GYN Flashcards
2hr GTT
What are the dia criteria for DM?
Fasting:
- Normal is <100
- 100-125 is c/w Pre DM
- >=126 DM
2hr
>=200 is DM
140-199 PreDM

- The coccygeous muslce overlies the SSL and is a component of the lev ani muscle. T or F
- Components of the levator ani
- in a transobturator sling, what muscles are passed?
- Origin of Inf and superior epigastric arteries.
- True, but not a part of the lev ani
- Puborectalis, pubococcugeons, ilieo coccygeous
- photo
- They include the superior epigastric artery and the musculophrenic artery, both originating from the internal thoracic artery, and the inferior epigastric artery and the deep circumflex iliac artery, both originating from the external iliac arteries.

How do you manage anticoagulated patients preoperatively?

- AGC on PAP
- Atypical Endometrial cells on PAP
- You did the work up for AGC and it was all negative. What do you do now?
- What if they has specified AGC favor neoplasia and the results were all normal?
- Colpo, Ecc, Ebx if >=35 or risk factors
- Ecc + EBx (if normal, then do a colpo…start with looking at the most obvious glandular source)
- If no CIN2+, AIS, or CA -> cotest @1 and 2 yrs
- Excise

- What do you do if AIS on cytology?
- What do you do if AIS on biopsy?
- What do you do after CKC if margins positive?
- What do you do after CKC if margins negative?
- After a hyst, what is the follow-up?
- How does this all chage for fertility preservation?
- Colpo, ECC, Ebx if >35yo or risks!
- Everyone gets a cone!
- If margins positive, you re-excise even if a hyst is planned to rule out cervical CA.
- If margins negative, proceed to hysterectomy.
- HPV based test q1yr x3, then q3yr x25 yrs
- Once negative margins obtained, cotest + ECC q6m x3 years, then annually x2yrs. Hyst when done childbearing.

- What do you do after HSIL is confirmed on biopsy?
- What is the follow up if negative margins?
- What if positive margins?
- Excisional procedure.
- Negative margins: HPV based test at 6 months, if neg HPV based test annually x3 yrs, then Q3y X 25 years
- Repeat excision, or colpo + ECC @ 6 months

- How do you manage a young woman with CIN3?
- How do you manage CIN2 in <25?
- >=25 + fertility desired?
- Lets say <25yrs…what do we do and at what interval?
- How about >25yrs and desiring fertility?
- If results remain abnormal for __yrs, excision.
- TREAT!
- OBS is preferred if less than 25 years.
- If >25 and fertility desired, OBS is acceptable.
- Colpo + cyto @ 6m and 12m
- Colpo + HPV based test @ 6m and 12 m
- 2yr of persistent CIN2, RX!

- How do we screen HIV patients?
- 2019 ACS screening?
- When do we DC screening?
- What is the screening following a hyst for cervical disease (CIN2-3 / AIS)?
- Start w/in 1 year of sexual activ ity, latest 21yo, 3 in a row, then space q3yrs, can use HPV at 30 but never spaces > 3yrs
- <25yo no screening; 25-65 1ty HPV Q5 preferred, cotest q5 and cyto alone q3 also acceptable
- >65 if prior adequate screen if >=25 yrs from CIN2 or greater (this includes AIS)
- HPV based test q1yr x3, then q3yr x25 yrs
- t
ASCCP Unsatisfactory Cyto:
- What generally guides management?
- HPV neg…
- HPV +…unk genotype and >25
- HPV+..16/18
- HPV status
- Repeat in 2-4m, colpo if unsatisfactory again
- Colpo
- Colpo

CIN3 risk is used as the benchmark for the ASCCP 2019 quidelines.
- At what threshhold and above is colpo recommnended?
- At what threshhold can you treat expideted or colpo?
- How about expedited Rx?`
- >=4%
- 25-59
- 60-100%
Athlete Triad
- Definition
- 1st line Rx
- Menstrual dysf, low energy availability, and low BMD
- Corretion of the energy imbalance, ok to supp Ca/D, no OCP or bisphosphos or E
BUT, if evidence of dec bone density, could use Patch low doese E + cyclic P (no OCP, no bisphos…ocps can mask menses, these lowe doses will not)
Bartholin cyst in >40yo requires excision. T or F
True
- MOA of Ella.
- Plan B Kg above which efficacy drops
- T or F: highest risk of post sterilization regret is young age.
- Patch has dec effacy after __kg.
- SPRM; inhibits follic rupture
- BMI >25 (165lb)
- T
- 90kg
Bladder Injury
- Non-trigonal injury <1cm
- Non-trigonal injury >1cm
- Trigonal injury
- Expectant management (foley 1 week)
- Primary repair (foley for 1-2 weeks)
- Running non-locked x1
- Embricating x1
- Retrograde fill w/ 300cc (vs cysto)
- Foley 2 weeks
- Plain vs CT urogram
- How to treat intraductal papilloma?
- What is the appearance of ductal ectasia?
- Pagets? Rx?
- What is the algorithm for nipple discharge work-up? What characteristics warrant age-appropriate imaging immediately
- T or F, in workup of discharge, always get an US, and a mmmo if >30 as well. T or F
- Periductal mastitis is associated w/ what risk factor?
- Inflammatory breast ca rx
- Excise.Generally, intraductal papillomas are surgically excised when they are identified by core biopsy due to the risk of areas of ductal carcinoma in-situ or atypia within the lesion.
- The discharge typically is very thick and sticky and either green or black in color but occasionally can become sero- sanguineous or bloody. Ductal ectasia is not associated with breast carcinoma, but the surrounding tissue may become fibrotic, causing a confusing palpable density.
- Paget disease of the breast is an intraductal carcinoma, which presents as a scaly skin lesion similar to eczema appearing on the nipple and spreading to the areola. Ulceration can be present, and there may be a clear yellowish exudate with crusting. Breast conserving surgery with radiation, mastectomy
- See photo.
- t
- smoking
- mastectomy, axillary dissection, neoadjuvant chemotherapy, and radiation therapy. Lymph node involvement is present in the majority of cases, even in the absence of physical exam findings. This explains why axillary dissection is indicated as part of treatment, and sentinel lymph node biopsy is not appropriate.

