritis
* Midcarpal joint preserved = radiolunate fusion - Radioscaphoid arthritis
- Capitate-lunate preserved = PRC or 4-corner fusion
- Capitate-lunate involved = 4-corner fusion
- Radioscapholunate arthritis
* Midcarpal joint preserved = radioscapholunate fusion

What are the important considerations when performing a radioscapholunate fusion?
[Bone Joint 2015;97-B:1303–8]
- Midcarpal is free of arthritis
- Distal scaphoid pole excision
* Increases ROM
* Decreases pain
* Rncreases rate of union due to unlocking the midcarpal joint

What is the resulting wrist function following total wrist arthrodesis?
[JAAOS 2017;25:3-11]
- Loss of flexion, extension, ulnar and radial deviation
- Supination and pronation are retained
What are the indications for total wrist fusion?
[JAAOS 2017;25:3-11]
- Rheumatoid arthritis
- Post-traumatic arthritis
- Spastic wrist contracture
- End stage osteonecrosis
- Kienbock disease
- Preiser disease
- Complete brachial plexus paralysis
- Failed wrist arthroplasty
- Postinfection degeneration
- Failed wrist surgery
- PRC
- SL reconstruction
- Arthrodesis
- Silicone synovitis
What are the contraindications for total wrist fusion?
[JAAOS 2017;25:3-11]
- Active infection
- Lack of an adequate soft tissue coverage
What are the complications associated with total wrist arthrodesis?
[JAAOS 2017;25:3-11]
- Major
- Nonunion
- Ulnocarpal impaction
- Carpal tunnel syndrome
- Extensor tenosynovitis
- Deep infection
- Implant-related problems
- Minor
- Superficial infection
- Carpal tunnel symptoms
- Intraoperative fractures
- Postoperative fractures
- Asymptomatic radiographic loosening
What are advantages of wrist arthrodesis vs. wrist arthroplasty?
[JAAOS 2017;25:3-11]
- Reliable pain relief
- Lower complication rate
- Less revision
What is the recommended position of wrist fusion?
[JAAOS 2017;25:3-11]
- Unilateral wrist arthrodesis
- 10-15° extension
- Slight ulnar deviation
- Bilateral wrist arthrodesis
- Dominant wrist = slight extension
- Nondominant wrist = neutral to slight flexion
What are the general principles of total wrist arthrodesis?
[JAAOS 2017;25:3-11]
- Adequately prepare the joints
- Remove cartilage and expose subchondral bone
- Without PRC:
- Radiolunate
- Radioscaphoid
- Scapholunate
- Scaphocapitate
- Lunocapitate
- Triquetrohamate
- 3rd CMC joint
- With PRC
- Radiocapitate
- Radiohamate
- 3rd CMC joint
- Prepare the distal radius to accept plate
* Remove dorsal cortical rim - +/- triquetrum excision
* Prevents ulnocarpal abutment and provides bone graft - Bone graft
- Triquetrum
- PRC
- Olecranon
- Precontoured stainless steel locking wrist fusion plate
- Fix to 3rd metacarpal shaft
- Compression across arthrodesis sites
- Manual compression and compression by design through plate
- +/- ECRL and ECRB tendon transfer over plate if finger extensor directly overlying plate
- +/- distal ulna resection if DRUJ arthritis present
- Manual compression and compression by design through plate

What are the radiographic parameters to assess for distal radius malunion and how do they affect the biomechanics of the wrist?
[JAAOS 2007;15:27-40]
- Radial tilt
* Dorsal angulation leads to:- Loads being shifted dorsal
- DRUJ incongruency
- Tightening of the interosseous membrane
- Resulting loss in supination-pronation
- Preferential loss of wrist flexion and forearm supination
* Dorsal angulation causes two forms of wrist instability: - Dorsal radiocarpal subluxation with maintenance of midcarpal alignment
- Adaptive DISI
* Volar angulation preferentially decreases extension and pronation
- Radial length
- Ulnar variance
* Ulnar positive variance leads to ulnocarpal impaction - Radial inclination
* Decrease in inclination shifts loads from the scaphoid fossa to the lunate fossa - Joint congruity

What are contraindications to distal radius osteotomy for malunion?
[JAAOS 2007;15:27-40]
- Advanced degeneration
- Fixed intercarpal malalignment
- Severe osteoporosis
- CRPS
- Inability to comply with postoperative therapy
- Serious medical comorbidiities
- Very low demand
What are the 4 components of surgical management for distal radius malunion?
[JAAOS 2007;15:27-40]
In order:
- Osteotomy
- Bone grafting
- Fixation
- Ulnar-side procedure
What are the advantages and disadvantages of closing vs. opening wedge osteotomy for correction of distal radius malunion?
[JAAOS 2007;15:27-40]
- Closing wedge osteotomy
- Advantage
- More stable construct (bone-to-bone contact)
- Disadvantage
- Shortening of radius relative to ulna
- Requires ulnar sided procedure
- Shortening of radius relative to ulna
- Opening wedge osteotomy
- Advantage
- Restores radial length
- Corrects ulnar variance
- Corrects inclination and tilt
- Disadvantage
- Less stable construct
- Increased risk for nonunion or hardware failure

What are the bone graft options typically used in osteotomies correcting distal radius malunion?
[JAAOS 2007;15:27-40]
- ICBG – corticocancellous
- Local distal radius graft
- Cancellous autograft or allograft
- Bone graft substitute
What are the advantages and disadvantages of volar vs. dorsal plating in osteotomy correction of distal radius malunion?
[JAAOS 2007;15:27-40]
- Dorsal plating
- Advantage
- Easy access for bone graft in dorsal opening wedge osteotomy
- Disadvantage
- Hardware irritation and tendon rupture
- Volar plating
- Advantage
- Less hardware irritation and tendon rupture
- Disadvantage
- Difficult access for bone graft
- May require additional releases
- Difficult access for bone graft
What are the ulnar-sided procedures that can be considered in context of distal radius malunion?
[JAAOS 2007;15:27-40]
- Hemiresection-interposition
- Ulnar shortening osteotomy
- ‘Wafer’ resection
- Sauve-Kapandji
* DRUJ fusion with proximal pseudoarthrosis) - Darrach
* Complete distal ulna resection - Arthroplasty

What is the best timing for distal radius corrective osteotomy for malunion?
As soon as possible
- Avoids soft tissue contracture
What are the general types of distal radius malunions and what are the surgical considerations for each?
[Operative Techniques in Hand, Wrist, and Elbow Surgery]
- Dorsally angulated, extra-articular
- Approach – volar or dorsal
- Volar approach requires:
- Volar locking plate fixation
- BR Z-lengthening or release
- Dorsal and radial soft tissue and periosteal release
- Use of the locking plate as a reduction/correction tool
- First fix to distal fragment anatomically
- Can often be done prior to osteotomy
- Then bring the plate to the shaft correcting inclination, tilt and length
2. Volarly angulated, extra-articular
- First fix to distal fragment anatomically
- Volar approach requires:
- Approach – volar
- Less radial and dorsal release required
- Intra-articular
- Approach – volar or dorsal depending on location of fragment
- Dorsal approach
- Transverse capsulotomy for direct visualization
- Volar approach
- Do not perform capsulotomy
- Reduction may be visualized through osteotomy
- Dorsal approach
- Intra-articular and extra-articular deformity
- Approach – volar, dorsal or combined
- Typically, the intra-articular malunion is corrected first followed by the extra-articular malunion
- Often a dorsal approach is needed for dorsal capsulotomy and visualization of articular reduction
- Fixation can be volar, dorsal or fragment specific
What are the risk factors for scaphoid nonunion?
[JAAOS 2009;17:744-755]
- Displacement >1mm
- Proximal fracture
- Delayed treatment
- Inadequate immobilization
- Associated carpal instability
- Osteonecrosis
What are signs of scaphoid proximal pole osteonecrosis?
[JAAOS 2009;17:744-755]
- Radiographic sclerosis
- MRI changes
- Absence of punctate bleeding intraoperative

