GU Flashcards
(90 cards)
Name the cell of origin for adenomatoid tumors
mesothelial cell
IF a prostate needle core bx with a conventional adenocarcinoma containing the following patterns: 4-65% 3-30% and 5-5% what is the final gleason score?
9
Name an IHC stain that highlights the basal cell layer in the prostate
p63
What is the most common malignancy of the spermatic cord in adult males
liposarcoma
Invasive urothelial carcinoma of bladder: what pT stage does invasion of muscularis propria correspond with?
T2
Name a premalignant lesion in the prostate
High-grade prostatic intraepithelial neoplasia
Name 4 features of balanitis xerotica obliterans
- orthokeratotic hyperkeratosis - atrophy of epidermis - homogenous collagen in upper dermis - lymphoplasmacytic lichenoid inflammatory infiltrate
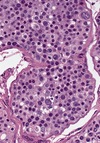
Name 3 positive stains in classic seminoma
- PLAP - Oct 4 - C-kit
What is the common genetic alteration seen in adult germ cell tumors of the testis?
- isochromosome 12p
Name 4 conditions associated with renal cell carcinoma
- Birt-Hogg-Dube - Tuberous sclerosis - Von Hippel Lindau - End-stage renal disese
If RCC grows directly into the adrenal gland (ipsilateral) what is the pT stage?
- pT4
What is the characteristic morphologic finding in malakoplakia?
- Michaelis-Guttman bodies
Name 4 variants of urothelial carcinoma with poor prognosis
- Sarcomatoid urothelial carcinoma - Micropapillary urothelial carcinoma - Nested urothelial carcinoma - Mixed urothelial and small cell carcinoma
What stage is a prostatic carcinoma if it invades the base of the seminal vesicle?
- pT3b
Describe 3 gleason grade 4 histologic patterns
- Glomerulations - Chains of fused glands - Poorly formed small glands
Name 3 mimics of invasive prostatic adenocarcinoma
- glandular atrophy - atypical adenomatous hyperplasia - cowper glands - granulomatous prostatitis - seminal vesicle in bx
Name 3 entities associated with intratubular germ cell neoplasia
- Cryptochordism - Embryonal carcinoma - Mixed germ cell tumor
Testicular bx/smears for fertility: LIst 2 patterns showing spermatozoa and 3 lacking spermatozoa
HAVE spermatozoa: hypospermatogenesis, obstruction of sperm excretory ducts NO spermatozoa: germ cell maturation arrest, sertoli cell only, testicular cell atrophy
Name 3 patterns seen in urothelial carcinoma in situ
- Clinging/denuding - Small cell - Pagetoid - Undermining
Discuss the pathogenesis of nephrogenic adenoma
- Increased incidence after organ transplantation and immunosuppression - In renal transplant recipients, derived from exfoliated and implanted renal tubular cells in the urinary tract ● In other patients, appears to be metaplastic and not a neoplasm ● Associated with inflammation, calculi, chronic catheterization, exstrophy, interstitial cystitis, intravesical thiotepa, malakoplakia, surgery
List the histologic features of nephrogenic adenoma
- Tubular, cystic, polypoid, papillary and polypoid patterns - Cuboidal to low-columnar epithelium with scant cytoplasm and occasional hobnail cells common - Basement membrane hyalinzed around tubules - inflammatory infiltrate and stromal edema - minimal atypia, no necrosis
Name the anatomic sites where nephrogenic adenoma might be found
- Urinary bladder - Ureter - Urethra - Renal pelvis
List stains that can help differentiate nephrogenic adenoma from prostatic adenocarcinoma
- Nephrogenic adenoma: cytokeratins, racemase, Pax8, EMA, PAX2 - Prostatic adenocarcinoma: racemase, PSA
What is the WHO classification of urothelal lesions?
Flat: hyperplasia, atypia of unknown significance, urothelial dysplasia, urothelial carcinoma in-situ Papillary: papillary hyperplasia, papilloma, papillary urothelial neoplasm of low-malignant potential, papillary urothelial carcinoma low grade r, papillary urothelial carcinoma high grade, invasive urothelial carcinoma