- Fibrocystic breast dz:
How does it present? How to rx?
Patient will be a woman 30 – 50-years-old
Complaining of intermittent breast pain and tenderness that peak before each menstruation
Ultrasound would show dense, prominent, fibroglandular tissue with cysts but no discernable mass
Most commonly caused by fluctuating estrogen levels during menstrual cycles
Treatment is well-fitting supportive bras, applying heat to the breasts or over-the-counter pain relievers. NOT OCPS.
Comments: Most common lesion of the breast. Fibrocystic changes are generally benign and do not increase risk for breast cancer
- Mammo recs from ACOG
- Clinical breast exam from ACOG
- offer at 40, recommend at 50
- Offer: Q yr at 40; Q1-3yr if 20-39
- ___therapy is the first-line treatment for patients with eating disorders.
- Second-line RX: __.
- Bupriprion is CI in patients with __ .
- CBT
- SSRI
- Bulimia; + seuzires
Calcium Recs if <50? >50?
Vid d recs <50? >50?
19-50: 1000mg; 600 D
51-70: 1200mg; 600 D

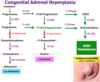
- 95% of cases of CAH are caused by ___ deficiency. This results in decreased levels of ___ & ___ and increased levels of ___.
- There are two types, classic, and non-classic. How do we test for it?
- Inheritance pattern?
- How does a neonate present? How do we treat it?
- What other enzyme def can casue virilization of a female?
- 21a, aldost/cortisol, androgens
- Use 17OP level, may need acth stim test
- Autosomal recessive
- hypotension, dec NA/gluc, inc K; vom, diarr, dec weight: FLUIDS, LYTES, STEROIDS
- 21-alpha-hydroxylase, 11-beta-hydroxylase, or 3-beta-hydroxysteroid dehydrogenases. resulting overproduction of androgens
Remember than in a patient with PCOS, late onset adult CAH is in the differential! 17ohp FASTING, FOLLICULAR PHASE, MORNING). level is greater than 200 ng/dLand less than 800 ng/dL, further testing with a cosyntropin (ie, adrenocorticotropic hormone) stimulation test shouldbe performed. A baseline 17-OHP greater than 800 ng/dL confirms the diagnosis and further testing is not necessary.
Rx for chancroid
azithro 1g
Or cftx 250mg
Isolation of the bacteria to confirm the disease is technically challenging and not always available, therefore, the diagnosis is primarily clinically made

- Chancroid geographic region
- Causative organism?
- Diagnosis (physical exam and lab)
- Rx
- Causative organism for LGV and geographic region.
- Diagnosis (physical exam and lab).
- RX
- Causative organism for GI/donovanosis
- Dx (physical exam and lab).
- Rx
- Of all ulcerative lesions, which does not have associated LAD?
- Africa/Caribbean
- H. Ducrey
- Eryhtematous base with clear borders, grey exudate + unilateral LAD (suppurative); special culture or PCR; school of fish
- Azithro 1g PO (or CFTX, or Cipro or Erythro
- Chlamydia L1-L3; tropics and subtropics (africa, india)
- Painless ulcer; + unilateral LAD (fibrosis + strictures); chlamidya serology + PCR
- Doxy 3w
- Kelbsiella
- Painless ulcer, bleeds easily, NO LAD; donovan bodies on microscopy
- Doxy 3wk
- No LAD with GI
Colon Cancer Screening Modalities
- Colonoscopy @ age __ q __ yrs. Stop at __ yrs.
- Flex sig q __ yrs.
- Fecal Immunochemical Test (FIT)
- FOBT
- What if you are high risk…when do you start?
- What if IBD?
- IN WHI, the E/P arm showed dec rates of colon Ca. T or F
- When do you start if 1st degree rel had cc?
- Colonoscopy @ age 45/50 q 10 yrs - 75yrs old.
- Flex sig q 5 yrs.
- Fecal Immunochemical Test (FIT) q1 year.
- FOBT (3 samples from 3 consec stools) q1year.
- 10yr before index case, or age 40.
- surveillance colonoscopy should be initiated 8 – 9 years after the onset of symptoms in individuals with a personal his- tory of inflammatory bowel disease and performed every 1–2 years thereafter.
- T. No effect in the E arm alone .
- at 40 or 10 yrs before dx
