What are the indications for vascularized bone grafting in scaphoid non-union?
[JAAOS 2009;17:744-755]
Scaphoid nonunion with proximal pole osteonecrosis and/or failure of previous grafting
What are the graft options for scaphoid nonunion based on location of fracture and presence of deformity?
[JAAOS 2009;17:744-755]
- Proximal 1/3 nonunion without significant humpback deformity
- Recommended
- 1,2 ICSRA (intercompartmental supraretinacular artery) - AKA Zaidenberg
- Origin
- Radial artery 5cm proximal to radiocarpal joint
- Advantages – single approach
- Disadvantages
- Unable to correct humpback deformity
- Vulnerable to kinking and impingement
- Origin
- Capsule-based (4th extensor compartmental artery)
- Advantages
- Simple harvesting technique
- Short arc of rotation and low risk of kinking
- Disadvantage
- Cannot correct humpback deformity
- Violates dorsal radiocarpal and intercarpal ligaments
- Advantages
- 1,2 ICSRA (intercompartmental supraretinacular artery) - AKA Zaidenberg
- Alternatives
- 2,3 ICSRA
- Free vascularized bone graft
- Medial femoral condyle or iliac crest
2. Waist nonunion and humpback deformity
- Medial femoral condyle or iliac crest
- Recommended
- Volar radius VBG (AKA Mathoulin)
- Origin
- Radial carpal artery
- Advantages
- Single incision
- Preserves dorsal blood supply
- Simultaneous correction of humpback deformity
- May preserve wrist flexion (compared to dorsal grafting)
- Single incision
- Origin
- Volar radius VBG (AKA Mathoulin)
- Alternatives
- Free VBG
- Medial femoral condyle or iliac crest
- Free VBG

What imaging should be obtained to assess for nonunion following prior surgical management of scaphoid fracture?
[JAAOS 2013;21:548-557]
- Radiographs
- Wrist PA, lateral, scaphoid, 45° pronated and supinated oblique view
- Assess for:
- Sclerosis
- Cysts
- Bone resorption at fracture site
- Hardware loosening
- CT scan
- Assess for:
- Bony union
- Arthritis
- Screw placement
- Fracture reduction
- Proximal pole sclerosis
What are the indications for reoperation following prior surgical fixation of scaphoid fracture?
[JAAOS 2013;21:548-557]
At 3 months if there is inadequate union and evidence of one of the following:
- Improper screw placement (at least 3-4 screw threads in each fragment)
- Insufficient compression across fracture site (presence of gapping)
- Inadequate fixation
- Lack of appropriate bone grafting
- Based on OR report or report from surgeon
What are the graft options for reoperation for scaphoid nonunion following prior surgical fixation?
[JAAOS 2013;21:548-557]
- Nonvascularized Bone Graft
- Useful when technical error is the primary cause
- IE. Screw malposition, fracture malreduction
- Options:
- Distal radius
- Tricortical iliac crest (deformity correction)
- Advantages – less technically challenging
- Disadvantages
- Heals by creeping substitution and resorption
- Prolongs time to union and reduces mechanical stability during healing
- Heals by creeping substitution and resorption
- Union rate = 70%
2. Vascularized bone graft - Union rate = 86%
- Options
- Zaidenberg (1,2 ICSRA)
- Mathoulin (Volar branch radial carpal artery)
- Free VBG (Femoral condyle of Iliac crest)
- Arterialization
* Direct implantation of the second dorsal intermetacarpal artery into the scaphoid
What is the approach to surgical management of scaphoid nonunion following prior surgical fixation?
[JAAOS 2013;21:548-557]
- If scaphoid alignment and initial screw position is acceptable and scaphoid is viable:
* Revise with a larger diameter variable pitch screw following the same tract with distal radius bone graft - If screw placement not acceptable:
* Redirect the screw
What is the treatment algorithm for scaphoid nonunion based on specific fracture characteristics?
[Operative Techniques: Hand and Wrist Surgery, 3rd Ed. Chung]
- Delayed union (<6 months)
* ORIF with headless compression screw - Established nonunion without humpback
* ORIF with headless compression screw + bone graft (cancellous ICBG or distal radius) - Nonunion with humpback deformity; no AVN
* ORIF via volar approach + corticocancellous bone graft - AVN without humpback deformity
* Vascularized bone graft via volar or dorsal approach - AVN with humpback deformity
* Vascularized medial femoral condyle bone graft via volar approach
What is the blood supply to the lunate?
[Kienbock’s Disease, 2016]
- Volar and dorsal branches from the radial artery
* Volar is dominant and 20% of the time it is sole supply - Gelberman described 3 patterns:
* ‘Y’ = 59%
* ‘I’= 31%
* ‘X’ = 10% - Gelberman hypothesized that a lunate at risk has only one arterial supply or dorsal and volar supply but no anastomoses

What is the classification system for Kienbock’s disease?
[J Hand Surg 2016:41(5);630][JAAOS 2001;9:128-136]
Lichtman Classification
- Stage I
- Normal xray
- MRI decreased signal T1
- Bone scan positive
- Stage II
- Lunate sclerosis
- Stage IIIa
- Lunate collapse (no scaphoid rotation)
- Carpal height maintained
- Stage IIIb
- Lunate collapse
- Carpal collapse
- Scaphoid rotation (hyperflexed, RS angle >60o)
- Cortical ring sign
- Capitate migrates proximal
- Decreased carpal height
- Stage IV
- Pancarpal arthritis (Kienbock’s disease advanced collapse)

What are the treatment options for Kienbock’s disease based on stage of disease?
[J Hand Surg 2016:41(5);630]
Stage I
- Nonoperative (3 months immobilization)
Stage II
- Radial shortening osteotomy
- If ulnar negative or neutral
- Capitate shortening
- If ulnar positive
- (vascularized bone graft)
Stage IIIa
- Same as Stage II
- Vascularized bone graft (dorsal pedicle)
- 4,5 ECA graft
- Vascularized pisiform
- Free vascularized medial femoral condyle
Stage IIIb
- Scaphocapitate fusion
- STT fusion
- PRC
Stage IV
- PRC
- Total wrist arthrodesis

What are the components of the TFCC?
[JBJS REVIEWS 2015;3(1):e1]
- Articular disc
* Extends between the volar and dorsal radioulnar ligaments (hammock) - Meniscus homologue
- Volar and dorsal radioulnar ligaments
* Superficial and deep (ligamentum subcruentum)
* Major stabilizers of the DRUJ - Sheath of ECU
- Ulnar capsule (ulnar collateral ligament)
* Arises from the ulnar styloid and extends between the ulnotriquetral ligament and the ECU sheath - Ulnolunate and ulnotriquetral ligaments (volar)

What is the function of the TFCC?
[JBJS REVIEWS 2015;3(1):e1]
- Stabilize ulnocarpal joint
- Stabilize DRUJ
- Transmits load from carpus to ulna
- Assists with wrist mechanics
What is the blood supply of the TFCC?
[JBJS REVIEWS 2015;3(1):e1]
- Peripheral 20% vascularized
- Central avascular
- Ulnar artery and anterior interosseous artery
* Palmar and dorsal branches

What is the innervation of the TFCC?
[JBJS REVIEWS 2015;3(1):e1]
- Ulnar nerve
- PIN
What is the classification of TFCC tears?
[JAAOS 2012;20:725-734] [JBJS REVIEWS 2015;3(1):e1]
Palmer classification
- Type 1 = traumatic
- 1A – central
- 1B – peripheral avulsion from ulnar styloid
- 1C – volar ulnocarpal ligaments
- 1D – radial attachment
- Type 2 = atraumatic
- 2A – TFCC wear (no tear)
- 2B – TFCC wear with lunate or ulnar head chondromalacia
- 2C – 2B + TFCC perforation
- 2D – 2C + LT ligament perforation
- 2E – 2D + ulnocarpal arthrosis

