Gargi & Emma's Notes - Obstetrics Flashcards
When do most caeses of asthma in pregnancy occur?
Most occur between 24-36 weeks
What is asthma?
Chronic inflammatory airway disease characterized by:
- variable reversible airway obstruction,
- airway hyper-responsiveness
- bronchial inflammation
What are the clinical signs of asthma in pregnancy?
- Wheeze, breathlessness, cough – worse in morning and at night
- Precipitating factors – e.g. cold, drugs (beta blocker, NSAIDs), exercise
- Atopic history
- Tachypnoea, use of accessory muscles, prolonged expiratory phase, polyphonic wheeze, hyperinflated chest
What is classified as a severe attack of asthma in pregnancy?
Severe attack if PEFR <50%, pulse >110, RR > 25, inability to complete sentences
What is classified as a life-threatening attack of asthma in pregnancy?
Life-threatening if:
- confusion,
- coma
- cyanosis,
- PFR <33%,
- silent chest,
- bradycardia,
- hypotension,
What are the investigations for ?asthma in pregnancy?
- Chronic:
- PEFR monitoring
- Acute:
- Basic obs (incl pulse oximetry)
- PEFR
- pulse oximetry
- ABG, FBC, (WCC infection?), U&Es
- blood/sputum cultures
- CXR (exclude other diagnoses)
What is the antenatal management of chronic asthma?
Chronic management:
- Antenatal:
- MDT approach
- Reassurance that asthma medication is safe during pregnancy à continue taking as normal
- Oral corticosteroids have small increased risk of malformations
- Optimise control
- Smoking cessation
- NB stepwise approach is:
- Step 1: salbutamol PRN
- Step 2: add low-dose ICS (400mcg/day)
- Step 3: – + LABA/increase ICS to 800mcg/day
- Step 4: medium-dose ICS (2000mcg/day) + LABA (or theophylline or LTRA)
- Step 5: high-dose ICS + LABA/tiotropium
- Step 6: oral corticosteroid + high-dose ICS + LABA
NB safer to have medications than to have asthma symptoms during pregnancy
What is management of chronic asthma during labour?
- In labour:
- Continue regular medications
- Avoid bronchoconstrictors if severe asthma (e.g. ergometrine, prostaglandins)
- Ensure adequate hydration
- Regional anaesthesia favoured over GA (to decrease risk of bronchospasm)
What is management of acute asthma during pregnancy?
Acute management:
- As for non-pregnant individuals
- Monitor O2 sats, ABG and PEFR
- ABCDE approach, high-flow O2
- Nebulised salbutamol (5mg initially continuous, then 2-4hourly) +/- ipratropium (0.5mg QDS)
- IV hydrocortisone (100-200 IV) followed by oral prednisolone for 5-7d (40mg PO)
- If no improvement: IV magnesium sulphate, IV aminophylline or IV salbutamol
- Summon anaesthetic help if pt getting exhausted PCO2 increasing
- ICU admission and ventilation if severe
- Discharge when PEFR >75% of pts best, diurnal variation <25%, stable on discharge meds for 24h
What are the complications of asthma in pregnancy?
Foetal complications:
- Possible increased risk of FGR & foetal brain injury
- (due to prolonged maternal hypoxia)
- Preterm labour + birth
- Perinatal mortality
- Increased cleft lip risk
- (due to oral corticosteroids use in 1st trimester)
- Inheritance for foetus (6-30%)
What is the prognosis of asthma during pregnancy?
- Prognosis → Severity of asthma remains stable in one third, worsens in another third and improves in the last
- Well-controlled asthma has little effect on pregnancy outcome
What are the 4 hypertensive diseases in pregnancy
- Chronic hypertension
- Gestational hypertension
- Pre-eclampsia
- Eclampsia
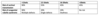
How is mild, moderate and severe HTN during pregnancy classified?
- Mild: 140-149 / 90-99
- Moderate: 150-159 / 100-109
- Severe: >=160 / >=110
Define chronic HTN in pregnancy.
Give some causes.
- Chronic hypertension: sustained BP readings ≥140/90 which occurred <20wks gestation or persists for >12wks postpartum
Essential in 90%, secondary in others
Endo – Cushing, pheo, CAH, Conn’s
Renal – RAS, chronic disease
Vasc – coarctation of aorta
RF – old age, ethnicity (Afro-Carib), obesity, smoking, diabetes, FHX, pre-eclampsia
# Define gestational HTN. Describe its aetiology.
- Gestational hypertension: sustained BP readings of ³140/90 after 20wks gestation in a previously normotensive patient, resolving by 12wks postpartum, in the absence of proteinuria
- Aetiology is unknown; may be due to upregulation of the RAAS without the drop in SVR to balance BP
What are the signs of chronic HTN in pregnancy?
Chronic –
- largely asymptomatic,
- BP may be normal in first trimester due to reduced systemic vascular resistance,
- secondary causes – renal bruits (RAS), radio-femoral delay (coarctation)
What are the Ix for ?chronic HTN in pregnancy?
- Bloods – FBC, UE, LFT, Urate, TFTs
- Urinalysis – proteinuria, catecholamines
- Renal artery USS
- Foetus – serial USS for growth
What is the Mx of chronic HTN prior to pregnancy?
- medication changed to non-teratogenic ie methyldopa, nifedipine, labetalol (NOT ACEi/ARBs),
- (increased risk of congenital abnormality/neonatal complications)
- May need reduced doses of other antihypertensives in the first half of pregnancy (when BP drops)
- Lifestyle advice
- Aim to keep BP <150/100
- aspirin 75mg of to reduce pre-eclampsia risk/IUGR.
- Monitor for pre-eclampsia, serial USS for growth, uterine artery Dopplers at 24/40 for risk
What is the Mx of mild chronic/gestational HTN in pregnancy?
- Lifestyle modification
- Consultation with dietitian; aim for limited/no weight gain in obese patients, reduce salt etc.
- Monitor BP around 1/wk to detect changes and signs of pre-eclampsia
What is the Mx of moderate chronic/gestational HTN in pregnancy?
- Lifestyle modification
- Antihypertensives
- Oral labetalol (1st line) à aim for <150/80-100; avoid labetalol in asthma
- Alternatives are methyldopa and nifedipine
- Close monitoring of BP and signs of pre-eclampsia (2x/wk); monitor for FGR
- Aim for delivery >37wks; may be earlier if complications (e.g. IUGR, development of pre-eclampsia)
What is the Mx of severe chronic/gestational HTN in pregnancy?
- Admit to hospital (until BP is <160/110)
- Antihypertensives
- IV labetalol or IV hydralazine
- Convert to oral labetalol/methyldopa when BP is under control
- BP monitoring at least 4x/d; daily urine monitoring for protein, monitor for FGR
- Consider delivery if severe refractory gestational HTN or >37wks
What is the Mx of severe chronic/gestational HTN post-natally?
- In gestational HTN, measure BP daily for 2 days, and at least once between day 3 and 5
- Reduce antihypertensives as their BP falls
- If BP remains high 6-8wks after birth à medical review
What is the prognosis of chronic HTN?
- Maternal risks: pre-eclampsia, abruption, HF, intracerebral haemorrhage
- Pre-eclampsia develops in 1/3
- –> RFs for developing superimposed pre-eclampsia are:
- renal disease,
- maternal age >40yo,
- pre-existing DM,
- multiple pregnancy,
- connective tissue disease (antiphospholipid),
- coarctation of aorta,
- severe HTN,
- BMI >35,
- previous pre-eclampsia
What are the complications of pre-eclampsia?
- Maternal – eclampsia, abruption, CVA, pulmonary oedema, cerebral oedema, renal/liver failure, DIC, HELLP syndrome (haemolysis, elevated liver enzymes, low platelets)
- Foetal – IUGR, death
What are the complications of eclampsia?
Eclampsia –
- DIC,
- permanent CNS damage (e.g. cortical blindness),
- CVA (1-2%),
- cardiac arrest,
- ARDS
- renal failure,
- death,
Define pre-eclampsia. Summarise its aetiology.
Proteinuria and hypertension in pregnancy, developing after 20/40.
- Impaired trophoblastic invasion into spinal arteries during placentation
- Resistance in uteroplacental circulation increases → leads to hypoperfusion and ischemia
- Causes release of inflammatory mediators → stimulating widespread endothelial damage, end organdysfunction, oedema
- RF - nulliparity, old mother, FHX, previous hx, pre-existing HTN, new partner, existing renal disease,diabetes, PCOS, multiple pregnancy, obesity
What are the signs of pre-eclampsia?
Pre-eclampsia –
- asymptomatic,
- headache,
- oedema,
- visual disturbance,
- RUQ pain due too liver capsule swelling;
- raised BP, oedema (facial),
- hyperreflexia,
- clonus;
- papillodema;
- RUQ tenderness;
- reduced fundal height
What are the Ix for ?pre-eclampsia?
- Bloods – FBC (low platelets, haemoconcentration), U&E, urate (renal impairment), LFT (increase transaminases), clotting
- Urine – proteinuria, MSU (exclude UTI), 24hr collection (significant protein - >0,3g/24h)
- USS – foetal growth, liquor volume, umbilical artery Doppler
What is the Mx of pre-eclampsia?
Pre-eclampsia – condition will not resolve until after delivery
- Mild/moderate – regular monitoring of BP with urinalysis, blood tests, serial USS, CTGs, antihypertensives (methyldopa, labetalol, nifedipine), delivery 37/40
- Severe/evidence of foetal compromise (NB required delivery) – antihypertensives (labetalol, nifedipine, hydralazine), seizure prophylaxis (IV magnesium sulphate), fluid restrict, fluid balance, steroids if preterm
Define eclampsia. Summarise its aetiology.
grand mal seizures on a background of pre-eclampsia.
- Unclear mechanism, theories related to cerebral vasospasm, hypertensive encephalopathy, tissue oedema, ischemia, haemorrhage
What are the signs of eclampsia?
- headache,
- epigastric tenderness,
- visual disturbances,
- oedema,
- previous findings of hyperreflexia,
- clonus;
- grand mal seizures
What are the Ix for ?eclampsia?
- Bloods FBC, clotting, U&E, Urate, LFT, G&S, ABG
- Urine – proteinuria
- Imaging – post seizure – CT head, CXR if signs
What is the Mx of eclampsia?
- Airway and Breathing – oxygen, patency, ventilate if needed
- Circulation – manage on left tilt, ensure large-bore IV access, evaluate pulse and BP
- Drugs – IV magnesium sulphate, 4g loading dose followed by 1g/h (monitor urine output, resp rate, patellar reflexes)
- Recurrent seizures – consider further bolus Mg sulphate, thiopentone, diazepam, IPPV (intermittent positive pressure ventilation), muscle relaxation
- Post seizure – assess chest, control BP (consider IV labetalol/hydralazine), strict fluid management (85ml/hr input, urine output >25mg/h), may require CVP monitoring, deliver baby when mother stabilised, consider ITU.
Define miscarriage
Involuntary, spontaneous loss of a pregnancy before 24wks gestation
- Early miscarriage is <12wks; late miscarriage is 12-24wks; (stillbirth is >24wks)
What is the aetiology of miscarriages?
Most miscarriages are due to chromosomal abnormalities in the embryo (commonly trisomy 16)
What are the different types of miscarriage?
-
Threatened miscarriage: PV bleeding but foetus is still viable
- PV bleeding, closed cervical os, foetal heartbeat visible
-
Inevitable miscarriage: miscarriage is about to occur
- PV bleeding, open cervical os, no foetal heartbeat
-
Incomplete miscarriage: some products of conception expelled and some remain
- PV bleeding, open cervical os, some products of conception expelled
-
Complete miscarriage: products of conception completely expelled
- PV bleeding symptoms resolving, closed cervical os, uterus empty on USS
-
Missed miscarriage: USS diagnosis of miscarriage in the absence of symptoms
- No PV bleeding, closed cervical os, no foetal heartbeat
-
Septic miscarriage: contents of uterus are infected, causing endometritis
- Complete or incomplete miscarriage, plus fever/rigors/uterine tenderness etc.

What are the risk factors for a miscarriage?
- Maternal age >35 (increased embryonic chromosomal abnormalities)
- Previous miscarriage
- Structural abnormalities of the uterus (fibroids, uterine septae, cervical incompetence)
- Parental chromosomal abnormalities (e.g. translocations)
- Endocrine disease (DM, thyroid disease, PCOS)
- Anti-phospholipid syndrome, other clotting abnormalities (FVL, anti-thrombin deficiency)
- Infections, incl bacterial vaginosis
- Obesity, smoking, possibly caffeine
Summarise the epidemiology of miscarriages
- Common –> 20% of pregnancies
- recurrent miscarriages affect 1% women
- Early miscarriages are more common than late miscarriages
What are the symptoms of a miscarriage?
- PV bleeding +/- clots/products of conception
- Suprapubic cramping pain
What are the signs of miscarriage O/E?
- On examination:
- General: assess for signs of shock or pyrexia
- Abdo/bimanual: uterine tenderness, exclude ectopic (adnexal mass, cervical excitation)
- Speculum: cervical os may be open, products of conception may be visible (remove if possible)
What are the signs and symptoms of a missed miscarriage?
- Missed miscarriage is asymptomatic; may be diagnosed at booking USS
What are the investigations for ?miscarriage?
- Urine pregnancy test
-
TVUSS
- Definitive diagnosis
- Miscarriage is suggested by gestational sac >25mm with no visible yolk sac or foetal pole, or CRL >7mm but no foetal heart activity
- If sac diameter is <25mm or CRL is <7mm repeat scan in 7-14d
-
Bloods: serial hCG, rhesus blood group, FBC, CRP (if pyrexial)
- hCG should be done if uncertain about miscarriage diagnosis >50% drop in 48hrs indicates failing pregnancy
What are the investigations for ?reccurrent miscarriage?
Outpatient Ix for recurrent miscarriage:
- Bloods: antiphospholipid antibodies, lupus anticoagulant, anticardiolipin antibodies, inherited thrombophilia screen
- Pelvic USS (structural abnormalities)
- Screen for bacterial vaginosis
- Karyotyping: on products of conception; parental (if POC reports unbalanced structural chromosomal abnormality)
Where should all miscarriage investigations and Tx take place?
EPAU
What is the Mx for Threatened miscarriage?
- ABC approach –> stabilise the patient, replace lost volume
- Analgesia (paracetamol)
- Close monitoring of foetus
What is the Mx for Inevitable/incomplete/missed miscarriage?
- ABC approach –> stabilise the patient, replace lost volume
- Manual evacuation of pregnancy tissue visualised in the vagina/cervical os (during speculum exam)
- Analgesia (paracetamol)
- Conservative management:
- Expectant waiting for products of conception to pass
- Must have access to 24hr emergency services
- May follow-up with repeat scans every 2wks until diagnosis of complete miscarriage is made
- Medical management:
-
Misoprostol intravaginally
- Prostaglandin E analogue –> stimulates cervical ripening and myometrial contractions
- Can go home but must have access to 24hr emergency services
- Follow-up with pregnancy test 3wks later
-
Misoprostol intravaginally
- Surgical management:
- surgical evacuation of products of conception –> ERPC (see separate topic)
- Joint 1st line with other management options (patient choice); definite indications are haemodynamic instability and infected tissue
-
Antibiotics may be given prophylactically; always given if signs of infection
- Co-amoxiclav or doxycycline (if at increased risk of Chlamydia infection)
What is the Mx for complete miscarriage?
- ABC approach –> stabilise the patient, replace lost volume
- Analgesia (paracetamol)
What is the Mx for recurrent miscarriage?
- Treat underling cause
- Psychological support and serial USS during pregnancy
What management is necessary for all types of miscarriage?
- Anti-D prophylaxis for all Rh negative patients >12wks gestation, or any gestation if surgical management
- Counselling:
- Ensure patients understand most miscarriages are not recurrent and they are not to blame
- Referral to support groups if necessary
What are the complications of miscarriage?
Complications:
- PV bleeding can be heavy and painful
- Infection
- Psychological upset
- Complications of management
- Conservative: unpredictable timing, heavy bleeding/pain, may need further intervention
- Medical: nausea/vomiting, heavy bleeding/pain, may need surgical intervention (10%)
- Surgical complications (see ERPC)
What is the prognosis of miscarriage?
Most patients: subsequent successful pregnancies; 40% chance of another miscarriage after 3
What is a biochemical pregnancy?
- a biochemical pregnancy is a positive pregnancy test 1-2 days before an expected period, then menstruation and negative pregnancy tests after.
- It is due to pregnancy failure during the early stages of implantation
What is an ectopic pregnancy?
Any pregnancy which is implanted at a site outside the uterine cavity
Which sites are the most common for implantation in ectopic pregnancies?
Most commonly occurs in the fallopian tube (98%) – mainly ampulla
- Can also occur in ovaries, cervix, interstitium of the uterus/tube or peritoneal cavity can be involved
What are the risk factors for an ectopic pregnancy?
- Previous ectopic pregnancy, PID, endometriosis, pelvic surgery (esp. reversal of sterilisation)
- Tubal damage/adhesions interfere with tubal transport
- IUD/IUS in situ
- Reduces the absolute risk of ectopic pregnancy, but increased risk if pregnancy does occur
- Assisted reproduction
- Smoking, increased maternal age (functional alterations of fallopian tube)
How common are ectopic pregnancies?
1% pregnancies are ectopic
What are the symptoms of an ectopic pregnancy?
- Lower abdominal/pelvic pain
- Amenorrhoea (4-10wks)
- PV bleeding/brown discharge (due to suboptimal hCG levels)
- Often scanty dark blood, described as prune juice
What is found in an ectopic pregnancy O/E?
- On examination:
- Adnexal tenderness, possible adnexal mass
What are the symptoms of a ruptured ectopic pregnancy?
- Haemodynamically unstable (pallor, tachycardia, hypotension, increased cap refill)
- Signs of peritonitis (rebound tenderness, guarding)
- Shoulder tip pain (referred pain due to irritation of diaphragm by blood in peritoneal cavity)
What is found O/E in a ruptured ectopic pregnancy?
- On examination:
- Cervical excitation, blood in vaginal vault/fullness in pouch of Douglas
What are the Ix for ?ectopic pregnancy?
