General OBGYN - SJS Flashcards
(475 cards)
Briefly discuss the pathophysiology of the different signs/symptoms of pre-eclampsia

What are the diagnostic criteria of pre-eclampsia

What are the risk factors for pre-eclampsia?

What are the symptoms of pre-eclampsia?
WHat is the management of eclampsia?

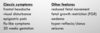
What is the clinical picture of HELLP?

What do we learn from the 12 week USS?
Identifies viability of the foetus
Estimates gestation and date of delivery
Identifies and characterizes multiple gestation
Identifies risk factors for Down Syndrome as part of 1st trimester screening.
Identifies major fetal abnormalities like anencephaly
What is the amnion and the chorion?
The chorion is the placenta
The amnion is the fluid sack of foetal urine
What can we tell from the 20 week scan?
Morphology scan –> head to toe check for anatomical abnormalities
Growth (4 measurements)
Locates the placenta (5% of women will have a low lying placenta)
Amniotic fluid volume
May also perform umbilical artery doppler and/or cervical length if indicated
What % of women have a low lying placenta at their 20 week ultrasound scan?
What is the management?
What % of women have placenta previa?
5%
Follow up ultrasound at 34 weeks, explain to mother that it’s like blowing up a baloon so the placenta is likely to move to a safe spot
0.5% go on to have placenta previa
What is the cut off amniotic fluid index for oligo and polyhydramnios?
Polyhydramnios - AFI >25
Oligohydramnios - AFI < 5 - 10
What are the causes of oligo and polyhydramnios?

What is Potter’s sequence?
A triad of consequences of oligohydramnios (regardless of the cause)
Clubbed feet
Pulmonary hypoplasia
Cranial anomalies
Why is general anaesthetic avoided in pregnant women?
Higher risk of aspiration
The uterus is pushing up on the abdominal cavity + progesterone relaxes the lower oesophageal sphincter
What are you looking for on foetal artery doppler?
Two things:
1) In suspected RhD, the flow velocity of the middle cerebral artery can be used to quantify foetal anaemia. This is the equivalent of listening for a flow murmur in an anaemic adult
2) diastolic flow patterns in the umbilical artery can demonstrate high resistance in the placenta vasculature and assess the risk for pre-eclampsia, IUGR and abruption
What are some indications for foetal growth and wellbeing studies in later pregnancy?
GDM
Gestational HTN
Suspected IUGR (uterus too small)
Decreased fetal movements felt (FMF)
History of pregnancy loss or complication in late pregnancy
What can you do to assess foetal wellbeing in later pregnancy?
SAM BLACK

What are the causes of a long or short symphysiofundal height?

At what gestational age is the foetal heart beat usually detectable on USS?
Often at 6 weeks
in 80% of cases at 12 weeks
90% at 13 weeks
At what gestational age do women typically start feeling foetal movements?
What can delay this?
Foetal movements begin to be felt between weeks 15 and 25
They can be masked by an anterior lying placenta
Why are babies of mums with GDM big?
GDM –> hyperglycaemia –> increased release of insulin and insulin like growth factor from the foetus –> hepatomegaly and increased growth
What are the components of the APGAR?

How do you interpret a CTG?
DR C BRaVADO

What causes Braxton Hicks contractions?
Around week 37 progesterone levels start to drop, but oestrogen levels remain high. This higher ratio of oestrogen to progesterone causes the uterus to be more sensitive to other hormones (notably oxytocin released from the anterior pituitary) which stimulate contractions. This effect can cause some women to experience some weak contractions in late pregnancy, either called “false labour contractions” or “Braxton-Hicks contractions”.















































