What are the physical examination findings/tests in a TFCC tear?
[JBJS REVIEWS 2015;3(1):e1]
- Prominent ulna
- Fovea sign
- Palpation of the depression volar between ulnar styloid, FCU and pisiform
- Tenderness suggests:
- Tear of ulnotriquetral ligament
- Foveal disruption of TFCC
- Chondromalacia of ulnar aspect lunate
- Suggestive of ulnocarpal impaction
- Ulnocarpal stress test
* Ulnar deviation with axial loading in alternating supination and pronation - Positive grind test
* Clicking, crepitus or pain with passive supination and pronation - Lunotriquetral shuck test
* Pain and laxity when examiner grasps the pisiform/triquetrum and lunate with opposite hands and translates volar and dorsal
Ballottement test
dorsal and palmar displacement of ulna with wrist in ulnar deviation
positive test produces pain
Nakamura’s ulnar stress test
ulnar deviation of pronated wrist while axially loading, flexing and extending the wrist
positive test produces pain
fovea test
used to evaluate for TFCC tear or ulnotriquetral ligament tear
performed by palpation of the ulnar wrist between the styloid and FCU tendon
What imaging is indicated for TFCC tears?
[JBJS REVIEWS 2015;3(1):e1]
- Radiographs
- Neutral rotation PA and lateral
- PA in ulnar and radial deviation
- Pronated PA clenched-fist views
- MRI/MRA
What are the findings during wrist arthroscopy?
[JBJS REVIEWS 2015;3(1):e1]
- Trampoline test
- Probe is used to test central disc tautness and rebound ability
- Laxity suggests detachment from one or more insertion points
- Hook test
- Traction applied to ulnar-most aspect of TFCC
- Ability to pull the TFCC radial and upward suggests foveal attachment disruption
What is the treatment of TFCC tears?
[JBJS REVIEWS 2015;3(1):e1]
- Nonoperative
* Most tears are initially treated nonoperative - Operative
- Contraindications:
- Severe OA
- Previous infection
- Severe osteoporosis of ulnar head
- Open
- Indicated when fixing distal radius fracture or surgeon not familiar with arthroscopy
- Arthroscopic
- Palmar 1A – debridement
- Palmer 1B, C, D – repair
- Transosseous or suture anchor fixation
- Ulnar positive wrists
- Perform ulnar shortening osteotomy or wafer procedure at time of TFCC repair
- Better outcomes
- Perform ulnar shortening osteotomy or wafer procedure at time of TFCC repair

What is ulnocarpal impaction?
[Hand Clin 26 (2010) 549–557]
- Mechanical abutment of the distal ulna with the carpus
- Usually associated with positive ulnar variance
What are the causes of positive ulnar variance?
[Hand Clin 26 (2010) 549–557]
- Congenital
- Physiologic
- Madelung
- Acquired
- Distal radius malunion
- Radial head excision
- Premature physeal closure of radius
- Post-wrist fusion
What is the resulting pathology from ulnocarpal abutment?
[Hand Clin 26 (2010) 549–557]
- Degenerative TFCC tears (Palmer 2A-E)
- Chondromalacia of ulnar head
- Chondromalacia of ulnar lunate
- Chondromalacia of triquetrum
- LT ligament perforation
What results in dynamic ulnar positive variance?
[Hand Clin 26 (2010) 549–557]
- Pronation
- Grip
[Do pronated grip view to elicit positive ulnar variance]
What is the treatment for ulnocarpal impaction?
[Hand Clin 26 (2010) 549–557]
- Nonoperative
- Rest
- Immobilization
- Activity modification
- NSAIDs
- Corticosteroid injections
- Operative
- Ulnar shortening osteotomy
- Technique
- Subcutaneous approach to the ulna
- Osteotomy at junction of distal and middle 1/3
- Compression plate
- Volar surface preferred
- Goal of 0 to -1mm ulnar variance
- Advantages
- Addresses ulnar styloid carpal impaction concomitantly
- Decreases dorsal subluxation of distal ulna
- Larger shortening can be achieved compared to wafer
- Stabilizes ulnar ligament complex
- Preferred if associated LT ligament injury
- Disadvantages
- Nonunion
- Hardware irritation
- Technique
- Wafer procedure
- Technique
- Open or arthroscopic
- Resection of thin wafer of dome of ulnar head
- Advantage
- Less revision compared to shortening osteotomy (hardware removal)
- No nonunion
- Disadvantage
- Limit resection to 2-3mm
- Does not address associated ulnar styloid carpal impaction
- Does not improve dorsal ulnar subluxation
- Does not tighten ulnar ligament complex
- Technique
What are the arthroscopic portals for wrist arthroscopy?
[JAAOS 2012;20:725-734] [JBJS REVIEWS 2015;3(1):e1]
1-2 portal
- Dorsum of the snuffbox just radial to the EPL tendon
- Risk = radial artery
3-4 portal
- Between the EPL and the EDC, just distal to the Lister tubercle
- Risk = EPL or EDC tendons
- Main viewing portal
4-5 portal
- Between the EDC and EDM, in line with the ring metacarpal, slightly proximal to the 3-4 portal
- Risk = EDC or EDM tendon
- Main radiocarpal instrumentation portal
6-R portal
- Radial side of the ECU tendons
- Risk = dorsal sensory branch of ulnar nerve
6-U portal
- Ulnar side of the ECU tendons
- Risk = dorsal sensory branch of ulnar nerve
Radial midcarpal (MCR)
- Radial side of the third metacarpal axis proximal to the capitate in a soft depression between the capitate and scaphoid
- Risk = ECRB and EDC tendons
Ulnar midcarpal (MCU)
- 1 cm distal to the 4-5 portal, aligned with the fourth metacarpal, at the lunotriquetral-capitatehamate joint
- Risk = EDC and EDM tendons
STT portal
- Midshaft axis of the index metacarpal just ulnar to the EPL at the level of the STT joint
- Risk = radial artery and small branches of radial nerve
Volar ulnar portal
- Interval between flexor tendons and FCU and the ulnar neurovascular bundle
- Risk = ulnar artery
Volar radial portal
- Just radial to the FCR tendon at the proximal wrist flexion crease
- Risk = radial artery and median nerve

What are the primary stabilizers of the thumb MCP joint?
[JAAOS 2011;19:287-296]
- Ulnar collateral ligament (UCL)
- Radial collateral ligament (RCL)

What are the eponymous names for the UCL and RCL injuries?
[JAAOS 2011;19:287-296]
- Chronic UCL = gamekeeper’s thumb
- Acute UCL = skiers thumb
- RCL = reverse gamekeeper’s thumb

What are the components of the UCL and RCL ligaments?
[JAAOS 2011;19:287-296]
- Proper collateral ligament
* Taut in flexion - Accessory collateral ligament and volar plate
* Taut in extension

Where is the typical thumb UCL and RCL ligament injured?
[JAAOS 2011;19:287-296]
- UCL
- Proximal phalanx avulsion (90%)
- Midsubstance and metacarpal avulsion less common
- RCL
* Variable, more common proximal at metacarpal
What is a Stener lesion?
[JAAOS 2011;19:287-296]
- Distal edge of the avulsed UCL is displaced proximal to the adductor aponeurosis
* Blocked from reapproximation to its insertion on the proximal phalanx - Surgical management is recommended

Which injury, UCL or RCL, is more prone to joint subluxation of the MCP joint?
[JAAOS 2011;19:287-296]
- RCL
* Adductor pollicis inserts on the proximal phalanx and ulnar sesamoid creating an ulnar and volar deforming force - Assess with anterior drawer test
* >3mm displacement volar is more common with RCL injury
How do you grade collateral ligament tears?
[JAAOS 2011;19:287-296]
Grade 1
- Sprain with no joint instability
Grade 2
- Incomplete tear with asymmetric joint laxity
- Instability does not meet the criteria for a complete tear
- Characterized by increased laxity with a firm end point, or an incomplete tear
Grade 3
- Complete tear with joint instability
- Laxity of >35° in 0° and 30° of flexion
- Or 15° greater than that of the contralateral side
- Laxity of >35° in 0° and 30° of flexion
How is instability of the thumb MCP joint defined?
[JAAOS 2011;19:287-296]
Joint stressed at zero degrees of extension and 30° flexion
- Instability = deviation of the proximal phalanx on the metacarpal head of >30-35°
What is the recommended management of thumb collateral ligament injuries based on grade of injury?
[JAAOS 2011;19:287-296]
Grade 1 and 2
- Nonoperative
- Cast or splint x 4 weeks
- Grip and pinch strengthening after 6 weeks
Grade 3
- Surgical
- Acute collateral ligament injury = repair
- Avulsion from proximal or distal insertion
- Suture anchor repair
- Midsubstance tear
- Direct repair
- Avulsion from proximal or distal insertion
- Chronic collateral ligament injury (>3 weeks)
- No arthritis
- Ligament reconstruction with free graft (palmaris longus)
- Arthritis = arthrodesis
- No arthritis
- Acute collateral ligament injury = repair
What is the direction of trapeziometacarpal (TM) dislocation?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
Dorsoradial