- Urine pregnancy test (to confirm pregnancy)
-
TAUSS and TVUSS
- TAUSS is less sensitive than TVUSS; should detect intrauterine pregnancy by 6wks after last period
- Intrauterine pregnancy excludes ectopic pregnancy (unless heterotopic)
- If intrauterine pregnancy is not seen –> TVUSS
- Can confirm diagnosis
- Ectopic is seen by ‘doughnut sign’ (adnexal mass)
- Doppler USS may show increased blood flow to ectopic (‘ring of fire’)
- Free fluid suggests ruptured ectopic
- TAUSS is less sensitive than TVUSS; should detect intrauterine pregnancy by 6wks after last period
-
Serial serum hCG
- If pregnancy cannot be identified on USS (PUL)
- If >1500iU and cannot be visualised on USS, there is increased risk the pregnancy is ectopic
- <63% rise (suboptimal rise) over 48hrs suggests ectopic
- Rule out other differentials if necessary, e.g. urinalysis for UTI, USS to look for ovarian cyst accident etc.
- Group and save/crossmatch if severely compromised; assess Rh status

What is the conservative Mx for an ectopic pregnancy?
- For low-risk, haemodynamically stable, asymptomatic/minimal pain with low/decreasing hCG levels
- Monitor serial hCG levels to ensure it is falling, until undetectable
- Can go home, but ensure 24hr emergency services access and are informed of symptoms of rupture
- If increasing pain, hCG levels are not decreasing or signs of tubal rupture medical/surgical management
What is the medical Mx for an ectopic pregnancy?
Medical management:
- IM methotrexate (anti-folate agent that prevents cell division)
- For haemodynamically stable patients, ideally hCG <1500iU/L (up to 5000), unruptured, without visible heartbeat, <4cm in diameter
- For these patients, medical management is joint 1st line with laparoscopy
- Monitor serial hCG levels to ensure it is falling, until undetectable (usually takes 2-4wks)
- Patient can go home after the injection (but must have access to 24hr emergency services and be informed of signs of rupture)
- May need surgery if treatment fails
What is the surgical Mx for an ectopic pregnancy?
- Joint 1st line with medical management;
- required if:
- haemodynamic instability,
- signs of rupture,
- hCG >5000,
- foetal heartbeat on scan,
- adnexal mass >4cm
- Methods:
- Laparoscopic salpingectomy (most common): ectopic and tube are removed; doesn’t effect fertility if contralateral tube is intact
- Laparoscopic salpingostomy: cut in fallopian tube; done is damage to contralateral tube to preserve future fertility
- Laparotomy if severe haemodynamic compromise
- hCG follow-up is needed after salpingostomy until undetectable (to ensure no residual tissue)
- Anti-D prophylaxis (if Rh negative)
What are the complications of an ectopic pregnancy?
- Fallopian tube rupture
- Recurrent ectopic if tube is salvaged (15% risk in future pregnancies
What are the complications of the Tx for an ectopic pregnancy?
Complications of treatment:
- Conservative management: may rupture, may need medical/surgical treatment anyway
- Medical management: SEs of methotrexate include hepatotoxicity, nephrotoxicity, myelosuppression, teratogenesis (must use contraception for 3-6 months after)
- Surgical management: GA risks, risk of damage to bladder/bowel/ureters, DVT, bleeding, infection, salpingotomy has risk of treatment failure (persistent trophoblast)
What is the prognosis of an ectopic pregnancy?
- 5 deaths/yr in UK;
- conservative management is 80% successful;
- medical/surgical is 90% successful
What is gestational trophoblastic disease?
A group of pregnancy-related tumours
How can gestational trophoblastic disease be divided?
They can be divided into 2 main groups:
- Benign conditions: hydatidiform moles
- Malignant conditions (gestational trophoblastic neoplasia): invasive malignancies that can metastasise, e.g. invasive mole, choriocarcinoma, placental site trophoblastic tumour, epithelioid trophoblastic
What is the aetiology of gestational trophoblastic disease?
Trophoblastic tissue is the part of the blastocyst that normally invades the endometrium
- In GTD, the trophoblastic tissue proliferated more aggressively
- hCG is normally excreted in excess
What are molar pregnancies? What is their aetiology?
Molar pregnancies:
- Due to an abnormality in chromosomal number during fertilisation
- Partial mole:
- One ovum with 23 chromosomes is fertilised by 2 sperm, each with 23 chromosomes –> produces 69 chromosomes (triploidy) (69XXX/69XXY)
- Usually not viable, but if mosaicism exists (foetus has normal karyotype and triploidy is confined to placenta), foetus may be viable
- May contain some evidence of foetal parts, e.g. RBCs
- Complete mole:
- One ovum without any chromosomes is fertilised by one haploid sperm which duplicates, or less commonly, 2 haploid sperm –> leads to 46 chromosomes of parental origin alone (46XX/46XY)
- Do not contain any evidence of foetal parts
- These tumours are usually benign but can become malignant (invasive moles)
What is gestational trophoblastic neoplasia?
- Choriocarcinoma: malignancy of trophoblastic cells of placenta; usually co-exists with molar pregnancy
- Placental site trophoblastic tumour: malignancy of intermediate trophoblasts (anchor placenta to uterus); usually occurs after normal pregnancy
- Epithelioid trophoblastic tumour: malignancy of trophoblastic placental cells; mimics SCC
What are the risk factors of gestational trophoblastic disease?
- extremes of maternal age (<20 or >35),
- previous gestational trophoblastic disease,
- smoking
What is the epidemiology of gestational trophoblastic disease?
- Uncommon : 1/1000 pregnancies
- More common in Asians
What are the symptoms of gestational trophoblastic disease?
- Vaginal bleeding
- Varies from light spotting to heavy bleeding; may include passage of hydropic villi
- Missed period
- Hyperemesis (due to high hCG)
- Hyperthyroidism (rare; due to stimulation of thyroid by high hCG)
What is found O/E in gestational trophoblastic disease?
- Unusually large uterus for gestational age;
- soft, boggy consistency of uterus
What are the Ix for gestational trophoblastic disease?
- Urine pregnancy test
-
Serum hCG
- Markedly elevated; often >100,000iU/L
- Bloods: FBC (anaemia), TSH (normal), blood type
-
TVUSS
- Complete mole has snow-storm appearance of uterine cavity and absence of placental parts
- Partial mole has small placenta with partial foetal development
-
Histological examination of products of conception
- To confirm diagnosis
- Performed post-treatment on molar pregnancies, and all non-viable miscarriages (because many molar pregnancies terminate before symptoms)
- May show placental villi with irregular architecture, oedema with true villous cavitation, trophoblast hyperplasia
- Staging investigations (MRI, CT) if metastatic spread is suspected
What is the Mx of gestational trophoblastic disease?
- Referral to specialist centre (CX, Sheffield, Dundee) for treatment and follow-up
Molar pregnancy:
- Surgery:
- ERPC
- Serial serum hCG levels (persistent/rising suggests malignancy)
- Anti-D prophylaxis if mother is Rh negative
- Avoid pregnancy until 6 months of normal hCG levels
Malignant conditions or mole that has not resolved:
- Chemotherapy (methotrexate + folic acid)
What are the complications of gestational trophoblastic disease?
-
Recurrence of molar pregnancy (1%; 20% if 2 or more molar pregnancies)
- hCG samples are needed in every future pregnancy to exclude recurrence
-
Gestational trophoblastic neoplasia
- Follows 15% complete moles and 0.5% partial moles; may occur in normal pregnancy
- Diagnosis made with persistently elevated/rising hCG
- Highly malignant but sensitive to chemotherapy –> 95% cure rate
What is placenta praevia?
- Placenta abnormally attached to the lower uterine segment
How is placenta praevia classified?
Classified into complete, partial, marginal or low-lying
- Complete: placenta covers the entire internal cervical os
- Partial: placenta covers a portion of the internal cervical os
- Marginal: edge of placenta lies within 2cm of the internal cervical os
- Low-lying placenta: edge of placenta lies within 2-3.5cm of the internal cervical os
- N.B. complete and partial are AKA major placenta praevia (overlying cervical os); the others are minor placenta praevia (not covering cervical os)
What happens to the placenta in praevia as the pregnancy progresses?
- Placenta praevia often moves upwards as pregnancy progresses (because lower segment of uterus forms in 3rd trimester –> rest of myometrium moves upwards)
- More likely if low-lying placenta and marginal, some partial
What is the major risk in placenta praevia?
Placenta praevia gives increased risk of haemorrhage
- Possibly due to defective attachment to uterine wall, or damage as foetus moves into lower uterine segment
- Bleeding is from maternal circulation (not foetal) –> more likely to compromise mother if serious
What are the risk factors for placenta praevia?
- previous C-section (or other uterine scarring),
- IVF,
- previous placenta praevia,
- age >40yo,
- high parity
What is the epidemiology of placenta praevia?
- 0.5% pregnancies at term;
- much higher at 20wks
What are the symptoms of placenta praevia?
- Usually detected on routine USS
-
Painless vaginal bleeding in 2nd/3rd trimester
- Varies from spotting to haemorrhage; often intermittent bleeds increasing in frequency/intensity
- Spontaneous or provoked (e.g. by vaginal examination)
What is seen O/E in placenta praevia?
- examination:
- Breech presentation and transverse lie are common
- Foetal head high (not engaged)
- Speculum (assess bleeding)
What are the Ix for ?placenta praevia?
-
Ix for ALL antepartum haemorrhage:
- Thorough history: how much bleeding, onset, fresh/brown, SROM, provoked (post-coital), abdo pain, foetal movements, cervical smears
-
Examination:
- General: pallor, cap refill, HR, BP
- Obstetric: palpable contractions, lie and presentation of foetus, CTG
-
Assess bleeding: externally, speculum (look for blood, clots, cervical dilatation, SROM)
- Do not do bimanual in PV bleed (unless placenta praevia excluded, as risk of massive bleeding) or ruptured membranes (infection risk)
- Swabs: exclude infection if bleeding is minimal
- Basic obs
- Bloods: FBC, clotting, group and save, cross match (if transfusion likely), U&Es, LFTs (exclude PET/HELLP, organ dysfunction), Kleihauer test (if RhD -ve)
- CTG
-
USS (preferably TVUSS)
- Definitive diagnosis of placenta praevia
- Used for monitoring previous diagnosis
Which investigation must be excluded in ?placenta praevia?
- Do not do bimanual in PV bleed (unless placenta praevia excluded, as risk of massive bleeding) or ruptured membranes (infection risk)
What is the Mx of antepartum haemorrhage e.g. in placenta praevia?
- ABCDE, senior help, IV access, fluids/blood transfusion, CTG, urgent USS
- Consider antifibrinolytics (tranexamic acid)
- Admit (all women with bleeding)
- Anti-D if necessary
- If severe bleeding, not stabilised by resuscitation emergency C-section
What is the Mx of placenta praevia if identified at 20wk scan?
- Advice about pelvic rest: no penetrative sex, no douching; advise to go to hospital if bleeding
-
Re-scan at 28-32wks
- Non-complete is likely to have moved superiorly –> no further Ix
- Complete is unlikely to resolve
- If unresolved –> follow management of confirmed placenta praevi
What is the Mx of confirmed placenta praevia?
- Admit if bleeding; admission can be delayed if asymptomatic (give advice given if found at 20 week scan)
- Corticosteroids if <34wks
- Anti-D if necessary
-
Plan for delivery:
- Complete/partial placenta praevia: C-section at 37wks
- If presents in labour –> emergency C-section
- Marginal/low-lying placenta: await normal vaginal delivery
- If pre-term labour: tocolytics and corticosteroids (to allow for transfer to experienced centre); C-section if labour progresses, anti-D
- Complete/partial placenta praevia: C-section at 37wks
What are the complications of placenta praevia?
- Haemorrhage (antepartum, intraoperative, PPH)
- Preterm labour
- Need for C-section
- Placenta accreta (abnormally adherent placenta)
- Adheres to myometrium, usually in previous scar
- Prevents placental separation risk of haemorrhage (may need hysterectomy)
- IUGR, foetal death
What is the prognosis of placenta praevia?
- Non-complete placenta praevia is likely to resolve by term
- Prognosis is generally good; increased risk of recurrence in subsequent pregnancies
What is the definition of antenatal haemorrhage:?
bleeding after 24wks
What are some causes of antenatal haemorrhage?
- placenta praevia,
- placental abruption,
- marginal placental bleed,
- vasa praevia,
- uterine rupture,
- local genital causes (polyps, ectropion, infections)
What is vasa praevia?
Foetal blood vessels traverse the foetal membranes over the internal cervical os
What is the aetiology of vasa praevia?
Blood vessels may arise from a velamentous insertion or accessory placental lobes
- Velamentous insertion: normally, the umbilical cord inserts into the middle of the placenta; in velamentous insertion it inserts into the foetal membranes then travels within the membranes to the placenta
- Accessory placental lobes: vessels may be joining accessory placental lobes to the main placenta
The vessels are not protected by umbilical cord or placental tissue –> high risk of rupture when membranes rupture
- Leads to massive foetal bleeding and foetal compromise
What are the risk factors for vasa praevia?
- multiple gestation,
- IVF
What are the symptoms of vasa praevia?
- Triad of:
- Painless fresh vaginal bleeding
- Ruptured membranes
- Foetal distress
- May be detected antenatally on USS
What are the Ix for ?vasa praevia?
- CTG
-
Alkali denaturation test
- NaOH mixed with blood –> foetal Hb is resistant to denaturation with 1% NaOH present
- Determines immediately if blood if foetal (turns pink) or maternal (turns yellow)
What is the Mx of vasa praevia if detected before bleeding?
If detected before:
- Admission from 32weks (allows emergency C-section if membranes rupture)
- Corticosteroids
- Elective C-section before rupture of membranes (35-36wks)
What is the Mx of vasa praevia if detected once bleeding occurs?
- ABCDE (see full management of antepartum haemorrhage in placenta praevia)
- Immediate C-section
What are the complications and prognosis of vasa praevia?
Very high foetal mortality –> 50%, increasing to 75% if membranes rupture
What is placental abruption?
Separation of the placenta from the uterine wall before delivery of the foetus
What is the aetiology of placental abruption?
May be due to direct abdominal trauma, indirect trauma or vasospasm (e.g. cocaine use)
- Thought to occur following rupture of maternal vessels within basal layer of endometrium –> accumulation of blood and splitting of the placental attachment from the basal layer
- The detached portion is unable to function –> foetal compromise
- Bleeding is maternal and/or foetal
What are the types of placental abruption?
There are 2 types of placental abruption:
- Revealed: bleeding drains through the cervix –> vaginal bleeding
-
Concealed: bleeding remains in the uterus, usually forming a retroplacental haematoma
- Bleeding is not visible but may be severe
Abruption can involve the whole placental (total) or only part of the placenta (marginal)
- A marginal bleed is large enough to cause bleeding but not enough to cause maternal/foetal compromise
What are the risk factors of placental abruption?
- previous placental abruption,
- pre-eclampsia/HTN,
- smoking,
- cocaine,
- trauma,
- chorioamnionitis,
- oligohydramnios,
- polyhydramnios (sudden decrease in pressure when membranes rupture),
- multiple pregnancy
Which type of placental abruption is the most common?
partial is most common
What are the symptoms of placental abruption?
- Abdominal pain (due to retroplacental blood)
- Vaginal bleeding (if revealed)
- Often dark
What is seen O/E in ?placental abruption?
- On examination:
- Couvelaire uterus: woody (tense) uterus due to blood, painful
- Signs of maternal collapse
When is placental abruption considered as severe?
- Abruption is considered severe if:
- foetal/maternal death,
- foetal distress,
- preterm birth,
- IUGR,
- DIC,
- renal failure,
- hypovolaemic shock,
- need for transfusion/hysterectomy
What are the Ix for ?placenta praevia?
- Investigations for antepartum bleeding:
- Thorough history: how much bleeding, onset, fresh/brown, SROM, provoked (post-coital), abdo pain, foetal movements, cervical smears
-
Examination:
- General: pallor, cap refill, HR, BP
- Obstetric: palpable contractions, lie and presentation of foetus, CTG
-
Assess bleeding: externally, speculum (look for blood, clots, cervical dilatation, SROM)
- Do not do bimanual in PV bleed (unless placenta praevia excluded, as risk of massive bleeding) or ruptured membranes (infection risk)
- Swabs: exclude infection if bleeding is minimal
- History and exam
- Bloods: FBC, clotting, G&S, cross match, U&Es, LFTs, Kleihauer test
- CTG
-
USS
- May show retroplacental haematoma
- Poor negative predictive value don’t use to exclude abruption
What is the inital Mx of placental abruption?
Initial management:
- ABCDE, IV access, fluids/blood transfusion, CTG
- Consider antifibrinolytics (tranexamic acid)
- Admit (even without vaginal bleeding if uterine tenderness)
- Anti-D if necessary
- If severe bleeding, not stabilised by resuscitation emergency C-section
What are the next steps in Mx of a placental abruption?
Management depends on health of foetus:
- Foetal demise (death):
- Aim to minimise morbidity to mother
- Vaginal delivery (+/- IOL) if mother is stable; emergency C-section if mother is unstable
- Live foetus >34wks:
- Reassuring foetal/maternal status:
- Vaginal delivery (+/- IOL)
- Unstable foetal/maternal status:
- Emergency C-section
- Reassuring foetal/maternal status:
- Live foetus <34wks:
- Reassuring foetal/maternal status:
- Admission
- Conservative management regular USS and CTG
- Corticosteroids
- If preterm labour: consider tocolytics
- Plan for delivery at 37wks (risk of stillbirth if later)
- Unstable foetal/maternal status:
- Emergency C-section
- Reassuring foetal/maternal status:
What are the complications of placental abruption?
Complications:
- Maternal:
- Haemorrhage
- DIC
- Renal failure
- Foetal:
- IUGR
- Preterm birth
- Stillbirth, perinatal death
What is the prognosis of placental abruption?
- Foetal prognosis depends on gestational age (30% overall)
- Maternal prognosis depends on blood loss
What is acute fatty liver of pregnancy?
Fatty infiltration of hepatocytes during pregnancy, without any inflammation or necrosis
What is the aetiology of acute fatty liver of pregnancy?
Likely to be due to a mitochondrial disorder which affects fatty acid oxidation
- May lead to hepatorenal failure, DIC and hypoglycaemia
What are the risk factors for acute fatty liver of pregnancy?
- nulliparity,
- multiple pregnancy,
- pre-eclampsia,
- obesity,
- male foetus
What are the symptoms of acute fatty liver of pregnancy?
- Usually presents around 35wks (but can occur earlier or immediately after delivery)
- Nausea and vomiting
- Abdominal pain, liver tenderness
- Pruritis
- Jaundice
- Ascites
- Bleeding/coagulopathy
What are the Ix for ?acute fatty liver of pregnancy?