What is the reduction maneuver for a thumb CMC/TM dislocation?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- Traction
- Abduction
- Pronation
- Dorsal pressure on the base of the metacarpal (anatomical snuffbox)
What is the treatment of thumb CMC/TM dislocation?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- CRPP
- Intermetacarpal pinning
- Transarticular pinning
- Open/arthroscopic reduction if closed reduction not attained
* Repair capsule/ligament protect with pinning

What is the pattern of injury in a Bennett fracture dislocation?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- Anteromedial (volar-ulnar) fragment
- Smaller (less articular surface area)
- Nondisplaced, attached to volar oblique ligament
- Metacarpal fragment
- Larger (greater articular surface area)
- Displaced
- Proximal, dorsal and radial

What are the deforming forces of the metacarpal fragment in a Bennett fracture?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- APL = proximal, dorsal, radial
- Adductor pollicis = narrowing of 1st web space

What is the reduction maneuver for a Bennett fracture dislocation?
[J Hand Surg 2009;34A:945–952.]
- Traction
- Abduction
- Pronation
- Pressure to the metacarpal base (dorsal to palmer)
**TrAPP/TAPP

What is the open approach for fixation of a Bennett fracture?
[J Hand Surg 2009;34A:945–952.]
Wagner approach
- Junction of the glabrous and nonglaborus skin
- Elevate thenar muscles and perform capsulotomy
What is the management of Bennett fracture dislocations?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- Large anteromedial fragment
* Open reduction and direct screw fixation - Small anteromedial fragment
* CRPP – transarticular or intermetacarpal - Irreducible or intra-articular gap >2mm [J Hand Surg 2009;34A:945–952.]
* Open reduction

What is the pattern of injury in a Rolando fracture?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
‘T’ or ‘Y’ pattern
- Extra-articular fracture separating metadiaphysis from epiphysis and a vertical fracture separating the epiphysis into two fragments
- Central joint depression may be present

What are the deforming forces on the fragments in a Rolando fracture?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- Adductor pollicis – metadiaphysis adduction (narrows 1st web space)
- APL – dorsoradial displacement of radial articular fragment
- Ulnar articular fragment does not displace due to volar oblique ligament

What is the treatment of a Rolando fracture?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
Open or arthroscopic reduction
- Followed by provisional K-wire fixation and miniplate fixation or definitive k-wire fixation

What is the pattern of injury of a comminuted fracture of the 1st metacarpal base?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
Often regarded as a Rolando fracture, worst stage
What is the treatment of a comminuted 1st metacarpal base fracture?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- Intermetacarpal blocked pinning
- External fixation

What is the pattern of injury of an extra-articular fracture of the 1st metacarpal base?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- Proximal fragment that remains reduced
- Metacarpal fragment displaces into adduction

What degree of displacement is acceptable for nonoperative management of an extra-articular 1st metacarpal base fracture?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
<30° of angulation
- >30o results in unacceptable narrowing of the 1st web space
What is the treatment of extra-articular fractures of the 1st metacarpal base?
[J Hand Surg Eur Vol. 2015 Jan;40(1):42-50]
- <30° of angulation = closed reduction and casting
- >30° of angulation = CRPP (intermetacarpal)
What is the usual deformity of proximal phalanx fractures?
Apex volar
- Proximal fragment flexes due to interosseous attachments
- Distal fragment extends due to extensor central slip

What is the usual deformity of middle phalanx fractures?
- Apex dorsal if fracture proximal to FDS insertion
- Apex volar if fracture distal to FDS insertion

What is the acceptable alignment of phalanx fractures for conservative care?
- No rotation
- <10-15° angulation
- <2mm shortening
What is the treatment for proximal phalanx fractures?
- Nonoperative (most)
* Stable fractures with acceptable alignment = buddy taping - Operative
* K-wire
* Eaton-Belsky pinning through the metacarpal head
* Screws
* Plates and screws

What is acceptable alignment for metacarpal head fractures?
No articular displacement acceptable
What is acceptable alignment for metacarpal neck fractures?
- Index and middle = <10-15°
- Ring = <40°
- Small = <60°
- No rotation

What is acceptable alignment for metacarpal shaft fractures?
- Index and middle = <10°
- Ring = <20°
- Small = <30°
- No rotation
What are the stabilizing structures and anatomy of the PIP joint?
[JAAOS 2013;21:88-98]
- Volar plate
- Anatomy
- Volar base of the middle phalanx to the proximal phalanx via swallow-tail extensions called checkrein ligaments
- Function
- Primary = resists hyperextension
- Secondary = resists lateral stability
- Collateral ligaments
- Proper collateral ligament
- Anatomy
- Pit on lateral side of proximal phalanx head to volar 1/3 of middle phalanx base
- Function
- Primary = resists lateral displacement in flexion
- Anatomy
- Accessory collateral ligament
- Anatomy
- Lateral proximal phalanx head and proper collateral ligament to the volar plate
- Function
- Primary = resists lateral displacement in extension
3. Volar base of middle phalanx
- Primary = resists lateral displacement in extension
- Anatomy
- Function = resists dorsal displacement

What is the mechanism of injury for dorsal fracture dislocation of the PIP joint?
[JAAOS 2013;21:88-98]
- Extension (most common)
- Axial load of a flexed PIP joint

What structures are injured in a dorsal fracture dislocation of the PIP joint?
[JAAOS 2013;21:88-98]
- Volar plate rupture or avulsion of volar base off middle phalanx
- Volar avulsion of variable size (loss of buttress effect)

How is the stability of a dorsal PIP fracture dislocation determined?
[JAAOS 2013;21:88-98]
- Stable
- Articular surface <30% involvement
- Clinical stability = stable throughout ROM
- Tenuous
- Articular surface = 30-50% involvement
- Clinical stability = Requires ≤30° of PIP flexion to maintain reduction
- Unstable
- Articular surface >50% involvment
- Clinical stability = Requires >30° of PIP flexion to maintain reduction

What is the management of dorsal PIP fracture dislocations based on stability?
[JAAOS 2013;21:88-98]
- Stable
* Buddy taping - Tenuous
- Extension block splinting (if no hinging)
- Prevents extension of the PIPJ into the range where it is unstable while permitting motion within the stable range
- Unstable
- Operative options
- Extension block pinning or transarticular pinning +/- percutaneous pinning of large fracture fragment
- Indicated when concern for closed reduction failure or digit will not accommodate extension block splint (swollen, short, small digit)
- Dynamic distraction and external fixation (Suzuki splint)
- ORIF
- Large fragments
- Volar plate arthroplasty
- Comminuted and impacted volar fragment
- <50% articular surface involvement
- Hemi-hamate resurfacing arthroplasty
- Comminuted and impacted volar fragment
- >50% articular surface involvement
- Extension block pinning or transarticular pinning +/- percutaneous pinning of large fracture fragment

What is the mechanism of injury for volar PIP fracture dislocation?
- Hyperflexion
- Axial load of an extended PIP joint

What structures are injured in a volar PIP fracture dislocation?
- Central slip rupture or avulsion of dorsal base of middle phalanx
- Dorsal avulsion of variable size

What is the management of volar PIP fracture dislocation?
- Stable and small minimally displaced fracture
- <50% articular surface and <2mm displacement
- PIP joint splinting
- Stable and large or displaced fracture
- >50% articular surface and >2mm displacement
- CRPP or ORIF
- Unstable with minimally displaced fracture
* Dynamic distraction and external fixation

What is the most common site of OA in the hand?
[JAAOS 2018;26:562-571]
Index DIP
- 2nd most common = thumb basal joint
What hand is most commonly affected by OA?
[JAAOS 2018;26:562-571]
Nondominant
What are the 5 articulations of the pantrapezial joint?
[JAAOS 2018;26:562-571]
- Trapeziometacarpal (CMC joint)
* Most commonly affected articulation - Trapeziotrapezoid
- Scaphotrapezial
- Scaphotrapezoidal
- Trapezial-index metacarpal

What are the stabilizers of the thumb basal joint?
[JAAOS 2018;26:562-571]
- Static
- Deep anterior oblique “beak” ligament
- Tightens with thumb abduction, pronation and extension
- Dorsal “deltoid” ligaments
- Strong
- Volar ligaments
- Weak
- Dorsoradial ligament
- Ulnar complex
- Ulnar collateral
- Volar TM ligament
- Dorsal TM ligament
- Dynamic
- Extrinsic
- FPL, APL, EPB, EPL
- Intrinsic
- APB, Adductor pollicis, FPB, opponens pollicis

Deficiency of what ligament was thought to lead to CMC arthritis?
[JAAOS 2018;26:562-571]
Anterior oblique ligament

What are risk factors for thumb basal joint arthritis?
[JAAOS 2018;26:562-571]
- Advanced age
* 36% >80y vs. 6.6% 40-49y - Female
- Ligamentous laxity/ higher Beighton score
- Occupations
* Repetitive finger use or heavy manual labour - Post-traumatic
- Intra-articular fracture
- Traumatic ligamentous instability
What is the characteristic deformity at the thumb in basal thumb OA?
[JAAOS 2018;26:562-571]
- Metacarpal adduction
- MCP hyperextension
What are the special tests for thumb basal joint arthritis?
[JAAOS 2018;26:562-571]
- CMC grind test
* Pain with axial load and rotation around the thumb axis - CMC subluxation test
* Pain or instability with attempted subluxation - Decreased pinch strength
What is the best radiographic view for CMC arthritis?
[CORR course]
Roberts view
- Thumb hyperpronated and flat on the cassette

What is the association of thumb basal joint arthritis and carpal tunnel syndrome?
[JAAOS 2018;26:562-571]
- 30% of patients with CTS have thumb basal joint arthritis
- ≤30% of patients with thumb basal joint arthritis have CTS
What is the radiographic classification of thumb basal joint arthritis?
[JAAOS 2018;26:562-571]
Eaton-Littler
- Stage I
- Normal joint with widening
- Synovitis, effusion, ligamentous laxity
- Normal joint with widening
- Stage II
- Mild joint narrowing
- Mild subchondral sclerosis
- Subchondral cysts and/or periarticular debris
- Stage III
- Severe joint space narrowing
- Subchondral sclerosis/cysts
- Larger periarticular debris
- Stage IV
- Involves scaphotrapezial joint

What is the treatment of thumb basal joint arthritis?
[JAAOS 2018;26:562-571]
- Nonoperative
* Exercise therapy, heat, education, magnetotherapy, adaptive equipment, orthoses, NSAIDs, corticosteroid injections - Operative
- Joint preserving options described (Stage I/II)
- 1st metacarpal extension osteotomy
- Arthroscopy and debridement
- Imbrication of the dorsoradial capsule
- Volar beak ligament reconstruction
- Joint sacrificing options described (Stage III/IV)
- Trapeziectomy
- Trapeziectomy and ligament reconstruction and tendon interposition (LRTI)
- Distraction hematoma arthroplasty
- Suture suspension arthroplasty
- Prosthesis
- CMC arthrodesis

What are the advantages of simple trapeziectomy vs. trapeziectomy and LRTI for treatment of thumb CMC arthritis?
[JAAOS 2018;26:562-571]
None
- No benefit to pain or function
- No difference in adverse events
[No differences shown between trapeziectomy with or without LRTI]
What tendons make up the flexor tendons of the hand?
[JAAOS 2018;26:e26-e35]
- FDS
- FDP
- FPL
What is the blood supply to the flexor tendons?
[JAAOS 2018;26:e26-e35]
- Dorsal portion
* Two vinculae supplied by radial and ulnar artery - Volar portion
* Minimal direct blood supply (synovial diffusion)

Describe the pulley system for FDP and FDS tendons?
[JAAOS 2018;26:e26-e35]
A1 - MCP volar plate
A2 - proximal phalanx
C1 - between A2-A3
A3 - PIP volar plate
C2 - between A3-A4
A4 - middle phalanx
C3 - between A4-A5
A5 - DIP volar plate

What flexor pulleys are most important for digital motion and power?
[JAAOS 2018;26:e26-e35]
A2 and A4

Describe the pulley system for FPL?
[JAAOS 2018;26:e26-e35]
A1 - MCP volar plate
Oblique pulley - proximal half of proximal phalanx
A2 - IP volar plate

What pulley is most important for preventing bowstringing of the FPL?
[JAAOS 2018;26:e26-e35]
Oblique pulley

What are the 5 zones of the flexor tendon system?
[JAAOS 2018;26:e26-e35]
Zone 1 - distal to FDS insertion
Zone 2 - FDS insertion to proximal A1 pulley
Zone 3 - proximal A1 pulley to distal transverse carpal ligament
Zone 4 - carpal tunnel
Zone 5 - proximal transverse carpal ligament to musculotendinous junction

What are the fundamentals of tendon repair in flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Easy placement of sutures in the tendon
- Secure knots
- Smooth juncture of the tendon ends
- Minimal gapping
- Minimal interference with tendon vascularity
- Sufficient strength
The fundamentals of tendon repair are achieved by adhering to the following principles?
[JAAOS 2018;26:e26-e35]
- Minimal tendon handling to minimize adhesion
- Strength of repair is proportional to the number of core sutures and caliber of suture
- Core sutures should be 7-10mm from tendon edge
- Dorsal placement is biomechanically advantaged
- Epitendinous (peripheral) suture improves:
- Strength
- Minimizes gapping
- Reduces CSA
- Decreases gliding friction
- Locking loops increase tensile repair
- Internal knots have decreased strength
What is the treatment for Zone 1 flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Injury to FDP tendon (laceration or avulsion)
* Closed avulsion = Jersey Finger - Leddy classification
- Type I - retraction into palm
- Both vincula disrupted
- Repair within 7 days
- Worst prognosis
- Type II - retraction to PIP joint
- Repair within 6 weeks
- Type III - retraction to distal A4 pulley (bony avulsion)
- Repair within 6 weeks
- (Type IV) - fracture and avulsion of FDP tendon from bony avulsion
- (Type V) - distal phalanx fracture along with bony avulsion of FDP
3. Repair options - Stump >1cm = primary end-to-end repair
- Stump <1cm = suture anchor or pullout buttons
- Chronic = consider treating nonoperative or DIP fusion if symptomatic

What is the treatment for Zone 2 injuries flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Injury to FDP and/or FDS tendon
* FDP injured more often due to superficial nature - “No Man’s Land” due to poor outcomes
- Repair options:
- ≤50% = debride to prevent catching at pulleys
- >50% = repair

What is the treatment of Zone 3 flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Injury to FDP and/or FDS
- Good prognosis due to absence of fibrosseous sheath
- Repair options
* Direct surgical repair

What is the treatment for Zone 4 flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Often associated with median or ulnar nerve injury
- “Spaghetti wrist”
* Multiple tendons and median nerve involved - Repair options:
* Carpal tunnel release and direct repair

What is the treatment for Zone 5 flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Often associated with nerve or vascular injury
- Good outcomes