- Bloods: FBC (assess Hb, thrombocytopenia, WCC often high), clotting screen, LFTs (raised AST/ALT), serum bilirubin (raised), U&Es (may cause renal failure), glucose (may cause hypoglycaemia)
- USS
-
Biopsy
- Would be diagnostic (fatty infiltrates) but coagulation problems often contraindicate
What is the Mx for acute fatty liver of pregnancy?
- Supportive treatment:
- Fluid management
- Correct clotting defects (FFP, platelets, blood transfusion)
- Correct hypoglycaemia
- Prompt delivery
- Screen infants for defects in mitochondrial fatty acid oxidation
What are the complications of acute fatty liver of pregnancy?
Complications:
- DIC, bleeding
- Fulminant liver failure, renal failure
- Hypoglycaemia
- Pancreatitis
- Death (10-20% maternal mortality; 20-30% foetal mortality)
What is the prognosis of acute fatty liver of pregnancy?
Usually resolves after delivery; low recurrence rate
What is obstetric (intrahepatic) cholestasis?
Pruritic condition of pregnancy characterised by itching without a skin rash and abnormal LFTs
What is the aetiology of obstetric (intrahepatic) cholestasis?
Multifactorial aetiology –> hormonal, genetic and environmental interactions
- Due to abnormal sensitivity to the cholestatic effects of oestrogens –> build-up of bile acids in the liver –> deposition in skin and placenta –> itching
- Foetal morbidity is due to limited ability of the foetal liver to remove bile acids from blood, and the vasoconstricting effect of bile acids on placental veins
What are the risk factors for obstetric (intrahepatic) cholestasis?
- previous Hx/FHx,
- Hx Hep C,
- age >35yo,
- multiple pregnancy
What are the symptoms of obstetric (intrahepatic) cholestasis?
- Usually presents in 2nd half of pregnancy
- Intense pruritis
- Usually affects palms of hands and soles of feet; spares face
- Excoriation
- No rash
- Occasionally mild jaundice
What are the Ix for ?obstetric cholestasis?
-
Bloods:
- Bile acids (raised)
- LFTs (abnormal, esp raised AST/ALT)
- Coagulation profile (coagulopathy indicates more severe disease)
- Fasting serum cholesterol (usually elevated)
- Hep C virology
- Exclude other causes of liver dysfunction if necessary (e.g. HELLP, fatty liver of pregnancy, gallstones, etc.)
What is the Mx for obstetric cholestasis?
High-risk pregnancy; consultant-led care
Close monitoring
- Monitor LFTs weekly
- Foetal surveillance (serial growth scans, doppler USS)
Reduction of pruritis
- Antihistamines (diphenhydramine)
- Ursodeoxycholic acid (UDCA)
- Avoid tight clothing, topical antihistamine lotions, etc.
Delivery:
- IOL at 37wks (to reduce risk of a late stillbirth and maternal morbidity); earlier if foetal distress
- Deliver in labour ward with continuous CTG
- Corticosteroids for women <34wks (in case premature delivery occurs)
- 6-week follow-up to ensure LFTs return to normal
What are the complications of obstetric cholestasis?
Complications:
- Stillbirth (esp after 37wks gestation) – 2%
- Preterm labour (due to direct effects of bile salts on uterine muscle)
- Vitamin K deficiency and clotting abnormalities (liver dysfunction depletes vit K)
- Maternal morbidity (due to constant itching and sleep deprivation)
What is the prognosis of obstetric cholestasis?
Resolves after delivery but tends to recurs in subsequent pregnancies (90%)
What is varicella zoster infection in pregnancy?
Primary infection with VZV during pregnancy
What is the aetiology of varicella zoster infection in pregnancy?
Varicella zoster (HHV3) is a DNA virus responsible for:
- Chickenpox (aka varicella) –> primary infection
- Shingles (aka herpes zoster) –> reactivation (virus becomes latent in cranial nerves and dorsal root ganglia)
Transmitted by droplet spread and direct personal contact; vertical transmission
- Risk of vertical transmission is highest if primary infection occurs at <20wks or within 5 days of delivery
Incubation period is 14 days; infectious from 48hrs before rash until vesicles have crusted (usually 5 days)
Non-immune pregnant women are vulnerable to severe infection
What are the symptoms of varicella zoster infection in pregnancy?
- Primary infection:
- Fever, malaise
- Pruritic maculopapular rash –> becomes vesicular and crusts before healing
- Associated with pneumonia, hepatitis, encephalitis
What are the Ix for ?varicella zoster infection in pregnancy?
- Antenatal screening is not routine, but women are asked if they have had chickenpox at booking
-
Primary infection is usually a clinical diagnosis
- If diagnosis is in doubt or severe infection: PCR of skin lesions or CSF (confirms diagnosis)
-
VZV IgM/IgG serology
- To determine immunity status in women who have been exposed and have unknown immune status
-
Serial USS
- For all women who develop primary varicella in pregnancy, to screen for foetal consequences
What is the Mx for a woman who has been exposed to varicella zoster infection during pregnancy?
Maternal suspected varicella contact:
- Clarify significance of contact (significant if face-to-face or in same room for >15mins)
- Determine immune status
- Previous history of chickenpox –> assume immunity, no action needed
- Uncertain/no history of chickenpox –>VZV IgG serology
- If IgG is present –> immune, no action needed
- If not immune:
- Give varicella zoster immunoglobulin (VZIG) if <10d since exposure
- Advise the woman that she is potentially infectious from 8-28d after contact
- Discuss postpartum varicella vaccination
- Seek medical help if rash develops
What is the Mx for a woman who has confirmed varicella zoster infection during pregnancy?
Maternal chickenpox:
- Avoid contact with other pregnant women and neonates until lesions have crusted over
- Consider hospital admission if >20wks or signs of severe infection (pneumonia, neurological signs)
- Advise woman to attend hospital immediately if symptoms worsen
- Acyclovir:
- For patients presenting <24hrs since rash onset and >20wks gestation
- Consider if <20wks gestation
- IV if any signs of severe infection
- For patients presenting <24hrs since rash onset and >20wks gestation
- Refer to foetal medicine specialist –> serial USS; counselling
- Delivery:
- Avoid until 7d after rash onset (to allow antibody transfer to reduce risk of newborn infection)
- Give VZIG if delivery occurs within 5-7d, or if mother developed varicella within 5d after birth
- Infection at <28wks gestation:
- Inform woman of 1% risk of foetal varicella syndrome
- May consider amniocentesis to detect VZV DNA
What are the maternal complications of varicella zoster infection during pregnancy?
Maternal complications:
- Pneumonia (10%), hepatitis, encephalitis, meningitis
- Delivery during viraemic period has high risk of thrombocytopenia and DIC
What are the foetal complications of varicella zoster infection during pregnancy?
Foetal complications:
-
Varicella infection of the newborn:
- Highest risk if maternal infection occurs 5 days before or after delivery (can occur within 4wks) – when foetus is unprotected by maternal antibodies and viral load is high
- Transmission can be transplacental, vaginal or from direct contact after birth
- Infants born in high-risk period should receive VZIG, be closely monitored, and receive acyclovir if any symptoms develop
- Mortality 30%
-
Foetal varicella syndrome:
- Occurs in 1% pregnancies infected by VZV before 20wks gestation
- Caused by subsequent reactivation of VZV in utero as herpes zoster
- Presents with skin scarring in a dermatomal distribution, ophthalmic lesions, limb hypoplasia and neurological abnormalities (incl. microcephaly)
What is cytomegalovirus infection in pregnancy?
Primary or recurrent infection with CMV in pregnancy
What is the aetiology of cytomegalovirus infection in pregnancy?
- CMV is a member of the Herpesvirus family (HHV5) DNA virus
- Transmitted via respiratory droplet transmission/personal contact; can be transmitted vertically via placenta and via blood products
- CMV establishes latency (in lymphocytes) and can become reactivated (like other Herpes viruses)
- Reactivation occurs intermittently, with shedding in the genital, urinary or respiratory tract
- Primary infection is more likely to cause congenital CMV (40%) than reactivation (1%)
- Primary infection in 1st trimester gives highest risk
- High prevalence of seropositive women means reactivation accounts for 30-50% of congenital infection
What is the epidemiology of cytomegalovirus infection in pregnancy?
- Most common virus transmitted to foetus during pregnancy
- 60% women are seropositive for CMV before pregnancy; 1% become infected during pregnancy
What are the symptoms of cytomegalovirus infection in pregnancy?
- Primary maternal CMV infection is usually asymptomatic
- May cause flu-like illness (fever, malaise)
What are the Ix for ?cytomegalovirus in pregnancy?
- Pregnant women are not screened; there is no vaccine
-
Viral serology for CMV-specific IgM and IgG
- Positive if IgG in a previously negative mother, or IgM and low IgG avidity (<30%)
- Investigations in foetus/infant:
-
Amniocentesis/foetal blood sampling and PCR if foetal infection is suspected
- Must be done after 21wks because functioning kidneys are required for virus to be excreted into amniotic fluid; at least 6wks after maternal infection
-
Serial USS for features of congenital CMV
- Diagnosis is often suspected after abnormalities are seen on USS
- Microcephaly, IUGR, hepatosplenomegaly, ventriculomegaly, hydrops
-
Neonatal brain USS if congenital infection
- audiological/ophthalmic/developmental routine screening
-
Amniocentesis/foetal blood sampling and PCR if foetal infection is suspected
What is the Mx of cytomegalovirus infection in pregnancy?
Referral to foetal medicine specialist (if confirmed CMV during pregnancy)
Maternal infection:
- No treatment needed
- Avoid anti-CMV drugs (ganciclovir, foscarnet) –> teratogenic
If foetal infection is confirmed (by amniocentesis):
- Offer TOP
- Serial USS to look for congenital CMV
What is the main complication of cytomegalovirus infection in pregnancy?
Congenital cytomegalovirus:
- 40% primary CMV infections in pregnancy are transmitted to foetus
- In infected infants, 90% have no features of CMV, 5% have clinical features at birth, 5% develop features later in life
- Highest risk of congenital CMV is
- Complications:
- Miscarriage/stillbirth, IUGR
- Microcephaly, poor tone/abnormal head lag, sensorineural hearing loss, blindness (chorioretinitis), hepatosplenomegaly, thrombocytopenic purpura
- Babies born without symptoms may develop sequalae later (2yrs): hearing loss, developmental delay, visual impairment
- High mortality in symptomatic newborns (DIC, hepatic dysfunction, bacterial superinfection)
What is rubella infection in pregnancy?
Infection with rubella virus in pregnancy; aka German measles
What is the aetiology of rubella virus infection in pregnancy?
- Single-stranded RNA togavirus
- Transmitted by airborne droplets between close contacts; also vertical transmission
- Incubation period 14 days; patients are infectious from 7-30d after infection (from 1wk before to 2wks after rash)
- Gestation at infection determines risk of vertical transmission and development of congenital rubella syndrome
What are the symptoms of rubella infection in pregnancy?
- Maternal rubella:
- Often asymptomatic
- Non-specific symptoms: fever, malaise, headache, coryza, arthralgia, lymphadenopathy
- Maculopapular rash (more common in children)
What are the Ix for ?rubella infection in pregnancy?
-
Antenatal screening is no longer done in UK (from 2016)
- Used to screen for IgM and IgG –> if neither present woman encouraged to seek vaccination post-partum (didn’t help current pregnancy but protected future pregnancies)
-
If maternal infection is suspected:
-
IgM and IgG ELISA
- IgM suggests recent infection; low IgG avidity suggests recent infection/high suggests distant
-
IgM and IgG ELISA
-
If maternal infection is confirmed:
- Amniocentesis/CVS
- Serial USS
- Infant urine/blood –> rubella PCR/IgM
What is the Mx for rubella infection in pregnancy?
Referral to foetal medicine specialist
- For any pregnant woman with known exposure
Maternal infection:
- Symptomatic treatment (e.g. antipyretics, NSAIDs)
- Inform woman she is infective from 7d before symptoms to 4d after
Foetal:
- <12wks: consider TOP (high likelihood of defects)
- 12-20wks: amniocentesis to confirm foetal infection
- Consider TOP if infection is confirmed; serial USS if continuing with pregnancy
- >20wks: no action required
What are the maternal complications of rubella infection in pregnancy?
Maternal complications (uncommon):
- Thrombocytopenia
- Encephalitis
What is the main foetal complication of rubella infection in pregnancy?
Congenital rubella syndrome:
- Increased risk of miscarriage/stillbirth and IUGR
- Classified into ‘present at birth’ and ‘late onset’
-
Present at birth:
- Sensorineural deafness, congenital cardiac abnormalities, ophthalmic defects (cataracts), CNS abnormalities (microcephaly, developmental delay)
-
Late onset:
- DM, thyroiditis, GH abnormalities, behavioural disorders
What is Toxoplasmosis in pregnancy?
Infection with Toxoplasma gondii during (or immediately before) pregnancy
What is the aetiology of toxoplasmosis?
Toxoplasma gondii is a protozoan parasite found in cat faeces, soil or uncooked meat
Transmitted by ingestion of the parasite from undercooked meat or from unwashed hands; also vertical transmission
Parasitaemia occurs within 3wks of infection –> risk to foetus if infected occurs during/just before pregnancy
- Transplacental infection may occur during parasitaemia –> 40% foetuses infected
What is the epidemiology of toxoplasmosis?
1/3 people are infected by toxoplasmosis at some point in their life; congenital toxoplasmosis is rare
What are the symptoms of toxoplasmosis in pregnancy?
- Maternal infection:
- Usually asymptomatic (90%)
- May have non-specific symptoms: lymphadenopathy, fever, malaise, arthralgia
What are the Ix for ?toxoplasmosis in pregnancy ?
- Screening is not routinely done
-
If maternal infection is suspected:
-
IgM and IgG, IgG avidity ELISA
- IgG suggests previous exposure; IgM may suggest acute infection (serial testing must be done to show rising titres – high false-positive rate)
-
IgM and IgG, IgG avidity ELISA
-
Investigations for foetus/infant:
- Amniocentesis/CVS
-
Cord serum/newborn serum: IgM, IgA and IgE
- IgM suggests infection; IgA/E in cord serum are diagnostic of congenital toxoplasmosis
-
Serial USS
- Suspicious USS may be the first suggestion (is suspicious –> do amniocentesis/CVS)
What is the Mx for toxoplasmosis in pregnancy?
Prevention:
- Advise pregnant women to avoid raw/rare meat, avoid handling cats and litter, wear gloves and wash hands when gardening/handling soil
Maternal treatment:
-
Spiramycin (oral, 3wk course, 2-3g/d)
- Reduces the incidence of transplacental infection
- May also use pyrimethamine, sulfadiazine and calcium folinate
- Offer TOP if USS abnormalities
Newborns with congenital toxoplasmosis:
-
Pyrimethamine, sulfadiazine and calcium folinate for 1yr
- Limits CNS and eye damage
What is the main complication of toxoplasmosis in pregnancy?
Congenital toxoplasmosis:
- Highest risk is if infection in 1st trimester
- 10% infections are transmitted; 85% congenital disease if transmitted
- In 3rd trimester, 85% infections are transmitted but only 10% risk of congenital disease
- Increased risk of miscarriage and IUGR
- Often asymptomatic at birth, but 85% develop symptoms
- Symptoms: retinopathy, CNS problems (seizures, learning difficulty), intracerebral calcification
- If severe: microcephaly, ventriculomegaly
What is listeria infection in pregnancy?
Infection with Listeria monocytogenes in pregnancy –> leads to listeriosis
What is the aetiology of listeria infection in pregnancy?
Listeria monocytogenes is a gram-positive facultatively anaerobic bacillus, whose lifecycle involves obligate intracellular replication
- People with reduced cell-mediated immunity, and therefore pregnant women, are most at risk
Infection is by consuming contaminated food –> unpasteurised milk, ripened soft cheese, pate, prawns
- It is not transmitted in hot foods; can multiply at refrigerator temperatures (so transmitted in chilled food)
Vertical transmission can occur (transplacentally or through contaminated birth canal (ascending through cervix))
What are the symptoms of listeria infection in pregnancy?
- Maternal infection:
- 1/3 asymptomatic
- Flu-like illness with fever, general malaise, myalgia, headache, diarrhoea and vomiting
What are the investigations for ?listeria infection in pregnancy?
- Not routinely screened for
- Bloods: FBC (high WCC)
- Blood cultures
- Vaginal, perinatal and amniotic fluid swabs and culture
- For perinatal listeriosis
What is the Mx of listeria infection in pregnancy?
Prevention:
- Advise pregnant women to not eat soft cheese/unpasteurised milk/pate
Treatment of maternal infection:
- IV ampicillin
- Gentamycin added if very severe (but rarely used as teratogenic)
What are the complications of listeria infection in pregnancy?
Complications:
- Maternal meningitis, sepsis, endocarditis
-
Septic abortion/stillbirth (20%)
- Due to chorioamnionitis or transplacental transmission with generalised formation of microabscesses in the embryo (granulomatosis infantiseptica)
- Premature delivery (50%)
- Meconium staining
-
Clinical neonatal Listeria infection (in 75% neonates born to mothers with listeriosis)
- Respiratory distress, sepsis, neurological symptoms
What is the aetiology of parvovirus B virus in pregnancy?
Parvovirus B19 is a single-stranded DNA virus
- Infects erythrocyte progenitor cells –> usually causes a mild, self-limiting infection
- Foetus has decreased RBC survival time (more vulnerable) –> aplastic anaemia
Transmitted by respiratory droplets or blood; vertical transmission (transplacental)
- Transplacental transmission occurs in up to 30% infections; 2nd trimester has highest risk
What is the epidemiology of parvovirus B infection in pregnancy?
- Common (1 in 400 pregnancies); most common in women who work with young children (e.g. teachers)
- 50% women of childbearing age are immune, so 50% are susceptible to infection
What are the symptoms of parvovirus B infection in pregnancy?
- Maternal infection:
- Usually asymptomatic
- Arthralgia (usually proximal interphalangeal joints and knees), malaise
- NB in children: erythema infectiosum (slapped cheek syndrome)
What are the Ix for ?parvovirus B infection in pregnancy?
- Not routinely screened for
- IgM/IgG serology
- IgM may persist for 2-3 months after infection
- FBC and reticulocyte count (for anaemia)
- Foetal investigations:
- Amniocentesis for PCR
- Serial USS (for hydrops)
- Ascites, oedema, pleural effusion, polyhydramnios
- High velocity in MCA on Doppler USS suggests anaemia
What is the Mx of parvovirus B infection in pregnancy?