What are the disadvantages associated with active rehab vs. passive rehab for flexor tendon injuries?
[JAAOS 2018;26:e26-e35]
- Active protocols:
* Higher risk of rupture - Passive protocols:
- Adhesion
- Contracture
- Decreased ROM
- Poor gliding between FDP and FDS
What are the pathways and phases of (flexor) tendon healing?
[JAAOS 2018;26:e26-e35]
Pathways
- Intrinsic = tenocytes within the tendon
- Extrinsic = inflammatory cells outside the tendon
- Implicated in adhesions/scarring
Phases
- Inflammatory (0-72h)
- Strength of repair is equivalent to strength of suture repair
- Proliferative (72h-4 weeks)
- Type III collagen laid down
- Strength increases
- Remodeling phase (>4 weeks - 112 days)
- Type I collagen laid down
- Strength increases
- Does not reach preinjury

What are the pathological changes that occur in the tendon and the tendon sheath in trigger finger (stenosing tenosynovitis)?
[JAAOS 2015;23:741-750]
- Tendon sheath
- Fibrocartilaginous metaplasia
- Cartilage degradation
- Vascular ingrowth
- Tendon
- Chronic degenerative tears
- Absence of inflammatory cells

What pulley is most commonly involved in trigger finger?
[JAAOS 2015;23:741-750]
A1 pulley

What digits are the most commonly involved in trigger finger?
[JAAOS 2015;23:741-750]
Ring finger and thumb
What are the risk factors for development of trigger finger?
[JAAOS 2015;23:741-750]
- Female
- Diabetes
- RA
- Crystalline arthropathy
- Thyroid disease
- Renal insufficiency
- Overuse
What condition is commonly associated with trigger finger?
[JAAOS 2015;23:741-750]
Carpal tunnel syndrome
- >60% of patients with trigger digits demonstrate clinical or electrodiagnostic evidence of median nerve compression at the wrist
What is the management of trigger finger?
[JAAOS 2015;23:741-750]
- Nonoperative
- Therapy
- Splinting
- NSAIDs
- Corticosteroid injections
- Commonly used firstline
- Operative
- Percutaneous release of A1 pulley
- Open release of A1 pulley
What are reasons for persistent triggering following release of A1 pulley?
[JAAOS 2015;23:741-750]
- A0 pulley stenosis
* Tight band of superficial palmar aponeurosis proximal to A1 - FDP entrapment at FDS decussation
* In patients with diabetes, RA - A3 pulley entrapment
What is the cause of pyogenic flexor tenosynovitis (flexor tendon sheath infection)?
[JAAOS 2012;20:373-382]
- Puncture wound (most common)
- Staph aureus (most common)
What are the four cardinal signs of Kanavel in flexor tendon sheath infections?
[JAAOS 2012;20:373-382]
- Symmetric swelling of entire digit
- Tenderness along course of tendon sheath
- Semiflexed posture
- Pain with passive extension of digit

What is the treatment of pyogenic flexor tenosynovitis?
[JAAOS 2012;20:373-382]
- Nonoperative
- Indication
- Early presentation <48 hours of symptom onset
- Initiate empiric antibiotics
- If no improvement in 12-24 hours proceed with surgical I&D
- Operative
- Open I&D
- Indication
- Advanced, atypical or chronic cases
- Midaxial or palmer zig-zag incision
- Indication
- Closed tendon sheath irrigation
- Two incisions
- 1 oblique incision just proximal to A1 pulley and midaxial incision at DIP joint
- Angiocath is threaded into sheath at proximal incision and penrose drain at distal incision
- Irrigation is performed in OR then intermittently at bedside
- Two incisions
- Continuous closed irrigation
- Same as closed but irrigation is continuous

What are the etiologic associations with Dupuytren disease?
[JAAOS 2011;19:746-757]
- Northern European
- Caucasian
- Male
- Family history
* Autosomal dominant - Advanced age
- Smoking
- Alcohol
- Local trauma
- Local infection
- Diabetes (type I > type II)
- Epileptic medication
- Manual labour
What cell is responsible for the contractile nature of Dupuytren disease?
[JAAOS 2011;19:746-757]
Myofibroblasts
What is the most commonly involved cord in the hand in Dupuytren disease?
[JAAOS 2011;19:746-757]
Pretendinous cord
[Normal fascial bands become pathologic cords]

What ligaments are typically spared in Dupuytren Disease?
[JAAOS 2011;19:746-757]
- Transverse ligament of the palmar aponeurosis
2. Cleland ligament
What are the clinically relevant cords in Dupuytren Disease?
- Pretendinous cord = MCP contracture
- Central cord = PIP contracture
- Lateral cord = PIP or DIP contracture
- Natatory cord = web space contracture
- Spiral cord = displaces NV bundle superficial and to midline
* MCP and PIP contracture

What is the clinical presentation of Dupuytren Disease?
[JAAOS 2011;19:746-757]
- Palmer skin pitting and thickening
* Fibrosis of Grapow fibres - Painless nodules
- Cords which may become adherent to overlying skin (resemble flexor tendons)
- Positive table top test
* Unable to place palm flat on table in presence of MCP joint contracture (>30°)

What is the most commonly affected digit in Dupuytrens Disease?
[JAAOS 2011;19:746-757]
Ring finger
- Followed by:
- Small
- Long
- Index
- Thumb
What joint is affected first in Dupuytren Disease?
[JAAOS 2011;19:746-757]
MCP before PIP
How does Dupuytren disease progress?
[JAAOS 2011;19:746-757]
Palmer to digital
Patients with bilateral Dupuytren disease commonly have Garrod nodes (knuckle pads over PIP) which is associated with increased incidence of which ectopic diseases?
[JAAOS 2011;19:746-757]
- Peyronie disease (penile fibromatosis)
- Ledderhose disease (plantar fibromatosis)

What is the nonoperative management of Dupuytren Disease?
[JAAOS 2011;19:746-757]
- Observation
- Percutaneous fasciotomy (needle aponeurotomy)
- Collagenase
- Enzymes derived from Clostridium histolyticum
- Injection followed by manipulation
- Outcomes:
- Good short term results
- Higher recurrence [CORR course]
- Complications
- Edema, contusion, pain, skin tear, lymphadenopathy
- Rare – CRPS, flexor tendon rupture
What is the operative management of Dupuytren Disease?
[JAAOS 2011;19:746-757]
- Indications
* ≥30° MCP joint contracture
* >15° PIP joint contracture - Techniques
* Fasciotomy
* Limited fasciectomy
* Dermofasciectomy
* Radical fasciectomy (healthy and diseased fascia)
What are the features of rheumatoid hand and wrist?
[JAAOS 2006;14:65-77][Orthobullets] [AAOS comprehensive review 2, 2014]
- Rheumatoid nodules
- Caput ulnae syndrome
- Dorsal subluxation of the distal ulna
- Prominent ulnar head
- Carpal deformity
* Classically, palmar translation, ulnar translation, supination, radial deviation - DISI or VISI
- Arthritis
* Usually progression from DRUJ, radiolunate/radioscaphoid, pancarpal arthritis - Extensor tendon
- Tenosynovitis
- EDQ rupture
- EDC rupture
7. Flexor tendon - Tenosynovitis
- Carpal tunnel syndrome
- FPL rupture over prominent distal scaphoid and trapezium (Mannerfelt syndrome)
- FDS and FDP rupture
8. Ulnar drift
9. Volar subluxation of proximal phalanx to MCP joint
10. Swan neck deformity
11. Boutonniere deformity
What is the management of caput ulna syndrome?
[JAAOS 2006;14:65-77] [J Hand Surg Am. 2011;36(4):736–747]
- Darrach procedure
- Favoured in low demand, elderly patients
- Main concern in RA is ulnar translation of carpus (weak ligamentous support)
- Sauve-Kapandji
- Favoured in active, younger patients
- Main concern in RA is less predictable fusion
What is the management of carpal deformity and arthritis in rheumatoid wrist?
[JAAOS 2006;14:65-77] [J Hand Surg Am. 2011;36(4):736–747]
- Total wrist arthrodesis (first line)
* Plates may be less attractive given tenuous soft tissue - Partial arthrodesis if midcarpal preserved
- Radiolunate
- Scaphoradiolunate
- Total wrist arthroplasty
What is the management of MCP joint subluxation and ulnar deviation in rheumatoid hand/wrist?
[J Hand Surg Am. 2011;36(4):736–747]
- Early disease (MCP joint reducible)
- Synovectomy with cross intrinsic transfer
- Ulnar intrinsic lateral band released and transferred radial aspect of adjacent digit (proximal phalanx)
- Late disease
- MCP joint arthroplasty
- Silicone arthroplasty with centralization of extensor tendon
- Imbrication of radial sagittal bands and release of ulnar sagittal bands
- Silicone arthroplasty with centralization of extensor tendon
- Volar plate arthroplasty
- Indicated if MCP joint too small to accept silicone implant

What is the management of extensor tendon rupture in rheumatoid hand/wrist?
[J Hand Surg Am. 2011;36(4):736–747]
- Address the underlying cause
* Remove ulnar head (Darrach or SK) and synovectomy - Tendon transfers
* EDM/little EDC rupture- End-to-side transfer to intact ring EDC
* Little and ring rupture - EIP transfer
* Little, ring and middle rupture - EIP transfer to little and ring
- End-to-side middle to intact index EDC
- End-to-side transfer to intact ring EDC
What are 3 other reasons for loss of MCP joint extension in RA (other than extensor tendon rupture)?
[J Hand Surg Am. 2011;36(4):736–747]
- Extensor tendon subluxation between metacarpal heads
- MCP joint dislocation
- PIN palsy secondary to elbow joint involvement (rare)
What is the management of the thumb in RA?
Thumb MCP fusion
Who is the ideal candidate for reimplantation of digits/wrist?
[JAAOS 2015;23:373-381]
- Young, healthy
- Sharp mechanism
- Minimal tissue destruction and contamination
What are the indications for reimplantation?
[JAAOS 2015;23:373-381]
- Thumb amputation
- Multiple digit amputation
- Amputations at or proximal to the palm
- Pediatric finger amputation at any level
- Single digit amputation in Zone I (relative)
What are the relative contraindications for reimplantation?
[JAAOS 2015;23:373-381]
- Single digit amputation through Zone II
- Severe crush, mangled or contaminated amputation
- Segmental injuries
- Prolonged warm ischemia time
- Medically unfit
What are two clinical poor prognostic signs for reimplantation?
[JAAOS 2015;23:373-381]
- Red line sign
- Red stripe along the mid lateral aspect of the avulsed digit
- Represents hemorrhage along the vessel
- Ribbon sign
- Tortuous, spiraled blood vessels are seen
- Indicates significant intimal injury

What are other poor prognostic factors for reimplantation?
[JAAOS 2015;23:373-381]
- Avulsion mechanism
- Smoker
- Diabetes
- Prolonged ischemia
What is the recommended initial management of a traumatically amputated digit/part?
[JAAOS 2015;23:373-381]
- Wrap in saline-moistened gauze
- Place in sealed plastic bag
- Place on ice
What are the classic maximum ischemia times for reimplantation?
[JAAOS 2015;23:373-381]
- Digit = 12 hours warm and 24 hours cold
- Hand and proximal = 6 hours warm and 12 hours cold
What are the anatomical features of the extensor mechanism of the finger?
[JAAOS 2015;23:623-632]
- 3 muscles contribute to finger extension
- EDC
- Lumbrical
- Dorsal interosseous
2.The EDC is stabilized by the sagittal bands at the level of the MCP joint
- Radial and ulnar sagittal bands arise from the EDC dorsally and travel volarly to insert on the volar plate and volar periosteum of the proximal phalanx
- The sagittal bands help to extend the MCP joint through a ‘lasso’ effect
- The EDC tendon trifurcates into a central slip and two lateral slips which join the lumbricals to form the conjoint lateral band
- The central slip inserts into the dorsal base of the middle phalanx
- The lumbricals arise from the FDP tendons
- Distal to the PIP joint, the radial and ulnar conjoint lateral bands are anchored dorsally by the triangular ligament and volarly by the transverse retinacular ligament, preventing volar and dorsal subluxation
- Overlying the distal aspect of the middle phalanx, the radial and ulnar conjoint lateral bands come together to form the terminal tendon.
- The terminal tendon inserts into the base of the distal phalanx and extends the DIP joint

What is a boutonniere deformity and what is the etiology?
[JAAOS 2015;23:623-632]
- Deformity = flexion of PIP joint and extension of DIP joint
- Etiology
- Disruption of central slip and triangular ligament
- Allows the conjoint lateral bands to sublux volarly with PIP joint flexion
- Lateral bands migrate proximally increasing tension on the terminal tendon causing DIP hyperextension
- Mechanism of injury
- Blunt trauma
- Open laceration
- Volar dislocation of PIP joint

What is a pseudo boutonniere deformity?
[JAAOS 2015;23:623-632]
- Hyperextension injury to the PIP joint leading to PIP joint flexion contracture
- Cause is scarring of volar plate and capsule
* Central slip and triangular ligament remain intact - Distinguished based on Elson and Boyes tests
- Treatment differs as it requires aggressive mobilization
What is the most reliable test to diagnose a Boutonniere deformity?
[JAAOS 2015;23:623-632]
Elson test
- The examiner holds the PIP joint in 90° of flexion and instructs the patient to actively extend the DIP joint
- With an intact extensor mechanism, holding the PIP joint in 90° of flexion causes slack in the lateral bands as they are held distally by their attachments to the central slip
- The patient is unable to generate any extension power at the DIP joint
- With a boutonnière injury, flexion of the PIP joint does not advance the lateral bands distally secondary to disruption of the central slip
- Tension is generated in the terminal tendon because of the disrupted central slip
- Therefore, the patient is able to generate an abnormal amount of active extension at the DIP joint with the PIP joint held in flexion

What is the classification system of Boutonniere deformity?
[JAAOS 2015;23:623-632]
Burton Classification of Boutonniere Deformity
- Stage I
- Supple, passively correctable deformity
- Stage II
- Fixed contracture
- Contracted lateral bands
- No joint involvement
- Stage III
- Volar plate and collateral ligament contractures
- Intra-articular fibrosis
- Stage IV
- Volar plate and collateral ligament contractures
- Intra-articular fibrosis
- Plus proximal interphalangeal joint arthritis

What is the management of Boutonniere deformity?
[JAAOS 2015;23:623-632]
- Nonsurgical
- Burton Stage I
- Extension splinting of PIP joint for 4 to 8 weeks to allow the central slip to heal
- Active DIP flexion exercises are performed multiple times daily
- Burton Stage II
- As long as full passive PIP joint extension is achieved
- Surgical
- As long as full passive PIP joint extension is achieved
- Burton Stage I
- If acute and not amenable to splinting
- Pin PIP joint in extension
- Open injuries
- Large bony avulsions
- Chronic injuries
- Proceed with caution
- First, achieve full passive PIP joint extension
- Second, do 1 of 3 options:
- Terminal tendon tenotomy (simplest) OR
- Tendon rebalancing technique OR
- Staged reconstruction
- Alternative option
- Arthrodesis
What are Burton’s principles for treatment of chronic Boutonniere Deformity?
[JAAOS 2015;23:623-632]
- Surgical treatment of boutonnière deformities should be done only by experienced hand surgeons
- Surgical treatment is rarely necessary for supple boutonnière deformities
- Preoperative and postoperative therapy programs are an essential part of surgical treatment
- Tendon procedures should be done after full passive PIP joint extension has been achieved
* Procedures may need to be staged, with tendon rebalancing following a PIP contracture release - If arthritic change is present, tendon rebalancing should be combined with implant arthroplasty or arthrodesis
- Flexor function should not be jeopardized in an attempt to achieve full extension
- All procedures involve rebalancing the extensor mechanism to divert force from the DIP joint to the PIP joint