Referral to foetal medicine specialist for all suspected infection
Maternal:
- Symptomatic therapies (antipyretics, analgesia)
Foetal:
- Serial USS and Doppler assessment (for foetal hydrops)
- Intrauterine blood transfusion considered in hydrops (at tertiary centre)
- 10% risk of intrauterine death if <20wks gestation (can’t transfuse); 1% if >20wks
What are the complications of parvovirus B infection in pregnancy?
Foetal complications:
- Severe anaemia, hydrops fetalis and intrauterine death
- Aplastic anaemia results in high output cardiac failure and increased hepatic and extrahepatic erythropoiesis –> portal HTN and hypoproteinaemia –> ascites (hydrops)
- Hydrops fetalis: abnormal accumulation of fluid in 2 or more foetal compartments
- If foetus survives the anaemia –> full recovery
- 10% risk intrauterine death if foetus is infected
- Aplastic anaemia results in high output cardiac failure and increased hepatic and extrahepatic erythropoiesis –> portal HTN and hypoproteinaemia –> ascites (hydrops)
What is the aetiology of malaria infection in pregnancy?
Parasite transmitted by female Anopheles mosquito; most severe type is Plasmodium falciparum
Pregnant women have increased risk of malaria, and are more susceptible to severe disease
- Parasites can sequester in the placenta (so may have negative blood films)
- Co-infection with HIV is common in endemic areas –> vertical transmission of both malaria and HIV is more common if the two infections co-exist
What are the symptoms of malaria infection in pregnancy?
- Maternal infection:
- Cyclical spiking pyrexia (often every 48-72hrs)
- Headache, myalgia, anorexia, diarrhoea
- Anaemia; jaundice and renal failure (due to haemolysis)
- Hypoglycaemia
- Altered consciousness, seizures, hypotension (if severe)
What are the Ix for ?malaria infection in pregnancy?
- Thick and thin blood films
- Thick films to identify parasite; thin films to identify species
- Bloods: FBC (anaemia), clotting (may have bleeding complications), U&Es, LFTs, glucose
- Foetal monitoring (CTG, USS)
What is the Mx of malaria infection in pregnancy?
Prevention:
- In endemic areas: insecticide-treated bed nets, preventative treatment during pregnancy
- For travellers:
- Advise they should only go if absolutely necessary
- Insecticide sprays, mosquito nets, appropriate clothing
- Antimalarial drug prophylaxis: expert advice, balance risks of teratogenicity with risk of malaria; chloroquine and mefloquine considered safe for foetus)
Treatment:
- Manage with infectious diseases specialist and obstetrician
- Supportive care (ABCDE)
-
Antimalarials
- Choice is dictated by local sensitivity
- Quinine + clindamycin; IV artesunate if severe
What are the complications of malaria infection in pregnancy?
Maternal complications:
- Hypoglycaemia
- Severe anaemia
- Metabolic acidosis
- AKI
- Seizures
Foetal complications:
- Associated with miscarriage, preterm labour and IUGR
- Congenital malaria affects 1%
What is HIV infection in pregnancy?
Pre-existing HIV infection before pregnancy, or infection during pregnancy
What is the aetiology of HIV infection in pregnancy?
HIV is transmitted through sexual contact, blood and blood products or vertical transmission
- Vertical transmission can occur in utero, intrapartum or through breastfeeding

What are the symptoms of HIV infection in pregnancy?
- Asymptomatic initially
- Seroconversion: flu-like illness 1-3wks after infection
- General decline in immune function –> infections (AIDS)
- Time between HIV infection and AIDS varies from a few months to 17yrs in untreated patients
What are the Ix for ?HIV infection in pregnancy?
-
Routine antenatal screening at booking (for all pregnant women) – antigen/antibody ELISA
- Repeat testing if woman remains at risk of HIV/possible exposure
- Testing at 6 weeks, 3 months and 6 months after possible exposure
- Rapid HIV tests if woman presents for labour unbooked
- Repeat testing if woman remains at risk of HIV/possible exposure
- Regular CD4 and viral load tests for HIV-positive women
- Neonatal HIV testing (see management)
What is the Mx of HIV infection in pregnancy?
MDT approach –> infectious diseases, obstetricians etc.
Maternal management:
-
Antenatal antiretroviral therapy:
- Given antenatally to all HIV +ve women (regardless of viral load)
- Women already receiving ART should continue their therapy
- Started ASAP; continued intrapartum; discontinued after delivery (if not needed for mother’s HIV)
- Given antenatally to all HIV +ve women (regardless of viral load)
-
Delivery:
- If viral load >1000copies/mL at 38wks or in labour:
- C-section (elective or emergency if woman presents in labour)
- Start IV zidovudine 3hrs before surgery (and continue antepartum ART)
- If viral load <1000copies/mL at 38wks or in labour, or HCV co-infection:
- Vaginal delivery (as low risk of transmission)
- Avoid obstetric interventions if possible (e.g. foetal blood sampling, instrumental)
- IV zidovudine considered if viral load 50-999copies/mL
- Continue antepartum ART
- Vaginal delivery (as low risk of transmission)
- If viral load >1000copies/mL at 38wks or in labour:
- Avoid breastfeeding
- May still be encouraged in developing countries
Management of infants:
- Clamp cord ASAP and bathe baby immediately after birth
- Treat all infants with ART from birth
- Usually zidovudine orally for 4-6 weeks
- HAART if mother started antiretrovirals late in pregnancy
- PCR to detect infant infection
- At birth, 3 weeks, 6 weeks and 6 months
- HIV can be excluded in infants who have not been breastfed and have 2 or more negative tests (1 must be at >4 months)
- Antibodies aren’t tested because maternal antibodies cross placenta –> always positive
- At birth, 3 weeks, 6 weeks and 6 months
What are the complications of HIV infection in pregnancy?
Complications:
- Vertical transmission
- <2% with appropriate treatment; up to 45% without treatment
- Possible increased risk of stillbirth, prematurity
- Data about teratogenic effects of ART is incomplete; generally considered safe (and benefits outweigh risks)
What is hep B infection in pregnancy?
HBV chronic infection in pregnancy
What is the aetiology of Hep B infection in pregnancy?
HBV is a DNA virus that infects hepatocytes
Transmitted mainly in blood; also by other body fluids (saliva, semen); vertical transmission can occur at delivery
Infection resolves in 90% adults; chronic infection occurs in 10%
- Women with HBsAg or HBeAg are infectious (acute or chronic); anti-HBsAb suggests past infection but now immune (and do not infect others)
What are the symptoms of Hep B infection in pregnancy?
- Usually asymptomatic
- Jaundice, fever, hepatomegaly, RUQ tenderness
- Myalgia, nausea, vomiting, fatigue
What are the Ix for ?Hep B infection in pregnancy?
- Routine antenatal screening offered to all pregnant women
- HBsAg/HBeAg: indicates acute or chronic infection
- Anti-HBsAb: indicates resolved infection (or vaccination) and immunity
- Anti-HBc IgM: indicates acute infection (not chronic)
- LFTs, clotting profile
What is the Mx of Hep B infection in pregnancy?
Refer to hepatologist ongoing monitoring for long-term consequences of chronic infection
Maternal antiviral therapy:
- Tenofovir
- Considered if viral load is >200,000IU/mL
Neonatal immunoprophylaxis:
- Hepatitis B vaccine
- Given immediately after delivery
- Gives immediate protection from any virus transmitted via contact with blood during delivery
- Hepatitis B immunoglobulin
- Given at birth, 1 month and 6 months
- Gives ongoing protection from subsequent exposure
What are the complications of Hep B infection in pregnancy?
Complications:
- Chronic infection –> cirrhosis, hepatic failure, hepatocellular carcinoma
- Vertical transmission during delivery
- 90% infected infants without post-exposure prophylaxis develop chronic HBV
- Vertical transmission is 95% preventable with appropriate management
What is the aetiology of Hep B infection in pregnancy?
RNA virus belonging to Flavivirus family, which infects hepatocytes
After primary infection, 80% people progress to chronic infection (less likely if young and healthy)
Transmission is mainly via blood (esp IVDU); sexual transmission is rare; vertical transmission can occur by direct contact with infected maternal blood around the time of delivery
- Risk of vertical transmission is higher in those co-infected with HIV
What are the symptoms of Hep B infection in pregnancy?
- Primary infection:
- Usually asymptomatic –> most do not know they are infected
- Jaundice, fever, hepatomegaly, RUQ tenderness
- Myalgia, nausea, vomiting, fatigue
- Chronic infection:
- Liver failure, hepatic encephalopathy etc
What are the Ix for Hep B infection in pregnancy?
-
Regular antenatal screening is not offered (due to lack of evidence for effective treatment in pregnancy)
- Offered to high-risk groups, e.g. HIV positive
- HCV antibodies in serum (IgM/IgG), confirmed by PCR
- LFTs, clotting studies
What is the Mx of Hep B infection in pregnancy?
Antivirals are used in non-pregnant adults (may cause teratogenic effects – use with caution)
Delivery:
- No strong evidence for mode (C-section hasn’t been proven to reduce transmission) –> can have vaginal
- C-section recommended if co-infection with HIV
What are the complications of Hep B infection in pregnancy?
Complications:
- Chronic infection –> liver failure, HCC
- Vertical transmission (5% risk)
- Risk increases with increasing maternal viral load
- Infected neonates are prone to chronic hepatitis
What is TB infection in pregnancy?
Active infection with TB during pregnancy
What is the aetiology of TB infection in pregnancy?
- Caused by Mycobacterium tuberculosis
- Transmitted via droplets; vertical transmission is very rare but can occur
- RFs for TB infection include travel to endemic areas, exposure to infection, immunosuppression
- Pregnancy may increase risk
What are the symptoms of TB infection in pregnancy?
- Cough, fever, anorexia, night sweats, malaise
What are the Ix for ?TB infection in pregnancy?
- Consider Ix if symptoms suggesting active TB, recent exposure to TB or HIV positive
-
Sputum sample
- MC&S (acid-fast bacilli on microscopy)
- CXR (opacities in upper lobes)
-
Tuberculin skin test (Mantoux test)
- Inject purified protein derivative of M. tuberculosis –> red/swollen injection site after 1-2 days if previously encountered TB (active or latent infection or vaccine)
- Negative result does not completely rule out TB (false negatives)
- Interferon gamma blood tests have recently been developed to detect previous exposure –> may be more specific
- Inject purified protein derivative of M. tuberculosis –> red/swollen injection site after 1-2 days if previously encountered TB (active or latent infection or vaccine)
What is the Mx of TB infection in pregnancy?
Specialist referral for women with TB in pregnancy
Prophylaxis:
- Do not give BCG during pregnancy (live vaccine)
- If in an at-risk group, vaccinate post-partum
Latent infection:
- Treat if there is high risk of progression to active TB (e.g. recent TB infection, HIV infected) –> isoniazid + pyridoxine
- Otherwise, don’t treat
Active infection:
- Management is the same as non-pregnant women –> rifampicin (6 months), isoniazid (6 months), pyrazinamide (2 months), ethambutol (2 months)
What are the complications of TB infection in pregnancy?
- Pregnancy has little impact on TB
- Late diagnosis and treatment can lead to prematurity and IUGR
- Vertical transmission
- Risk is very low
- Good outcomes with early treatment of neonate
- Infection of newborn (droplet transmission if mother has untreated disease)
- 2 weeks of treatment usually means patients are non-infectious
- If mother has had <2wks of treatment before delivery:
- Treat baby prophylactically with isoniazid and pyridoxine for 3 months
- Tuberculin test after 3 months (if +ve, assess for TB and treat; if -ve, give BCG and stop Rx)
What is group B streptococcal infection in pregnancy?
Infection with GBS (aka Streptococcus agalactiae)
What is the aetiology of group B streptococcal infection in pregnancy?
Streptococci are gram-positive cocci which grow in chains GBS is a subtype of beta-haemolytic Strep
GBS is a commensal bacterium found in the vagina or rectum of 20% pregnant women
- Usually causes no symptoms but can cause neonatal infection
- Early-onset neonatal infection is due to infection of the amniotic fluid before birth
- Transmission can occur from the time the membranes are ruptured until delivery
- Late-onset infection may occur due to colonisation after birth
- Early-onset neonatal infection is due to infection of the amniotic fluid before birth
RFs for colonisation with GBS are unknown
RFs for neonatal infection:
- Previous baby with GBS infection, maternal colonisation with GBS, GBS bacteriuria in pregnancy
- Maternal pyrexia during labour
- PROM (due to ascending infection)
- Preterm labour
What is the epidemiology of group B streptococcal infection in pregnancy?
20% pregnant women are colonised; neonatal infection is rare (0.05%)
Most common cause of early-onset sepsis
What are the symptoms of group B streptococcal infection in pregnancy?
- Maternal colonisation is asymptomatic
- May cause maternal infection
- UTI: frequency, urgency, dysuria
- Chorioamnionitis (intrapartum): fever, uterine tenderness, purulent amniotic fluid, foetal distress
- Endometritis (postpartum): fever, uterine tenderness, intermenstrual bleeding, foul discharge
What are the Ix for group B streptococcal infection in pregnancy?
-
Vaginal/rectal swabs to detect GBS
- Antenatal screening is not routine
- Routine screening does not accurately predict which women will be positive at delivery
- Many infected babies are preterm, so born before screening is done anyway
- Screening offered to high-risk groups
- E.g. previous GBS-infected baby, GBS bacteriuria in pregnancy
- May be offered if woman has been GBS +ve in previous pregnancy but unaffected neonate
- Swabs at 35-37wks
- Antenatal screening is not routine
What is the Mx of group B streptococcal infection in pregnancy?
Antenatal treatment of GBS is not recommended
- Does not reduce the chance of colonisation at delivery (women often become re-infected)
Intrapartum management:
-
Intrapartum antibiotic prophylaxis
- IV benzylpenicillin (clindamycin if allergic)
- Indicated if: previous infant with GBS disease, GBS bacteriuria during pregnancy, swabs +ve at 35-37wks, maternal pyrexia in labour, rupture of membranes >18hrs, preterm labour
- NB not indicated in planned C-sections (as no ruptured membranes no foetal exposure)
- Augment immediately if PROM in GBS +ve woman (reduce exposure of foetus)
What are the complications and prognosis of Group B streptoccocus infection in pregnancy?
Complications:
- UTI, chorioamnionitis, endometritis
-
Early-onset neonatal infection –> sepsis, meningitis, pneumonia (see paeds)
- Conflicting evidence about whether to treat if no signs of infection but RFs for infection (refer to hospital guidelines)
- Late-onset neonatal infection –> usually meningitis; also osteomyelitis, septic arthritis (see paeds)
Antibiotics in labour are 60-80% effective in reducing early-onset neonatal GBS infection
What is red degeneration of fibroids?
- Uterine fibroids (leiomyomas) are common, benign tumours of smooth muscle in the uterus affecting 20% of women of reproductive age.
- ‘Red’ degeneration describes the breakdown of myocytes secondary to ischaemia and is the most common form of fibroid degeneration
What is the aetiology of red degeneration of fibroids?
- ‘Red’ degeneration describes the breakdown of myocytes secondary to ischaemia and is the most common form of fibroid degeneration.
- It most commonly presents in pregnancy, when fibroids tend to outgrow their blood supply owing to increased circulating oestrogen
What is the pathophysiology of red degneration of fibroids?
- The pathophysiology of fibroids is not entirely clear. However, it is clear that they are oestrogen dependent, and receptors for this hormone bind 20% more oestradiol (E2) than in adjacent myometrium tissue.
- 15% of pregnant women who have fibroids experience red degeneration during pregnancy, a period of physiological hyper-oestrogenism.
- Experimental studies suggest that the growth of fibroid tissue under oestrogen influence is related to excessive production of extracellular matrix and hyaline tissue, which interposes between myocyte cells and the capillary beds causing ischaemia (necrobiosis).
- This then leads to aseptic lysosomal digestion of ischaemic myocytes between areas of hyalinised tissue (cystic degeneration).
What are the symptoms of red degeneration of fibroids?
- Typical presentation is in the second trimester of pregnancy
- most commonly in 12th – 22nd week
- acute abdo pain AND low-grade fever
What are the signs of red degeneration of fibroids?
Obs:
- ~ tachycardia and tachypnoea, secondary to pain
- low-grade fever common
- NO haemodynamic compromise / increased oxygen requirement in simple acute fibroid degeneration
Abdo exam:
- Constant abdominal pain localising to the area of the fibroid
- Area tender to palpation
- Rebound tenderness present
- Fibroid likely palpable as it enlarges
- Firm and fixed on palpation
What are the Ix for ?red degeneration of fibroids?
Bloods
- FBC
- May show raised WCC
- Highly elevated WCC and CRP with clinical signs of infection suggests sepsis secondary to infection of degenerating fibroid
Imaging
-
USS
- Colour-flow doppler can help differentiate fibroids from myometrial thickening
-
Serial USS
- useful to track developing size and relation to the fetus of fibroid
-
MRI
- Considered if symptoms continue or exacerbate despite conservative management, and to rule out other diagnoses such as torsion of a pedunculated fibroid if ultrasound is inconclusive
- MRI can map fibroid location and relation to the fetus if surgery is being considered
Other
-
CTG
- Close monitoring of the fetus for complications
- Fetal distress is an indication for emergency caesarean section
What is the Mx for red degeneration of fibroids?
Conservative management
- The mainstay of treatment is conservative management.
- The decision will then be made whether to manage in ambulatory care with regular check-ups or to admit the patient for observation.
-
Patients should be reassured that fibroids usually regress during the puerperium owing to hormonal withdrawal.
-
Analgesia (paracetemol)
- Some may require hospitalisation and monitoring, with opiate analgesia for severe pain
- Acute painful episode usually resolves in 4-7 days
- NSAIDS should be used with caution to avoid fetal complications such as premature closure of the ductus arteriosus
Surgical management
- In very rare cases, the decision may be made to remove fibroids in the first or second trimester of pregnancy.
-
Myomectomy
- Fibroids causing intractable pain or a torted pedunculated fibroid are rare indications for myomectomy, and the risk of intra-operative bleeding is very high
- Combined caesarean section with myomectomy following delivery of the baby is also not recommended
What is HELLP syndrome?
- 3 features of the condition:
- Hemolysis
- Elevated Liver enzyme levels
- Low Platelet levels
- It is a serious condition that can develop in the late stages of pregnancy.
- Whilst there is significant overlap with severe pre-eclampsia in terms of the features some patients present with no prior history so many specialists consider it a separate entity in its own right.
What % of those with seevere pre-eclampsia go on to develop HELLP syndrome?
~ 10-20% of patients with severe preeclampsia will go on to develop HELLP
What are the risk factors for HELLP syndrome?
- Previous pregnancy with HELLP syndrome
- Pre-eclampsia or pregnancy induced HTn
- 25yrs <
- Caucasian
- Multiparous (given birth 2 or more times)
What are the symptoms of HELLP syndrome?
- RUQ abdo pain
- nausea & vomiting
- headache
- blurry vision
- fluid retention and excess weight gain
- lethargy/fatigue
- rarely, nosebleed or seizures
What are the signs of HELLP syndrome?
- tender RUQ abdomen
- ~ oedema
- brisk reflexes (sign of pre-eclampsia)
- HTN
What are the Ix for ?HELLP syndrome?
-
Bloods:
-
FBC
- reduced haemoglobin, low or normal haematocrit, thrombocytopenia
-
peripheral blood smear
- diagnostic: schistocytes, burr cells, polychromasia may be seen ( = haemolysis)
-
LFTs
- high ALT or AST (= haemolysis)
-
bilirubin level
- high total and indirect billirubin ( = haemolytic anaemia)
-
serum LDH
- high ( = haemoloysis / liver dysfunction).
-
uric acid
- ~ high (= renal compromise)
-
prothrombin time
- ~ high (+ thrombocytopenia = DIC)
- fibrinogen level
- ~ low (+ thrombocytopenia = DIC)
-
FBC
-
Urine:
-
urinalysis
- proteinuria (= increased tubular permeability)
-
protein-to-creatinine ratio
- protein-to-creatinine ratio of >0.30
-
urinalysis
-
Foetal USS
- evaluate fetal presentation, gestational age, and biophysical status, and to identify any growth restriction (if fetal growth restriction, progress to Doppler studies of umbilical cord and fetus).
- ~ fetal growth restriction
What is the Mx of suspected HELLP syndorme?
-
seizure prophylaxis
- IV magnesium sulfate: 4-6 g as a loading dose, then 1-2 g/hour infusion for at least 24 hours
-
IV corticosteroids
- IV dexamethosone: should be administered for 24 to 48 hours, ideally before delivery is undertaken, in pregnancies <34 weeks’ gestation in order to enhance fetal lung maturation and diminish risk of intraventricular bleeding and necrotising enterocolitis
if BP > ≥160/105:
-
Antihypertensives
- IV labetalol: 20 mg initially, followed by 40-80 mg every 10 minutes according to response, maximum 300 mg total dose
What is the Mx of confirmed HELLP syndorme?
- induction of labour / C section
- IV dexamethasone
- IV magnesium sulfate
- seizure prophylaxis
IF
-
BP ≥160/105
- continued antihypertensive therapy: IV labetelol
-
platelet count <25 × 10⁹/L (<25,000/microlitre) (or <30 × 10⁹/L [<30,000/microlitre] if bleeding, massive transfusions, or surgery)
- platelet transfusion ± anti-D immunoglobulin
-
fibrinogen <2.94 micromol/L (<100 mg/dL)
- fresh frozen plasma or cryoprecipitate
-
haematocrit <25%
- blood transfusion
What is PROM?
Premature rupture of membranes (PROM): spontaneous rupture of membranes >1hr prior to the onset of labour, at >37wks gestation
Pre-term premature rupture of membranes (PPROM): spontaneous rupture of membranes >1hr prior to the onset of labour, at <37wks gestation
What is the aetiology of PROM?
Physiological mechanisms (e.g. enzymatic collagen breakdown, Braxton Hicks contractions) lead to weakening of membranes
-
In PPROM, there is early weakening and rupture of membranes
- Strongly associated with infection (often subclinical)
- Other RFs: previous PPROM/preterm labour, antepartum bleeding, UTI/genital infections, invasive procedures (amniocentesis), polyhydramnios, multiple pregnancy, cervical incompetence, smoking
What is the epidemiology of PROM?
- PROM is common –> 10% term pregncies
- PPROM occurs in 2% of pregnancies (40% of preterm deliveries)
What are the symptoms of PROM?
- ‘Broken waters’ –> painless popping sensation, followed by gush of fluid vaginally, then constant trickle
- Can be less dramatic, e.g. gradual leakage, change in consistency of discharge
What are the signs of PROM?
On examination:
- Avoid bimanual until woman is in active labour (risk of infection)
- Speculum: fluid draining from cervix and pooling in posterior fornix, lack of normal discharge
What are the Ix for ?PROM?
- Usually clinical diagnosis
- Basic obs
- Bloods: FBC, CRP (infection)
- Micro: MSU, vaginal swabs (infection)
- CTG
- USS
- May show oligohydramnios
- Confirm presentation
- Other tests (not routine):
- Ferning test: fluid placed onto glass slide and dried fern-patterned crystals form if PROM/PPROM
- Swabs of fluid for IGFBP-1 or PAMG-1 (high concs in amniotic fluid)
What is the Mx of PROM?
PROM:
-
Clear liquor and no known GBS:
- Expectant management for 24hrs –> 60% women go into labour
-
IOL after 24hrs (but can wait up to 72hrs with 4hrly temperature and 24hrly foetal monitoring
- Prostaglandin or oxytocin infusion
- Monitor for signs of chorioamnionitis (temperature, CTG etc.)
- Prophylactic antibiotics considered
-
Meconium, known GBS or maternal pyrexia:
- Augment labour immediately
- Antibiotics (benzylpenicillin or clindamycin)
- Neonatal observation for at least 12hrs
What is the Mx of PPROM?
PPROM:
- Admit (may be subsequently managed as outpatient)
- Monitoring –> 4hrly temperature, regular CTG
- Advise patient to avoid sexual intercourse
- Give corticosteroids
- Antibiotics (erythromycin for 10d, benzylpenicillin during labour if GBS isolated)
- Most women go into labour within 24hrs –>little can be done to stop this
- Tocolysis is contraindicated (risk of infection)
-
If labour doesn’t start, management is determined by gestation:
-
<34wks: aim for increased gestation, deliver if signs of complications/foetal compromise
- If very premature, discuss viability
- 34-36wks: IOL
-
<34wks: aim for increased gestation, deliver if signs of complications/foetal compromise
What are the complications of PROM?
Complications:
- Chorioamnionitis (inflammation of foetal membranes/amniotic fluid due to infection)
- Preterm labour
- Oligohydramnios (and its complications)
- Placental abruption
- Cord prolapse
- Neonatal death (due to prematurity, sepsis and pulmonary hypoplasia)
Most women go into labour soon after rupture
- Grater latency period in younger gestational age –> 50% with PPROM deliver within 1 week
What is the prognosis of PROM?
Prognosis correlated with gestational age
What is preterm labour?
Onset of labour before 37wks gestation
- Preterm: 34-37wks; very preterm: 28-33+6wks; extremely preterm: <28ks
Can be categorised into spontaneous preterm labour, PPROM and iatrogenic
What is the aetiology of pre-term labour?
Causes of preterm labour:
- Iatrogenic (e.g. pre-eclampsia, IUGR)
-
Cervical weakness (e.g. due to previous cervical surgery)
- Relationship between cervical length and risk of preterm labour –> <2cm increases risk
- Suggested by Hx of painless 2nd trimester pregnancy loss
-
Infection
- Usually chorioamnionitis (which ascended from vagina)
- Cervical weakness and PPROM predispose
- Bacterial vaginosis is also associated with PTL
- Multiple pregnancy (due to uterine distension and iatrogenic causes)
- Polyhydramnios (due to uterine distension)
- Uterine Mullerian anomalies (congenital abnormalities of the uterus, vary in severity)
- Antepartum haemorrhage and placental abruption (due to thrombin stimulating uterine contractions)
- Smoking, cocaine, alcohol
What are the risk factors for pre-term labour?
- previous PTL
- PPROM
- cervical surgery
- short cervical length
- maternal infection
- multiple pregnancy
- polyhydramnios
- antepartum haemorrhage
- foetal abnormalities
- smoking/cocaine/alcohol
- environmental stress
What are the signs and symptoms of pre-term labour?
- Labour/ruptured membranes
What are the Ix for pre-term labour?
-
As for normal labour:
-
Basic obs:
- Hourly pulse, 4hrly BP
- Frequency of contractions every 30mins
- VE every 4hrs
- Urine dip (ketones and protein)
- When 2nd stage is reached: hourly BP, pulse and VE
-
Foetal assessment in labour:
- With each contraction, placental blood flow and O2 to foetus are interrupted
- Foetus may become compromised (esp if low reserve before labour)
- Insufficient O2 –> anaerobic metabolism –> metabolic acidosis –> neurological injury, death
- Hypoxia and acidosis cause change in foetal HR pattern (detected by auscultation and CTG)
- Meconium is passed by healthy foetus at term, or in response to foetal distress
- With each contraction, placental blood flow and O2 to foetus are interrupted
-
Methods:
- Inspection of amniotic fluid
- Foetal compromise is suggested by meconium (esp bright green), absence of fluid, heavily blood-stained fluid
- Intermittent auscultation of foetal heart
- Using Pinard stethoscope or hand-held Doppler USS
- Listen for 1min after a contraction; repeat every 15mins in 1st stage and 5 mins in 2nd stage
- Continuous CTG (see procedures)
- Foetal scalp electrodes can be used to directly detect foetal HR (used if poor foetal position or maternal obesity making CTG quality poor)
- Foetal blood sampling (see procedures)
- Inspection of amniotic fluid
-
Basic obs:
-
TVUSS of cervix (for cervical length)
- If cervix is closed
- Estimates likelihood of delivery –> risk if <2cm
-
Cervico-vaginal swab for fibronectin
- For women with contractions but not in advanced labour (<3cm dilated)
- Estimates likelihood of delivery
- Negative: 1% chance of delivery within 1 week –> can usually discharge
- Positive: risk of delivery
What is the Mx for pre-term labour?
Management of labour is the same as term (with continuous monitoring, neonatologists present, NICU bed etc.)
Management if high risk of imminent delivery:
- Discuss viability
- Continuous monitoring (CTG)
- Tocolytics
- Nifedipine (CCB) or atosiban (oxytocin receptor antagonist)
- May delay labour for 2-7d –> provide time for corticosteroids and transfer to neonatal unit
- Corticosteroids (if <34wks)
- Biggest influence on neonatal outcome –> stimulate foetal lung maturation
- Transfer to neonatal unit
- Antibiotics for GBS prophylaxis (benzylpenicillin)
Prevention of preterm labour:
- Serial cervical length surveillance to monitor women at high-risk
- Cervical cerclage
- Suture to hold cervix closed
- Indications: multiple previous midtrimester losses/preterm labour (history indicated), cervix <2.5cm in woman with previous preterm labour (USS indicated), and if cervix is dilated in absence of contractions (rescue cerclage)
What are the complications of pre-term labour?
Complications:
- Neonatal death (50% survival at 24wks; 80% survival at 26wks)
- Respiratory distress syndrome
- Intracranial haemorrhage
- Necrotising enterocolitis
- Sepsis
- Retinopathy of prematurity
- Developmental delay, cerebral palsy
What is normal labour?
Labour: presence of strong, regular, painful contractions resulting in progressive cervical dilatation and effacement
- In practice, labour is suspected when women presents with contraction-like pains and is confirmed when midwife performs a vaginal examination that revels effacement and dilatation of the cervix
Loss of a ‘show’ (blood-stained mucus plug passed from cervix) or SROM may occur around the same time
Women are advised to contact labour suite/midwife if membranes rupture or contractions occur < every 5mins
What is seen and should be observed O/E in normal labour?
Examination:
- General exam & basic obs
-
Abdo exam:
- Lie of foetus, presentation, engagement
- Assess contractions (palpate uterus)
-
Bimanual:
- Assess cervix for length, effacement, consistency, dilatation
- Should be fully effaced by 4cm dilatation
- If cervix is >4cm dilated, can determine position and station of presenting part
- If no cervix is felt –> fully dilated (10cm)
- Assess foetal head position, station, attitude and presence of caput or moulding
- Normally, the vertex is presenting –> can feel posterior fontanelle (triangular, 3 suture lines)
- Failure to feel posterior fontanelle may be because head is deflexed (abnormal attitude), the occiput is posterior (malposition) or there is so much moulding that sutures can’t be felt –> all 3 indicate prolonged labour or obstruction
- Relate the leading part of the head to the ischial spines (station)
- Note the condition of the membranes
- If ruptured –> colour and amount of amniotic fluid draining
- Assess cervix for length, effacement, consistency, dilatation
What are the Ix performed in normal labour?
Basic obs:
- Hourly pulse, 4hrly BP
- Frequency of contractions every 30mins
- VE every 4hrs
- Urine dip (ketones and protein)
- When 2nd stage is reached: hourly BP, pulse and VE
Foetal assessment in labour:
- With each contraction, placental blood flow and O2 to foetus are interrupted
- Foetus may become compromised (esp if low reserve before labour)
- Insufficient O2 –> anaerobic metabolism –> metabolic acidosis –> neurological injury, death
- Hypoxia and acidosis cause change in foetal HR pattern (detected by auscultation and CTG)
- Meconium is passed by healthy foetus at term, or in response to foetal distress
- Methods:
- Inspection of amniotic fluid
- Foetal compromise is suggested by meconium (esp bright green), absence of fluid, heavily blood-stained fluid
- Intermittent auscultation of foetal heart
- Using Pinard stethoscope or hand-held Doppler USS
- Listen for 1min after a contraction; repeat every 15mins in 1st stage and 5 mins in 2nd stage
- Continuous CTG (see procedures)
- Foetal scalp electrodes can be used to directly detect foetal HR (used if poor foetal position or maternal obesity making CTG quality poor)
- Foetal blood sampling (see procedures)
- Inspection of amniotic fluid
Partogram:
- Allows instant visual assessment of the progress of labour based on the rate of cervical dilatation compared to an expected norm, according to the parity of the women –> allows slow progress to be identified early
- Other key obs are recorded –> frequency and strength of contractions, descent of head in 5ths palpable and station, amount of amniotic fluid draining, foetal HR, maternal obs (BP, HR, T)
- Line is drawn on partogram at the end of the latent phase to demonstrate progress of 1cm/hr (alert line)
- Another line (action line) is drawn parallel and 4hrs to the right of it
- If the plot of the actual cervical dilatation reaches the action line slow progress
- Slow progress also considered if cervix dilates <1cm in 2hrs
What is the Mx of the 1st stage of normal labour?
1st stage:
- Latent stage:
- Mobilise, stay at home where possible, simple analgesia
- Can eat and drink (light food)
- VE every 4hrs (if in birth centre/labour ward)
- Active stage:
- In birth centre/labour ward
- One-to-one midwife care
- 4hrly BP, pulse and VE; auscultate foetal HR every 15 mins
- Partogram
- Membranes may still be intact –> not necessary to rupture if progress is satisfactory
What is the Mx of the 2nd stage of normal labour?
2nd stage:
- Support and reassurance
- Hourly BP, pulse and VE; foetal HR auscultated every 5mins
- Women guided by their urge to push
- Midwife can encourage pushing if involuntary maternal pushing does not occur
- Progress of descent of head is judged by watching perineum
- At first there is a bulge when women bear down, then head is seen at the height of contractions
- Between contractions, head disappears
- When head no longer disappears (crowning) it has passed through the pelvic floor and delivery is imminent
- When crowning occurs, midwife’s hands flex foetal head and guard perineum (control speed)
- Discourage woman from bearing down by ‘panting’
- Episiotomy can be used to accelerate delivery once head has passed through pelvic floor
- Once head is born, there is restitution and external rotation with next contraction –> shoulders can be delivered
- To aid shoulder delivery –> gentle traction on the head downwards and forwards until the anterior shoulder appears beneath the pubis
- Head then lifted gradually until posterior shoulder appears over the perineum –> baby swept upwards to deliver body and legs
- At first there is a bulge when women bear down, then head is seen at the height of contractions
What is done to provide immediate care of the neonate at the end of the 2nd stage of normal labour?
Immediate care of the neonate:
- Immediate skin-skin contact with mother (helps bonding, oxytocin release – uterine contractions)
- Dry baby and cover with warm blanket
-
Baby usually takes 1st breath within seconds
- Allow mucous in resp tract to drain; suction only if necessary
- Clamp and cut cord
- Apgar score should be calculated at 1 min and 5 mins after birth
- Initiation of breastfeeding within 1st hour
- Measurements of head circumference, birthweight and temperature; general exam for abnormalities
- Vitamin K given
What is an APGAR score?
Apgar scores:
- Used to assess wellbeing of the baby
- 1min assesses need for resuscitation (or should already have been assessed), 5mins assesses result of resuscitation and prognostic info, 10 and 15mins give prognostic info
- <7 is abnormal

What is the Mx of the 3rd stage of labour?
3rd stage:
- Normally 5-10 mins; 30 mins is prolonged (if active management)
- Signs of placental separation: lengthening of cord, small gush of blood, rising of uterine fundus to above umbilicus, uterine contraction
- Management is either active or physiological:
- Active management:
- Recommended for all women (reduces risk of PPH)
- IM 10IU oxytocin –> given as anterior shoulder of baby is delivered, or immediately after delivery
- Early clamping and cutting of cord
- When the signs of placental separation are recognised, controlled cord traction is used to speed up delivery of placenta
- When contraction is felt, L hand moved suprapubically to elevate fundus, and R hand exerts firm traction on cord so placenta separates and is delivered gently
- Twisting motion to peel off membranes
- Uterine inversion is a rare complication –> when fundus is not adequately controlled and excessive traction is exerted in absence of complete separation and a uterine contraction
- In 2% the placenta is not expelled –> try again after 10 mins
- If this fails, placenta is retained –> removal under GA/regional anaesthetic in theatre
- Physiological management:
- Placenta delivered by maternal effort; no uterotonics used
- Associated with heavier bleeding
- Active management recommended if heavy bleeding (>500ml) or if >60mins pass
- Active management:
- After delivery of placenta, it should be inspected for missing cotyledons or a succenturiate lobe
- If suspected –> examination under anaesthesia and manual removal of placental tissue
- Inspect vulva for tears
- May need repairing
Which types of pain relief may be administered in labour?