What is a Swan Neck deformity and what is the etiology?
[JAAOS 2015;23:623-632]
- Deformity = hyperextension of PIP joint and flexion of the DIP joint
- Etiology
* Extrinsic- Due to excessive extension force on the middle phalanx
- Eg. terminal tendon rupture, wrist or MCP joint flexion contractures
- Intrinsic
- Eg. terminal tendon rupture, wrist or MCP joint flexion contractures
- Due to intrinsic muscle tightness
- Eg. chronic volar MCP joint subluxation, ischemic contractures
- Articular
- Eg. chronic volar MCP joint subluxation, ischemic contractures
- Due to injury or degeneration of volar PIP joint structures
- Eg. post traumatic, inflammatory, generalized laxity, FDS disruptions
- Due to excessive extension force on the middle phalanx
***NOTE: treatment differs for inflammatory vs. posttraumatic swan neck deformity

What test is used to assess for intrinsic muscle tightness (ie. in Swan neck deformity)?
[JAAOS 2015;23:623-632]
Bunnell test
- A patient with intrinsic muscle tightness will have a decrease in passive and active flexion of the PIP joint with the MP joint held in extension

What is the classification of Swan Neck deformities?
[JAAOS 2015;23:623-632]
Type I
- Full ROM
- No intrinsic tightness
- No functional limitations
Type II
- Intrinsic tightness
Type III
- Stiff PIP in all positions of the MP joint
- Joint space preserved
Type IV
- Severe arthritic change
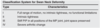
What are the management options for post-traumatic Swan Neck deformities?
[JAAOS 2015;23:623-632]

What are the 3 types of polydactyly of the hand?
[JAAOS 2018;26:75-82]
- Postaxial (ulnar) polydactyly (most common)
- Preaxial (radial) polydactyly
* Involves the thumb - Central polydactyly (rare)
What is the classification of postaxial polydactyly?
[JAAOS 2018;26:75-82]
Type A
- Well-formed digit with osseous connection
Type B
- Incompletely-formed with soft tissue connection
- Nonfunctional

What is the management of a Type B postaxial polydactyly digit?
[JAAOS 2018;26:75-82]
- Suture ligation
- Vessel clip
- Surgical excision
* Avoids complications of ligation/clip including neuroma, cyst, residual stump, infection

What is the timing of management of a Type B postaxial polydactyly digit?
[JAAOS 2018;26:75-82]
- If performed at bedside = as early as feasible
- If performed in OR = 12 months

What is the management of a Type A postaxial polydactyly digit?
[JAAOS 2018;26:75-82]
Surgical excision
- If digit arises from the MCP joint UCL, ulnar capsule and abductor digit minimi are transferred to the base of the proximal phalanx of retained digit

What is the Wassel classification of preaxial polydactyly?
[JAAOS 2018;26:75-82]
Type I
- Bifid distal phalanx
Type II
- Duplicated distal phalanx (2nd most common)
Type III
- Bifid proximal phalanx
Type IV
- Duplicated proximal phalanx (most common)
Type V
- Bifid metacarpal
Type VI
- Duplicated metacarpal
Type VII
- Any triphalangeal thumb

When should reconstruction occur for polydactyly?
[JAAOS 2018;26:75-82]
12-24 months
What are the goals of surgical management of preaxial polydactyly?
[JAAOS 2018;26:75-82]
- Aligned joints and physis with longitudinal axis
- Stable joint
- Balanced tendon pull
- Prevent nail deformity
What are the surgical options for management of preaxial polydactyly?
[JAAOS 2018;26:75-82]
- Excision and reconstruction (most common)
- Usually the less developed radial digit is excised, preserving the native UCL
- Radial collateral ligament and abductor pollicis longus is transferred to the proximal phalanx
- Bilhaut-Cloquet procedure
* Central portions of the duplicated digits are resected and the retained peripheral portions are closed down and combined to form a single thumb
* Wassel type II, III or IV - On-top plasty
- Considered when one thumb may be better developed proximally while the other thumb is better developed distally
- The well developed portions of each are combined into a single digit

What is the management of central polydactyly?
[JAAOS 2018;26:75-82]
Addressed on an individual basis
What is ulnar tunnel syndrome?
Characteristic Findings
Sites of Compression
Causes of Entrapment
Provocative Tests
EMG Findings
[JAAOS 2017;25:e1-e10]
- Entrapment of the ulnar nerve at the wrist
* Guyon’s canal - Characterized by:
- Numbness/paraesthesisa of the small and ulnar half of ring finger
- Ulnar palm and dorsum are spared
- Intrinsic muscle weakness
- Thenar spared
- Sites of compression:
- Zone I - proximal to bifurcation
- Motor and sensory
- Zone II - deep motor branch
- Motor only
- Zone III - superficial sensory branch
- Sensory only
- Causes of entrapment:
- Hook of hamate fracture
- Ganglion
- Adhesions
- Anomalous muscles
- Ulnar artery thrombosis or aneurysm
5. Provocative tests: - Tinels at the wrist
6. What are the EMG findings? - Prolonged motor/sensory latencies across wrist but sparing of the dorsal and palmar cutaneous branches and FDP/FCU

What are the borders and contents of the Canal of Guyon?
[JAAOS 2017;25:e1-e10]
Borders:
- Lateral – hook of hamate
- Medial – pisiform
- Roof – palmar carpal ligament
- Floor – transverse carpal ligament
Contents
- Ulnar nerve and artery/vein

What is carpal tunnel syndrome?
Carpal tunnel borders
Carpal tunnel contents
Characteristic features
Causes
Provocative Maneouvers
EMG findings
[JAAOS 2007;15:537-548]
- Compression of the median nerve at the wrist
- Borders of the carpal tunnel:
* Ulnar border – hook of hamate and pisiform
* Radial border – scaphoid tubercle and trapezium
* Roof – transverse carpal ligament
* Floor – concave arch of the carpals - Contents of the carpal tunnel (10):
* Median nerve (1)
* FPL tendon (1)
* FDS tendons (4)
* FDP tendons (4) - Characterized by:
- Numbness and paraesthesia in median nerve distribution
- Palmar cutaneous branch spared
- Night pain
- Grip and pinch weakness
- Loss of hand dexterity
- Thenar atrophy
5. Causes: - Idiopathic
- Women > men
- Anatomic
- Trauma
- Persistent median artery
- Infection
- Ganglion cyst
- Tumor
- Systemic
- Obesity
- Drug toxicity
- Alcohol
- Diabetes
- Hypothyroidism
- RA
- Primary amyloidosis
- Renal failure
- Pregnancy
- Exertional
- Repetitive use of hands and wrists
- Repeated impact to palm
- Operation of vibratory tools
- Provocative maneuvers:
- Phalen test – wrist flexion
- Reverse Phalens test – wrist extension
- Tinels
- Median nerve compression test
- EMG findings:
- Distal motor latency >4.5ms
- Distal sensory latency >3.5ms
- Order electrodiagnostic tests if clinical and/or provocative tests are positive and surgical management is being considered

What are the 4 variations in branching of the recurrent motor branch of the median nerve?
[JAAOS 2017;25:e194-e203]
- Extraligamentous (distal to TCL) – 50%
- Subligamentous (deep to TCL) – 30%
- Transligamentous (through TCL) – 20%
- Ulnar take off (distal to TCL)

What is the treatment of carpal tunnel syndrome?
[JAAOS 2009;17:397-405]
- Nonoperative
- First line
- Early surgery is an option when there is clinical evidence of median nerve denervation or the patient elects to proceed directly to surgical treatment
- Options:
- Splinting
- Corticosteroid injections
- Oral steroid
- Ultrasound
- Operative
- Complete division of the transverse carpal ligament
- The wrist should not be immobilized postoperatively
- Technical pearls: [JAAOS 2017;25:e194-e203]
- Safest location for a longitudinal incision
- Long-ring web space axis
- Distal dissection limit
- Palmar fat pad (found at distal TCL)
- Safest location for a longitudinal incision
What are the complications associated with carpal tunnel release?
[JAAOS 2007;15:537-548]
- Pillar pain
- Pain along edges of incision at thenar and hypothenar eminences
- Most common complication of open
- Laceration of palmar cutaneous branch of median nerve
* 2nd most common complication of open - Incomplete release of TCL
* Most common complication of endoscopic - Injury to motor branch
- Hypertrophic scar
- Tendon adhesion
- Infection
- Wound hematoma
- Finger stiffness
- Recurrence