Essentially up to the woman; some medical indications/contraindications
Non-pharmacological methods:
- One-to-one midwife care and supportive birth partner reduce need for analgesia
- Relaxation and breathing exercises
- TENS (transcutaneous electrical nerve stimulation) – not that effective, may be used in latent phase
Opioid analgesia:
- E.g. pethidine, diamorphine
- Can be given by midwives without involvement of medical staff
- Limited pain relief during labour and have significant SEs
- Nausea and vomiting (always give with antiemetic), drowsiness/sedation, delayed gastric emptying (increasing the risks of GA), short-term resp depression for baby (reversed with naloxone), possible interference with breastfeeding
- Usually IM injection; can be SC or IV infusion by a patient-controlled analgesic device
- Very short acting opiates can have doses timed with contractions
- Popular among women who can’t have epidural but find non-pharmacological options insufficient
Inhalational analgesia:
- Nitrous oxide is usually available in the form of Entonox (equal mix of NO and O2)
- Quick onset, short duration of effect, more effective than pethidine
- May cause light-headedness, nausea and hyperventilation (as women attempt to achieve maximum effect)
- Not suitable for prolonged use from early labour because hyperventilation may cause hypocapnoea, dizziness, tetany and foetal hypoxia; most suitable later in labour
Epidural analgesia:
- Most reliable way of providing effective analgesia in labour
- Decision to have an epidural is made between the woman, midwife, obstetric team and anaesthetist
What are the indications for pain relief in labour?
- Pain relief (main indication)
- Prolonged labour/oxytocin augmentation
- Maternal hypertensive disorders, some maternal medical conditions (e.g. cardiac disease)
- High risk of operative intervention
- Multiple pregnancy
What are the contraindications for pain relief in labour?
- Coagulation disorders (e.g. low platelet count)
- Local or systemic sepsis
- Hypovolaemia
- Logistical (insufficient numbers of trained anaesthetic/midwifery staff)
What are the side effects and complications of pain relief in labour?
- Loss of sensation and movement in legs; itching (must warn woman)
- IV access and more intensive maternal and foetal monitoring needed (continuous CTG)
- Second stage of labour is longer and greater chance of instrumental delivery; reduced maternal urge to push
- May assist vaginal delivery sometimes by relaxing the woman and allowing time for head to descend and rotate
- Limits mobility (so not ideal for early labour)
- Accidental dural puncture in 1%
- If subarachnoid space is accidentally reached (spinal tap) –> can cause leakage of CSF –> spinal headache
- Felt on top of head; relieved by lying flat and exacerbated by sitting upright
- Bladder dysfunction if bladder is allowed to overfill (because woman is unaware of needing to pee)
- Overdistension of detrusor can damage it permanently
- To avoid this most women are catheterised
- Hypotension
- Rectified with fluid boluses, and sometimes vasopressors
- Occasionally leads to foetal compromise
- Accidental total spinal anaesthesia (injection of epidural doses of LA into subarachnoid space)
- Leads to severe hypotension, resp failure, unconsciousness, death if not treated immediately
- Mother requires intubation, ventilation and circulatory support
- Hypotension treated with IV fluids, vasopressors and positioning woman on L side
- Urgent delivery of baby may be needed (helps maternal resuscitation)
- Avoided by test dose
- Spinal haematoma and neurological complications (rare)
- Short-term resp depression of baby (due to opioids)
- Little evidence for epidurals causing back pain after delivery
Describe spinal block and pudendal nerve block in labour
Spinal analgesia (spinal block):
- More effective than epidural and faster onset
- Spinal needle is passed through epidural space, through dura and into subarachnoid space (contains CSF)
- Small volume of LA injected
- Needle withdrawn
- Not used for routine analgesia in labour
- May be used for C-sections (if epidural is not already in place), trial of instrumental deliveries (in theatre), manual removal of retained placenta, repair of difficult perineal tears
- May cause hypotension and total spinal analgesia (rare)
Pudendal nerve block:
- LA injected bilaterally around pudendal nerve where it passes the ischial spine
- Suitable for low-cavity instrumental vaginal deliveries
Define abnormal labour
Labour is abnormal if there is:
- poor progress (delay in cervical dilatation or descent)
- and/or foetal compromise
- Also not considered normal if there is malpresentation, multiple pregnancy, a uterine scar or IOL
What is used to plot the progress of labour and detect abnormal progress?
Partograms
Name the patterns of abnormal labour
- Prolonged latent phase:
- Primary arrest:
- Secondary arrest:
- Arrest in the second stage of labour:
What is Prolonged latent phase?
- When latent phase is > 8hrs
- More common in primiparous women
- Due to delay in the chemical processes that cause cervical softening and effacement
- Managed at home with simple analgesics, mobilisation and reassurance
- Artificial rupture of membranes or oxytocin infusion increase the likelihood of poor progress later in labour and need for C-section
- Partogram should not be commenced until latent phase is complete
What is Primary arrest?
- Poor progress in the active 1st stage of labour (<2cm cervical dilatation/4hrs)
- More common in primiparous women
- Usually caused by inefficient uterine contractions; also caused by cephalopelvic disproportion, malposition and malpresentation
What is Secondary arrest?
- Progress in active 1st stage is initially good but then slows down/stops, usually after 7cm dilation
- Usually caused by foetal malposition, malpresentation or cephalopelvic disproportion; can sometimes be caused by inefficient uterine contractions
What is Arrest in the second stage of labour?
- Delivery is not imminent after the usual interval of pushing in the second stage of labour
- Birth should happen within 3hrs of start of 2nd stage (nulliparous) or 2hrs (multiparous)
- Delay is diagnosed if birth not imminent within 2hrs of pushing for nulliparous or 1hr for multiparous
- May be due to inefficient uterine activity, malposition, malpresentation, cephalopelvic disproportion, a resistant perineum, maternal exhaustion, fear or pain
What is Poor Progress in the 1st Stage of Labour?
What are the causes of Poor Progress in the 1st Stage of Labour?

What is Poor Progress in the 2<u>nd</u> Stage of Labour ?
Birth not imminent within 2hrs of pushing for nulliparous or 1hr for multiparous
What are the causes of Poor Progress in the 2nd Stage of Labour?

What are the Management options for delay in 2nd stage of labour?
- Regular reviews of progress and foetal wellbeing; continued pushing with encouragement
- Oxytocin to augment contractions
- Episiotomy for a resistant perineum
- Instrumental vaginal birth
- C-section
What are the Risk factors for foetal compromise in labour?
- Placental insufficiency, multiple pregnancy, maternal DM, cholestasis of pregnancy, infection, oligohydramnios
- Prematurity, postmaturity, IUGR
- Prolonged labour, augmentation with oxytocin/hyperstimulation, cord prolapse, uterine rupture
How is foetal compromise recognised?
-
Meconium staining
- Significant if thick, fresh, dark green/bright green/black or particulate
- Thin and light meconium is likely due to foetal gut maturity
-
Abnormal CTG
- High false positive rate
Define venous thromboembolism in pregnancy
Venous thromboembolism is a collective term for deep vein thrombosis or pulmonary embolism in pregnancy
What is the aetiology of venous thromboembolism in pregnancy?
Pregnancy results in 6-10x increased risk of VTE
- Due to increased levels of clotting factors VIII, IX, X and fibrinogen, and decreased protein S and ATIII
- This means pregnancy is a hypercoagulable state (to reduce risk of PPH), exacerbated by uterus putting pressure on IVC in late pregnancy and immobility (esp in puerperium)
- Most DVTs form in proximal veins of L leg (due to compression of uterus on L iliac vein)
- The highest risk is post-partum (as these changes become more pronounced as pregnancy progresses)
What are the RFs for VTE in pregnancy?
- General: maternal age, thrombophilia, obesity, Hx/FHx DVT, smoking, immobility, post-surgery
- Obstetric: multiple pregnancy, hyperemesis/dehydration, pre-eclampsia, C-section (esp emergency), instrumental delivery, prolonged labour, infection
What is the epidemiology of VTE in pregnancy?
Responsible for 1/3 maternal deaths in UK
Incidence is 0.1% without thromboprophylaxis; increases to 2% following emergency C-section
What are the symptoms of VTE in pregnancy?
- DVT:
- Unilateral calf pain, erythema and swelling
- PE:
- Sudden onset dyspnoea, pleuritic chest pain, haemoptysis
- Signs of DVT
What are the Ix for ?VTE in pregnancy
- Measure calf circumference (to identify unilateral swelling)
-
Bloods: FBC, U&Es, LFTs, clotting
- Don’t do D-dimer (raised in pregnancy)
-
DVT:
- Compression duplex USS
-
PE:
- ABG (hypoxia, hypercapnia)
- ECG (sinus tachycardia, S1Q3T3)
- CXR, duplex USS
- If duplex USS is positive diagnostic
- If duplex USS is negative V/Q scan or CTPA
- Consider thrombophilia screen
What is the Mx of VTE in pregnancy?
Prophylaxis:
- All women risk assessed in early pregnancy, then repeated in intrapartum and postnatal periods
- All women: advised to avoid dehydration, mobilisation
- If LMWH is contra-indicated: compression stockings
Treatment:
- Massive PE:
- ABCDE, senior help
- IV unfractionated heparin; rarely may need thrombolysis
- Haemodynamically stable:
- SC LMWH (enoxaparin)
- Given on clinical suspicion (before diagnosis confirmed)
- If confirmed VTE:
- Continue LMWH until 6wks postpartum; can convert to warfarin 3wks after delivery
- Discontinue at start of labour or 24hrs before planned delivery
- NB NOACs are not licenced in pregnancy; warfarin is teratogenic
- SC LMWH (enoxaparin)
What is the antenatal assessment of VTE in pregnancy?

What is the antenatal assessment of VTE in pregnancy?
What is the postnatal assessment of VTE in pregnancy?

What are the complications of VTE in pregnancy?
Complications:
- Death (15 maternal deaths/yr)
- Effects of long-term anticoagulation
- Post-thrombotic leg syndrome (may be prevented with compression stockings
Define diabetes in pregnancy
Pre-existing or new-onset diabetes in pregnancy (gestational diabetes mellitus)
Definitions of GDM vary:
- NICE 2015: fasting glucose ≥5.6mmol/l and/or 2hr (post 75g glucose load) of 7.8mmol/l
- WHO 2013: fasting glucose ≥5.1mmol/l and/or 1hr (post 75g glucose load) of 10.0mmol/l or 2hr of 8.5mmol/l
What is the aetiology of diabetes in pregnancy?
Gestational diabetes:
- In normal pregnancy, insulin resistance increases (due to altered carbohydrate metabolism and antagonistic effects of human placental lactogen, progesterone and cortisol)
- Usually, pancreatic beta cells can compensate for increased insulin demands → 30% increase
- In GDM, there is deficient beta-cell response → insufficient insulin secretion to compensate for the increased demands
- Women without DM but with potentially impaired glucose tolerance may deteriorate enough to have GD
NB glycosuria may occur at physiological blood glucose concentrations in pregnancy
What are the risk factors for diabetes in pregnancy?
GDM RFs:
- increasing age,
- ethnicity (South Asian, Afro-Caribbean),
- obesity,
- smoking,
- PCOS,
- FHx T2DM,
- lack of physical activity,
- prior GDM,
- previous macrosomic baby (may be due to unrecognised GDM)
What is the epidemiology of diabetes in pregnancy?
Pre-existing DM affects 1% pregnant women; GDM complicates 5% of pregnancies
What are the signs and symptoms of diabetes in pregnancy?
- GDM is usually asymptomatic; identified on screening
- If symptomatic, features are the same as other DM (polyuria, polydipsia, fatigue)
On examination:
- Increased SFH (macrosomia/polyhydramnios)
What are the Ix for ?diabetes in pregnancy?
-
Pre-existing DM:
- Detailed anomaly scan, foetal cardiac scan
- Monitor for complications:
- Retinal screening at booking, 16-20 weeks and 28 weeks
- Renal screening
- Monitor for pre-eclampsia
-
GDM:
- Screening with OGTT
- Fasting plasma glucose measured, 75g glucose drink is given, measure glucose after 2hrs
- Usually targeted at high-risk groups: ethnic groups at high risk, FHx, maternal obesity, PCOS, previous macrosomia
- OGTT is offered at:
- Booking: if previous GDM
- 24-28 weeks: if risk factors of previous GDM
- At any point during pregnancy: if 2+ glycosuria on one occasion, or 1+ on 2 occasions
- Screening with OGTT
What is the Mx of pre-existing diabetes in pregnancy?
Pre-existing DM:
- Pre-conceptual:
- Aims to decrease the risk of complications (esp congenital malformation)
- Education about the complications
- Optimisation of glycaemic control (to achieve HbA1c <42mmol/mol); optimise diet
- High-dose folic acid (5mg/d)
- Pre-conception adjustments to medications, e.g. ACEi and statins are contraindicated
- MDT review for patients with vascular complications; counsel about additional complications
- During pregnancy:
- MDT approach → consultant-led, obstetrician, physician, specialist midwives and nurses, dietitian
-
Strict blood glucose control
- → monitoring encouraged 7x/day (before and after meals)
- Aim for <5.3mmol/l before meals; <7.8mmol/l after meals
- Insulin requirements usually increase increase insulin/metformin dose in 2nd half of pregnancy
-
Monitor and prophylaxis for complications of DM:
- Retinal and renal screening; monitor for pre-eclampsia
- Aspirin from week 12 (reduce risk of pre-eclampsia)
-
Foetal surveillance:
- Detailed anomaly scan at 20wks with cardiac assessment
- Serial growth scans (for macrosomia, polyhydramnios, IUGR)
-
Plan for delivery:
- Aim for vaginal at 38-39wks; 50% have C-section due to macrosomia/maternal complications
- Deliver on labour ward with NICU facilities
- Sliding scale of insulin and glucose in labour (if insulin-dependent)
- Maintain maternal glucose at 4-7mmol/l
- Postnatally:
- Return to pre-pregnancy doses of medications
- Warn patients of increased risk of hypoglycaemia in postnatal period (esp if breastfeeding)
What is the Mx of GDM?
Gestational DM:
- Principles of management are the same as pre-existing DM (same blood glucose levels, monitoring, foetal surveillance, education, delivery etc.)
- During pregnancy:
-
Strict blood glucose control:
- Diet and exercise (1st line)
- Slow-release carbohydrates, fruit and veg
- Metformin
- If uncontrolled by diet and exercise
- Consider glibenclamide if metformin is not tolerated/ineffective and insulin has been declined
- Insulin
- If uncontrolled by diet and exercise or SEs of metformin
- Diet and exercise (1st line)
-
Strict blood glucose control:
- Postnatally:
- Discontinue metformin/insulin after birth
- Exclude T2DM after pregnancy fasting glucose 6 weeks after birth, then yearly tests
- OGTT at booking and 24-28weeks in subsequent pregnancies
What are the complications of diabetes in pregnancy?
- Foetal complications:
-
Only in pre-existing DM: Congenital abnormality → 2-4x increased risk, esp neural tube and cardiac defects
- Critical period is organogenesis (often before pregnancy is confirmed)
- Foetal macrosomia (due to foetal hyperinsulinaemia so increased fat deposition) → can cause traumatic delivery and shoulder dystocia
- Stillbirth → 5x increased risk
- Polyhydramnios (due to increased foetal urine output)
- Neonatal hypoglycaemia (due to withdrawal of maternal glucose while foetal insulin levels remain high (because foetus had been compensating for high glucose))
- Respiratory distress syndrome (due to decreased lung maturation)
- Neonatal jaundice
-
Only in pre-existing DM: Congenital abnormality → 2-4x increased risk, esp neural tube and cardiac defects
- Maternal complications:
- Related to severity of diabetic-related vascular disease preceding the pregnancy
- Risk of pre-eclampsia increased 3x
- Women with diabetic retinopathy are at risk of progression careful surveillance
- Risk of deterioration of established nephropathy
- Worsening of ischaemic heart disease
- Increased infection risk (UTI, wound, endometrial)
- Severe hyper/hypoglycaemia and DKA
- Increased operative delivery rate
- GDM complications are less severe than in pre-existing DM (because complications relate to glucose levels)
GDM recurs in up to 80% pregnancies; 50% diagnosed with T2DM within 10yrs
Define thyroid disease in pregnancy
Hypothyroid or hyperthyroid in pregnancy
What is the aetiology of thyroid disease in pregnancy?
During pregnancy there is increased TBG (due to oestrogen) and stimulation of TSH receptor by hCG → increased total T3/4 (not free T3/4 because more is bound to TBG)
- Thyroxine levels rise from 6-12wks and peak by mid-gestation; reverse changes are seen with TSH
- Foetus begins producing TSH from week 12; very little until week 18-20 when it increases gradually
- Increased T3/4 in mother ensures adequate supply to foetus
- In pregnancy, iodide losses through urine and to foetus contribute to a state of relative iodine deficiency
- Therefore, additional 250ug/d is recommended in pregnancy not always achieved
Hypothyroidism:
- Most common cause worldwide is iodine deficiency; most common cause in developed world is autoimmune (Hashimoto’s) thyroiditis
Hyperthyroidism:
- Most common cause is Grave’s disease (autoimmune)
- May worsen in 1st trimester due to hCG stimulation of TSH receptors; may improve in 2nd half due to falling titre of thyroid-stimulating antibodies
- Other causes are toxic adenoma, toxic multinodular goitre, subacute thyroiditis
- Transient gestational hyperthyroidism: self-limiting thyrotoxicosis due to hCG stimulation of thyroid gland
- Resolves as hCG falls → does not need treatment
Postpartum thyroiditis:
- Syndrome of thyroid dysfunction occurring within the first 12 months of delivery, due to the postpartum immunological rebound that follows the immune tolerant state of pregnancy
- Similar pathology to Hashimoto’s
- RFs: autoimmune conditions
What is the epidemiology of thyroid disease in pregnancy?
- 2-3% have subclinical hypothyroidism; 0.5% have overt clinical hypothyroidism
- 0.5% have hyperthyroidism
- Up to 10% develop postpartum thyroiditis
What are the signs and symptoms of thyroid disease in pregnancy?
- Many symptoms resemble normal pregnancy → can be difficult to detect new presentations
- Hypothyroidism: fatigue/lack of energy, cold intolerance, constipation, dry skin, brittle hair, low mood
-
Hyperthyroidism: tremor, sweating, insomnia, weight loss, anxiety, heat intolerance
- On examination (depending on cause): goitre, Grave’s opthalmopathy, tachycardia, HTN, pretibial myxoedema
-
Postpartum thyroiditis:
- 30% have subclinical or overt hyperthyroidism about 1-4 months postpartum, then hypothyroidism (usually lasts 4 months) may present as postnatal depression
- 30% have only hyperthyroidism; 40% have only hypothyroidism
What are the Ix for ?thyroid disease in pregnancy?
-
TSH, serum free T4/3, thyroid antibodies
- TSH levels are trimester-dependent; measure free T3/4 rather than total
- TSH-receptor antibodies: Grave’s
-
Antithyroid peroxidase (TPO) antibodies: Hashimoto’s
- Also found in 90% women with postpartum thyroiditis; 50% with antibodies develop thyroid dysfunction postpartum → check in postpartum women with mood changes
- Consider thyroid USS
- Radioactive iodine uptake scans are contraindicated in pregnancy and breastfeeding
What is the Mx of hypothyroidism in pregnancy?
Hypothyroidism:
- Continue/start thyroxine
- Doses increased from 0.10-0.15mg/d until TSH is in normal range
- TSH monitored in each trimester; more often if dose adjustments needed
What is the Mx of hyperthyroidism in pregnancy?
Hyperthyroidism:
- Aim to maintain mild hyperthyroidism in the mother to prevent foetal hyperthyroidism
- No treatment is needed for subclinical or mild hyperthyroidism
-
Carbimazole or propylthiouracil
- Use lowest acceptable dose → can cross placenta to cause foetal hypothyroidism (less common in propylthiouracil – preferred)
- Regularly check maternal WBC (can cause agranulocytosis)
- Monitor TSH carefully → doses often reduced in 2nd half of pregnancy
- Breastfeeding encouraged (little excretion into breast milk) but monitor neonatal thyroid function
- Beta-blockers initially until antithyroid drugs take effect
- Radioactive iodine is contraindicated (destroys foetal thyroid)
What is the Mx of post-partum thyroiditis in pregnancy?
Postpartum thyroiditis:
- May require propranolol for hyperthyroid phase
- Hypothyroid treatment for hypothyroid phase
What are the complications of hypothyroidism in pregnancy?
Hypothyroidism (if uncorrected):
- Maternal:
- Anaemia
- Pre-eclampsia
- Placental abruption
- PPH
- Foetal:
- Prematurity, low BW
- Recurrent miscarriage
- Neurological maldevelopment, developmental delay
What are the complications of hyperthyroidism in pregnancy?
Hyperthyroidism (if uncorrected):
- Maternal:
- HTN, pre-eclampsia
- Cardiac failure
- Thyroid storm
- Life-threatening; may be precipitated by labour; can mimic impending eclampsia
- Presents with sweating, pyrexia, AF, HTN, hyperglycaemia, HF
- Treat with: ABCDE, propylthiouracil, high-dose steroids, beta-blockers, fluids
- Foetal:
- Miscarriage, stillbirth
- Preterm labour
- IUGR
- Thyroid dysfunction (due to TSHR antibodies crossing placenta in Grave’s) neonatal review
What are the complications of well-controlled thyroid disease in pregnancy?
Good thyroid control does not have complications
What are the complications of post-partum thyroiditis?
Postpartum thyroiditis may persist → permanent hypothyroidism in 30% after 3yrs and 50% after 7-10yrs
Define anaemia in pregnancy
- First trimester Hb <110g/l,
- 2nd/3rd trimester Hb <105g/l or
- postpartum Hb <100g/l
What is the aetiology of anaemia in pregnancy?
Increased plasma volume (out of proportion to RBC mass) predisposes pregnant women to develop anaemia
Causes of anaemia:
-
Microcytic (MCV <76): iron deficiency, thalassaemia, sideroblastic anaemia
- IDA is most common: due to nutritional deficiency or low stores; physiological requirements for iron in pregnancy are 3x higher than non-pregnant; requirements increase as pregnancy advances
- Normocytic (MCV 76-96): anaemia of chronic disease, marrow infiltration, haemolytic anaemia, CKD
- Macrocytic (MCV >96): B12/folate deficiency, alcohol, reticulocytosis, hypothyroidism
What are the RFs of anaemia in pregnancy?
- anaemia during previous pregnancy,
- poor diet,
- low socioeconomic status,
- increasing age,
- haemoglobinopathies
What is the epidemiology of anaemia in pregnancy
Very common 25% antenatally; 33% postpartum
What are the signs and symptoms of anaemia in pregnancy?
- May be asymptomatic (detected on FBC)
-
Dizziness, fatigue, dyspnoea
- These are also all features of a normal pregnancy
-
On examination:
- Pallor (best identified in the mucosa of the tongue and mouth)
- Koilonychia (spoon-shaped nails)
- Angular cheilitis (ulceration at the corners of the mouth)
- Tachycardia
What are the Ix for ?anaemia in pregnancy?
- Screened for anaemia at booking and 28wks (and 20wks if multiple pregnancy)
- Screen for sickle cell and thalassaemia at booking
-
FBC → Hb level and MCV
- If low MCV the probable cause is IDA
- Normal MCV with low Hb is typical of pregnancy
- Iron studies: ferritin, serum iron (low in IDA), total iron binding capacity (high in IDA)
-
Further Ix depend on suspected cause:
- Blood film
- Haemoglobinopathy screening (Hb electrophoresis)
- Folate & B12 levels
What is the Mx of IDA in pregnancy?
-
Advice:
- Animal protein (red meat, eggs, milks) and leafy greens
- Increase vitamin C to aid absorption; decrease tea/coffee
-
Oral iron (ferrous sulphate, ferrous fumarate)
- For treatment and diagnosis
- Repeat FBC after 4 weeks → if improves suggests it was IDA; if no improvement look for other cause (e.g. B12/folate deficiency)
- Advice: take with vit C (enhance absorption); tea/coffee inhibits absorption
- Supplementation should continue for at least 3 months and 6 weeks postpartum
- Can cause constipation/black stools
- Parenteral iron infusion (Ferinject) if poor compliance or malabsorption
- For treatment and diagnosis
What is the Mx of IDA in pregnancy?
-
Advice:
- Animal protein (red meat, eggs, milks) and leafy greens
- Increase vitamin C to aid absorption; decrease tea/coffee
-
Oral iron (ferrous sulphate, ferrous fumarate)
- For treatment and diagnosis
- Repeat FBC after 4 weeks → if improves suggests it was IDA; if no improvement look for other cause (e.g. B12/folate deficiency)
- Advice: take with vit C (enhance absorption); tea/coffee inhibits absorption
- Supplementation should continue for at least 3 months and 6 weeks postpartum
- Can cause constipation/black stools
- Parenteral iron infusion (Ferinject) if poor compliance or malabsorption
- For treatment and diagnosis
What is the Mx of B12 deficiency in pregnancy?
-
Advice:
- Found in animal products (fish, meat, eggs) and fortified cereals
-
IM hydroxocobalamin (B12) injections
- 3x/wk for 2wks, then once every 3 months
- Postnatal follow-up with GP
What is the Mx of folate deficiency in pregnancy?
-
Advice:
- Found in vegetables (not if overcooked), chickpeas, bananas, citrus fruit, mushrooms, fortified foods
- Folic acid (5mg/d)
What is the Mx of anaemia in pregnancy due to beta thalasaemia?
- Carriers may be asymptomatic when not pregnant but more anaemic during pregnancy
- Regular Hb monitoring & blood transfusions as required
- Folate supplementation (5mg/d)
- Screening for thalassaemia major
What is the Mx of anaemia in pregnancy due to sickle cell disease?
- Regular Hb monitoring & blood transfusion as required
- Folate supplementation (5mg/d)
- Prophylactic antibiotics through pregnancy and afterwards
What are the complications of anaemia in pregnancy?
-
Maternal complications:
- Poor work capacity/performance
- Susceptibility to infection
- Cardiac failure
- Sickle cell: increased risk of sickle cell crisis/stroke/PE
-
Foetal complications:
- Premature delivery and low BW
- Developmental problems
- Sickle cell: stillbirth rates 10%
What is epilepsy in pregnancy?
History of epilepsy diagnosis in pregnancy
What is the impact of pregnancy on pre-existing epilepsy?
Pregnancy has no consistent effect on epilepsy → some have more fits, some have less, some no difference
- Increased seizures are related to:
- Compliance issues with antiepileptics (fear of congenital abnormalities)
- Increased renal and hepatic drug clearance; increased Vd lower drug levels
- Decreased absorption (e.g. during labour, nausea and vomiting)
hat is a concern of pregnancy in a person with epilepsy?
A concern of epilepsy in pregnancy is related to the teratogenic effects of anticonvulsants
- All anticonvulsants are associated with 2-3x risk increased risk of congenital abnormality
- Polytherapy increases the risk of congenital abnormality by 3% for each additional anticonvulsant
- The major associated abnormalities are neural tube defects, facial clefts and cardiac defects
- Sodium valproate has highest risk of neural tube defects; levetiracetam and lamotrigine are safest
- Anticonvulsants may also cause a specific syndrome (developmental delay, growth restriction)
- Despite the risks, failure to take anticonvulsants may cause increased seizures foetal hypoxia
- The risk of seizures is greater than the risk of anticonvulsants (for mother and foetus)
What investigations are indicated in a pregnancy person with epilepsy?
-
Bloods (effects of anticonvulsants):
- serum anticonvulsant levels,
- FBC (may increase MCV),
- serum folate,
- LFTs
- Detailed foetal anomaly scan +/- foetal echo (if taking anticonvulsants)
What is the Mx of epilepsy in pregnancy?
Pre-pregnancy:
- Referral to specialists (obstetric neurology)
- Optimise control on least-teratogenic lowest-dose monotherapy if possible
- Antiepileptics often remain the same (risks of changing may outweigh benefits) if well-controlled
- May need to monitor levels
- If seizure-free for 2 years, may consider discontinuing medication
- Advice:
- Stress importance of compliance with medication
- Explain risks of congenital malformation and risks of recurrent seizures
- 5mg folic acid
Pregnancy:
- Same principles outlined in pre-pregnancy
- If seizures occur may require diazepam/lorazepam; dose of antiepileptics may need to be increased
Postnatal:
- IM neonatal vitamin K
- Gradually reduce dose of medications increased in pregnancy to baseline
- Encourage breastfeeding, but best avoided for a few hours after taking anticonvulsants
- Give advice about safe handling of the neonate don’t bathe alone etc.
What are the complications of epilepsy in pregnancy?
Complications:
- Increased seizure frequency causes 5 maternal deaths/yr in UK; foetal hypoxia
- Teratogenicity related to antiepileptics
- Increased risk of childhood epilepsy
- Haemorrhagic disease of the newborn
What is the prognosis of epilepsy in pregnancy?
Poorly controlled epileptics are most likely to deteriorate in pregnancy; long-term seizure-free patients are likely to have no change
When is the highest risk of seizures in a pregnant person with epilepsy?
Highest risk of seizures is peripartum
What are the causes of seizures in pregnancy?
causes of seizures in pregnancy include:
- epilepsy,
- eclampsia,
- encephalitis/meningitis,
- SOL,
- drug/alcohol withdrawal,
- metabolic abnormalities (e.g. hypoglycaemia)
Define UTI in pregnancy
- UTI: infection of the urinary tract.
- Cystitis is bladder infection;
- pyelonephritis is kidney infection
Define bacteruria in pregnancy
Bacteriuria: asymptomatic presence of bacteria in the urine
What is the aetiology of UTI in pregnancy
Most common organism is E. coli; others include Streptococci, Proteus, Pseudomonas & Klebsiella
Asymptomatic bacteriuria can progress to UTI or pyelonephritis
- More likely to lead to pyelonephritis in pregnancy (20%) due to dilatation of renal calyces and ureters
- Pyelonephritis is associated with low BW and preterm labour
What are the RFs for UTI in pregnancy?
- Hx recurrent cystitis,
- renal tract abnormalities (duplex system, scarred kidneys, ureteric damage),
- DM,
- bladder emptying problems (e.g. MS)
What is the epidemiology of UTI in pregnancy
- UTIs are common in pregnancy (up to 7%)
- 8% women have asymptomatic bacteriuria;
- pyelonephritis affects 1-2% women
What are the signs and symptoms of bacteruria in pregnancy?
- Bacteriuria
- Asymptomatic
What are the signs and symptoms of UTI in pregnancy?
- Symptoms may differ in pregnancy → classic presentation of dysuria, frequency and haematuria not often seen
- May present with lower back pain, loin tenderness, general malaise, flu-like symptoms
What are the signs and symptoms of pyelonephritis in pregnancy?
- Dehydration,
- very high temp (>38.5),
- systemic disturbance
- Occasionally shock
What are the Ix for ?UTI/pyelnephritits in pregnancy?
-
MSU → MC&S
- Urine dip done at each visit (nitrites and leukocytes suggest UTI)
- Urine is cultured at booking and if urine dip suggests UTI/clinical suspicion
- Many labs define a UTI as >105 colony forming units (cfu)/ml
- FBC, U&Es, creatinine (esp if pyelonephritis is suspected)
- CTG (if pyelonephritis is suspected)
- Consider more detailed renal Ix after delivery for recurrent UTIs
- E.g. renal USS, DMSA, cystoscopy
What is the Mx of Asymptomatic bacteriuria/UTI in pregnancy?
-
Antibiotics:
- Offer immediately if clinical suspicion; may change depending on sensitivities
- Refer to local guidelines, but usually: nitrofurantoin (avoid at 36+wks), cefalexin or amoxicillin (only if culture results show susceptibility)
- 7-day course
- Drink plenty of clear fluids
- Simple analgesia, e.g. paracetamol
What is the Mx of Pyelonephritis in pregnancy?
- Admission, ABCDE approach, senior help
- IV fluids
- Opiate analgesia
- IV antibiotics
- Refer to local guidelines: often cephalosporins (e.g. ceftriaxone)
- Gentamycin is sometimes used careful monitoring as potential foetal toxicity
What is the Mx of Recurrent UTIs in pregnancy?
- May need MSU sent to lab at each antenatal visit
- Low dose prophylactic antibiotics (e.g. nitrofurantoin) – guided by sensitivities
What are the complications of UTI & pyelonephritis in pregnancy?
Complications:
- Progression to pyelonephritis → shock, renal dysfunction
- Pyelonephritis is associated with preterm labour and low BW
Normally managed well
Define obesity in pregnancy
BMI ≥30
- BMI 30.0 – 34.9: class 1 (moderate);
- BMI 35.0 – 39.9: class 2 (severe);
- BMI 40+: class 3 (morbid)
What is the Mx of obesity in pregnancy?
Pre-conceptual:
- Pre-conceptual weight loss is ideal
- High dose folic acid (5mg)
- Vitamin D
During pregnancy:
- Pregnancy is considered high-risk (esp if BMI >35) → consultant-led care
- Dietary advice:
- Advise that the mother is not eating for 2 (maintain normal/small portion size), fruit and veg, low fat/sugar, high fibre
- Exercise advice:
- Aerobic and strength and conditioning exercise is recommended
- Avoid contact sports
- Aim to maintain weight (loss in pregnancy is impractical and likely to cause malnutrition)
- For normal weight women, the recommended total weight gain in pregnancy is 11-16kg; it is 7-11kg in overweight women and 5-9kg in obese women
- Thromboprophylaxis if indicated (see separate section)
- Screen for GDM; close BP surveillance with appropriately-sized cuff
What are the complications of obesity in pregnancy?
- Maternal:
- Difficulty accurately assessing growth/anatomy of foetus
- Increased risk of GDM, hypertensive disorders and VTE
- Difficulty with analgesia in labour (epidurals/spinals/GA) and foetal monitoring
- Increased instrumental/C-section rate
- Wound breakdown/infection
- Postnatal depression
- Foetal:
- Increased risk of congenital malformations (esp if BMI >40)
- Macrosomia risk of traumatic birth injury, shoulder dystocia
- IUGR
- 20% risk of miscarriage; increased risk of stillbirth and perinatal mortality
- Increased risk of childhood obesity and DM later in life
Define mastitis in pregnancy
Mastitis: inflammation of the breast, with or without infection.
Define breast abscess in pregnancy
Breast abscess: localised area of infection with a walled-off collection of pus
- May or may not be associated with mastitis
What is the aetiology of mastitis & breast abscess in pregnancy?
Mastitis is commonly related to breast feeding
- Blocked duct obstructs milk flow and distends the alveoli
- If the pressure persists, the milk extravasates into the perilobular tissue inflammation
Abscess is caused by bacteria colonising the skin, e.g. S. aureus, coagulase-negative Staph
What are the RFs of mastitis & breast abscess in pregnancy?
- lactating/breast feeding,
- poor breastfeeding technique,
- nipple injury,
- previous mastitis,
- skin infection,
- being a S. aureus carrier
What is the epidemiology of mastitis & breast abscess in pregnancy?
- Mastitis is most common in lactating women
- Breast abscess develops in up to 10% of women with mastitis
What are the signs and symptoms of mastitis in pregnancy?
-
Painful, erythematous, hot swelling of the breast
- Pain is often sharp and shooting, especially when breast feeding
- Fever
- Decreased milk outflow
What are the Ix for ?mastitis in pregnancy?
- Usually clinical diagnosis
- USS: to identify underlying abscess
- Needle aspiration drainage of breast abscess: purulent fluid indicates breast abscess
- Bloods (FBC, U&Es, CRP/ESR) and blood culture for systemic infection
What is the Mx of mastitis in pregnancy?
- Advice: massage of the breast (towards nipple), breastfeeding advice, bed rest, warm/cold compress
- Antibiotics – oral penicillin, vancomycin for MRSA
- Analgesia
What is the Mx of breast abscess in pregnancy?
- Needle aspiration
- Incision and drainage if aspiration fails or abscess is >5cm diameter
What are the complications of mastitis in pregnancy?
- Cessation of breastfeeding, reduced lactation
- An abscess is a complication of mastitis
- Sepsis (if abscess)
Define hyperemesis gravidarum
Persistent and severe vomiting during pregnancy, which leads to
- weight loss,
- dehydration
- electrolyte imbalances
What is the aetiology of hyperemesis gravidarum?
Nausea and vomiting of pregnancy (“morning sickness”) starts between 4-7 weeks gestation, peaks in week 9, and settles by week 20 (in 90% women)
- Hyperemesis gravidarum is the most severe form → diagnosed when there is severe and prolonged nausea and vomiting, with:
- >5% pre-pregnancy weight loss
- Dehydration, and
- Electrolyte imbalances
It is due to rapidly increasing levels of hCG (released by the placenta)
- hCG stimulates the CTZ in the brainstem
- There are also genetic, immunological and biosocial components
What are the RFs for hyperemesis gravidarum?
- 1st pregnancy,
- Hx/FHx of hyperemesis gravidarum,
- multiple pregnancy,
- gestational trophoblastic disease
What is the epidemiology of hyperemesis gravidarum?
- 75% pregnant women experience nausea and vomiting;
- 35% absent from work at least once
- Hyperemesis gravidarum occurs in 0.5% pregnancies
What are the signs and symptoms of hyperemesis gravidarum?
-
Severe nausea and vomiting
- Ask about duration, frequency, oral intake, urine output, bowel movements
- >5% weight loss
-
On examination:
- Signs of dehydration: dry mucous membranes, decreased skin turgor
- Signs of muscle wasting
What are the Ix for ?hyperemesis gravidarum?
- Basic observations: temp, pulse, BP, RR, O2
- Weight
- Scoring system to classify severity, e.g. pregnancy-unique quantification of emesis (PUQE)
- Urine dip/culture (exclude UTI, check for ketones (caused by starvation))
-
Bloods: FBC, U&Es, LFTs, TFTs, ketones, glucose, ABG
- Hypernatraemia, hypochloraemia, elevated urea and creatinine, exclude liver disease and infection
- ABG to exclude metabolic disturbances and monitor severity
-
USS:
- Confirm viability and gestation; exclude multiple pregnancy and gestational trophoblastic disease
What is the Mx of mild hyperemesis gravidarum?
- Manage in community
- Oral antiemetics
- 1st line: metoclopramide (max 5d), domperidone
- 2nd line: chlorpromazine
- H2 antagonists/PPIs for reflux/oesophagitis
- Oral rehydration
- Dietary modifications and reassurance
What is the Mx of moderate hyperemesis gravidarum?
Moderate (volume depletion or if community management has failed):
- Manage in ambulatory day care
- IV fluids
- 0.9% saline; add KCl as guided by electrolyte monitoring
- Parenteral antiemetics
- 1st line: metoclopramide (IV), ondansetron (IV)
- 2nd line: chlorpromazine (IM)
- Consider corticosteroids if no improvement (IV hydrocortisone then PO prednisolone)
- H2 antagonists/PPIs for reflux/oesophagitis
- Thiamine
- Psychological support
What is the Mx of severe hyperemesis gravidarum?
- As for moderate but inpatient management
- Thromboprophylaxis (for all women requiring admission)
What are the complications of hyperemesis gravidarum?
Complications:
- Electrolyte disturbance, Wernicke’s encephalopathy
- Mallory-Weiss tears
- VTE
- Psychological distress
- Increased risk of pre-eclampsia, IUGR, preterm birth
Define pregnancy of unknown location
A working diagnosis when the pregnancy test is positive but there are no signs of intrauterine pregnancy or ectopic pregnancy via TVUSS
What are the DDx for pregnancy of unknown location?
There are 3 differentials for PUL:
- Very early intrauterine pregnancy
- Miscarriage (aka spontaneously resolving pregnancy/failing PUL)
- Ectopic pregnancy
What is the epidemiology of pregnancy of unknown location?
- Most commonly caused by miscarriage;
- 20% are subsequently diagnosed with ectopic pregnancy
- Prevalence depends on quality of scanning at early pregnancy unit → higher quality reduces prevalence (diagnosed sooner)
What are the signs and symptoms of pregnancy of unknown location?
- Depends on the cause (see ectopic pregnancy and miscarriage)
- May be asymptomatic
What are the Ix for pregnancy of unknown location?
- Must be investigated to determine the location of the pregnancy
- Urine pregnancy test and TVUSS (should have been done for PUL to be diagnosed)
-
Consecutive serum hCG measurement (48hrs apart)
- If the initial hCG is >1500iU and there is no sign of intrauterine pregnancy on TVUSS, a viable intrauterine pregnancy is unlikely
- Decrease in serum hCG >50% after 48hrs:
- Likely miscarriage (hCG levels halve every 48hrs) → perform urine pregnancy test in 14d
- See miscarriage section
-
Increase in serum hCG >63% after 48hrs:
- Likely to be developing intrauterine pregnancy (hCG doubles every 48hrs) → repeat TVUSS in 7-14d
-
Change in hCG between these limits (50% decline – 63% rise):
- Refer for review in early pregnancy assessment service within 24hrs
- May be ectopic (rise in hCG is often suboptimal)
- See ectopic section
What is the Mx of pregnancy of unknown location?
- Admit if in pain or haemodynamically unstable (possible ectopic)
- Manage according to likely location (see separate sections)
- Information and support
- Advice on new/worsening symptoms;
- how to access emergency care;
- return if symptoms worsen etc.
What is the aetiology of multiple pregnancy?
May be classified according to number of foetuses (twins, triplets, etc.), number of fertilised eggs (zygosity), number of placentae (chorionicity), or number or amniotic cavities (amnionicity)
Multiple pregnancies can be dizygotic (70%) or monozygotic (30%)
-
Dizygotic (non-identical):
- Ovulation and fertilisation of >1 oocyte by different sperm
- Dichorionic diamniotic (DCDA): each foetus has its own placenta and amniotic cavity
- Placentae are always functionally separate but can become fused so appear as one
- Amniotic cavities are always separate; separated by thick 3-layer membrane
- May be the same sex or different sex
-
Monozygotic (identical):
- Single ovum is fertilised with subsequent division of the zygote
- The time of splitting determines the type of multiple pregnancy
- DCDA: splitting shortly after fertilisation (3d)
- Can’t determine if they are identical or not in utero, unless different genders
- Monochorionic diamniotic: splitting 4-8d after fertilisation
- Shared placenta; 2 amniotic cavities (but dividing membrane is thin (1 layer))
- Monochorionic monoamniotic: splitting 8-12d after fertilisation
- Shared placenta, shared amniotic cavity
- Conjoined twins: splitting after day 13
- DCDA: splitting shortly after fertilisation (3d)

What are the RFs for multiple pregnancy?
- assisted fertility (IVF),
- increasing maternal age
What is the epidemiology of multiple pregnancy?
- 3% live births;
- 10% of women >45yo
- 20% with IVF (rates proportional to number of embryos transferred)
- Vast majority (97%) are twin pregnancies; most of the remainder are triplet
What are the signs and symptoms of multiple pregnancy?
- Usually asymptomatic; incidental finding on USS
- Exaggerated complications of normal pregnancy (hyperemesis)
-
On examination:
- Large for dates,
- multiple foetal parts,
- more than 1 foetal heartbeat
What are the Ix for ?multiple pregnancy?
- Usually identified at 1st USS
- Dichorionic show lambda sign (triangular space between the 2 sacs); monochorionic show T sign (thin dividing septum)
- CTG is less reliable in twin pregnancies
What is the antenatal Mx of multiple pregnancy?
Pregnancy is managed as high risk → obstetrician-led care
- MDT: obstetricians, specialist midwives, ultrasonographers
Antenatal management:
- Serial USS for foetal growth
- Dichorionic: 4wkly from 24/40; monochorionic: 2wkly from 18/40
- Monitor FBC (increased risk of anaemia), BP (increased risk of pre-eclampsia), GTT (increased risk of DM)
- Routine iron and folic acid (due to increased demand)
- Careful assessment of congenital abnormalities at 20wk scan (increased risk)
- Abnormality in 1 foetus can be managed expectantly or by selective fetocide of the affected twin
What is the delivery Mx of multiple pregnancy?
Delivery:
- Make delivery plan early (risk of preterm delivery)
- Deliver at 37wks if possible (usually spontaneous labour before this; IOL may be needed)
- Mode of delivery:
- Vaginal: can be attempted if 1st twin is cephalic
- If malpresentation of 2nd twin:
- Breech delivery (if footling)
- ECV after delivery of 1st twin
- Internal podalic version if ECV unsuccessful (hand into uterus; pull foot through birth canal for breech delivery)
- 4% risk of emergency C-section for 2nd twin
- If malpresentation of 2nd twin:
- C-section: recommended if malpresentation of 1st twin, delayed delivery of 2nd twin, foetal distress, monoamniotic twins, higher order births (triplet and above)
- Vaginal: can be attempted if 1st twin is cephalic
- Intrapartum management:
- Continuous CTG; ensure 2 separate foetal heartbeats
- Ideally epidural analgesia (to allow for C-section/internal podalic version if needed)
- 2 neonatal resuscitation trolleys, 2 obstetricians, 2 paediatricians, anaesthetist present
- Aim for interval <30mins between delivery of twins; augment with oxytocin if needed
What are the complications of multiple pregnancy?
Maternal:
- All physiological changes in pregnancy are exaggerated →greater stress on maternal reserves
- Increased risk of hyperemesis, pre-eclampsia, anaemia, PPH, APH, DM, operative delivery, postnatal depression
- Financial costs
Foetal:
- Increased risk of congenital abnormalities
-
Pre-term delivery
- Either spontaneous or iatrogenic (due to complications)
- 60% DCDA are pre-term; higher in monochorionic
- Increased risk of late miscarriage and perinatal mortality (4x higher than singletons)
-
IUGR
- More difficult to manage → if only one twin is growth restricted, premature delivery may cause increased complications for the healthy twin
- In general, don’t deliver before 30wks (even if smaller twin may die)
-
Twin-to-twin transfusion syndrome (TTTS)
- Only in monochorionic twins
Monochorionic monoamniotic has highest rate of complications for twins (due to cord entanglement) → 20% perinatal mortality; hospitalise from 28wks
What is the aetiology of twin-to-twin transfusion syndrome?
- Due to unbalanced placental vascular connections between twins
- → if more occur in one direction than the other there is haemodynamic imbalance
- → polyhydramnios and hydrops in one twin, and oligohydramnios and IUGR in the other
What is the Mx of twin-to-twin transfusion syndrome?
- Management: tertiary referral, consider delivery if >26wks, laser ablation of vascular anastomoses, amnioreduction, septostomy
What are the complications of twin-to-twin transfusion syndrome?
- May cause twin anaemia-polycythaemia sequence if chronic
- Gradual development of anaemia in one twin and polycythaemia in the other, without characteristic oligohydramnios polyhydramnios pattern
What is rhesus disease?
Development of Rhesus antibodies in a Rhesus-negative mother after exposure to a Rhesus antigen on foetal RBCs
What is the aetiology of rhesus disease?
Rhesus disease is the most common type of RBC isoimmunisation, but more than 50 antigens can cause it
- Rh D antigen is most common, but others are Rh C, E, Kell, Kidd and Duffy
Occurs in Rh D -ve mothers who have been exposed to the blood of a Rh D +ve foetus by a sensitising event
- Sensitising events include: ectopic pregnancy, miscarriage, invasive obstetric testing (e.g. amniocentesis, CVS), antepartum haemorrhage, TOP, trauma, ECV, delivery, blood transfusion (very rare in UK)
- Exposure causes maternal production of IgM and then IgG antibodies against RhD (anti-D antibodies)
- This is called maternal isoimmunisation
- If the woman later becomes pregnant with a foetus who is RhD +ve, IgG antibodies cross the placenta → bind to foetal RhD on RBCs → foetal immune system destroys RBCs → foetal anaemia
- This is called haemolytic disease of the newborn
What are the RFs for rhesus disease?
- RhD -ve mother,
- RhD +ve father (to make foetus RhD +ve),
- previous pregnancy with sensitising event
What is the epidemiology of rhesus disease?
15% UK Caucasians are RhD -ve; 55% Caucasian males are heterozygous
- Therefore, 2/3 RhD -ve mothers would be expected to carry a Rh +ve foetus
Without prophylaxis, isoimmunisation occurs in 1%
What are the signs and symptoms of rhesus disease?
- Usually detected on antenatal screening
What are the the Ix for ?rhesus disease?
- Screening (ABO blood group, RhD typing and antibody screen) for all pregnant women at booking
What are the Ix indicated if a woman is RhD negative at booking?
- Repeat antibody screen at 28wks (if it was negative at booking) and after sensitising events
-
If positive RhD antibody screen (sensitised):
- Paternal RhD typing (if paternity is certain)
- If RhD positive → genotyping (to assess whether homo- or heterozygous)
- If heterozygous → 50% risk of Rh incompatibility → determine foetal Rh type (amniocentesis or free foetal DNA in maternal circulation)
- If homozygous → 100% risk of Rh incompatibility
- Antibody titres are monitored (correlates with severity)
- If titre reaches threshold for foetal anaemia → foetal monitoring for markers of anaemia (MCA Doppler, USS monitoring, cordocenesis)
- Paternal RhD typing (if paternity is certain)
- Determine whether fetomaternal haemorrhage occurred after a sensitising event (if not sensitised)
- Rosette test: used to rule out significant fetomaternal haemorrhage
-
Kleihauer test: determines amount of foetal blood in maternal circulation if rosette test +ve
- Used to determine how much anti-D to give after a sensitising event
What is the Mx for prevention of sensitisation in RhD -ve women?
-
Anti-D immunoglobulin (IM injection)
- Binds to foetal RhD +ve cells in maternal circulation → no immune response is stimulated
- Given to all RhD -ve women at 28wks, and following delivery (if baby is RhD +ve)
-
Given following a sensitising event, ideally within 72hrs (depending on event and gestation)
-
<12wks: indicated in ectopic pregnancy, molar pregnancy, TOP, heavy PV bleeding
- Not for all sensitising events because volume of foetal blood is small
-
12wks +: indicated for all sensitising events
- Dose guided by Kleihauer test
-
<12wks: indicated in ectopic pregnancy, molar pregnancy, TOP, heavy PV bleeding
-
Check Rh status of baby after delivery
- Cord blood for blood count, blood group and indirect Coombs test
What is the Mx of a RhD sensitised woman?
- Anti-D immunoglobulins are useless
- Close surveillance in subsequent pregnancy
- Paternal Rh type to assess risk in next pregnancy (see investigations)
- Close monitoring for signs of foetal anaemia in next pregnancy (see investigations)
What is the Mx of a foetus with probability of anaemia?
- Manage in tertiary centre; neonatologist present at delivery
- Consider delivery if >36wks
-
Foetal blood transfusion if too anaemic for delivery/<36wks
- Routes of transfusion: umbilical vein, intrahepatic vein, peritoneal cavity, foetal heart
- May need exchange transfusion after delivery
What are the complications of rhesus disease?
-
Foetal anaemia
- Signs: polyhydramnios, enlarged heart, hydrops foetalis, reduced foetal movements
-
Haemolytic disease of the newborn
- Can cause hyperbilirubinaemia and kernicterus
If sensitised, degree of foetal anaemia usually worsens for each subsequent pregnancy
What is oligohydramnios?
- Low level of amniotic fluid during pregnancy
- Defined as amniotic fluid index <5th centile for the gestational age, or deepest pool <2cm
What is oligohydramnios?
- Low level of amniotic fluid during pregnancy
- Defined as amniotic fluid index <5th centile for the gestational age, or deepest pool <2cm
What is the aetiology of oligohydramnios?
Volume of amniotic fluid increases steadily until 33wks, plateaus until 39wks then declines (volume at term is 500ml)
Amniotic fluid is comprised of foetal urine (main component), with contributions from the placenta and other foetal secretions (e.g. respiratory)
- Foetus swallows amniotic fluid passed out in urine repeats
- Problems with any structures that prevent this can lead to too much/too little fluid
- Anything that reduces urine production, blocks output from foetus, or allows fluid to leak can cause oligohydramnios
What are the main causes of oligohydramnios??
Main causes of oligohydramnios are:
- PROM/ruptured membranes (most common)
- Placental insufficiency/IUGR (reduced urine output because blood diverted to brain and away from kidneys)
- Renal agenesis (Potter’s syndrome), non-functioning kidneys (e.g. multicystic), obstruction
- Chromosomal abnormalities
- Post-term pregnancies
- TTTS (oligohydramnios in one twin; polyhydramnios in the other)
What are the signs and symptoms of oligohydramnios?
Symptoms of underlying cause, e.g. ruptured membranes
On examination:
- Abdo: decreased SFH, foetal parts easily palpable
- Speculum: assess for ruptured membranes if appropriate
What are the Ix for oligohydramnios?
-
USS
- For diagnosis
- Measure amniotic fluid index and maximum pool depth
- AFI: measure maximum depth in the 4 quadrants and add together (<10 is reduced volume; <5 is oligohydramnios)
- Maximum pool depth: vertical measurement
- Measure amniotic fluid index and maximum pool depth
- To exclude foetal anomalies
- For diagnosis
- Other Ix for cause, e.g. speculum for ruptured membranes, Doppler for placental insufficiency, karyotyping
What is the Mx of oligohydramnios?
Depends on underlying cause → treat cause
Term:
- Delivery (usually IOL)
Pre-term:
- Depends on cause
- Monitor with serial USS for growth, CTGs, delivery if necessary
What are the complications and prognosis of oligohydramnios?
Complications:
- Complications related to cause
- Labour: increased risk of CTG abnormalities, meconium aspiration, emergency C-section
- Neonate:
- Increased perinatal mortality
- Pulmonary hypoplasia
- Limb deformity/contractures (as can’t move limbs in utero)
Poor prognosis if early-onset (most is PPROM)
What is polyhydramnios?
Abnormally high level of amniotic fluid during pregnancy
Defined as amniotic fluid index >95th centile for the gestational age, or deepest pool >8cm
What are the main causes of polyhydramnios?
Main causes of polyhydramnios are:
- Idiopathic (60%)
- Failure of foetal swallowing (oesophageal atresia, diaphragmatic hernia, neurological abnormalities, muscular dystrophies)
- Duodenal atresia
- Foetal polyuria (maternal DM)
- Hydrops foetalis
- Congenital infections
- Chromosomal abnormalities
- TTTS (oligohydramnios in one twin; polyhydramnios in the other)
What is the epidemiology of polyhydramnios
1% of all pregnancies; much more common in DM/GDM
What are the signs and symptoms of polyhydramnios
Symptoms of underlying cause (e.g. DM)
- Maternal discomfort, breathlessness
- On examination:
- Abdo: increased SFH, impalpable foetal parts, tense abdomen
What are the Ix for ?polyhydramnios
-
USS
- For diagnosis
- AFI (>25 indicates polyhydramnios) and maximum pool depth
- Assess foetal size
- Look for structural abnormalities
- For diagnosis
- Other Ix for cause: OGTT (DM), Doppler and Rhesus Ix (foetal anaemia), karyotyping, TORCH screen etc.
What is the Mx of polyhydramnios
Depends on underlying cause → treat cause
- Usually no treatment is needed
Amnioreduction:
- Performed if severe maternal symptoms (e.g. breathlessness)
- Risk of infection and placental abruption (due to sudden release of intrauterine pressure)
Indomethacin (NSAID):
- Enhances water retention → reduces foetal urine output
- Don’t use beyond 32wks (risk of premature closure of ductus arteriosus)
In idiopathic: neonatologist examine before first feed (NG tube passed) to ensure no TOF/oesophageal atresia)
What are the complications and prognosis of polyhydramnios
Complications:
- Complications related to cause
- Malpresentation (foetus has more space to move within uterine cavity)
- Preterm labour (due to over-distension of uterus)
- Cord prolapse
- Placental abruption
- PPH (as uterus has to contract further)
Good prognosis → most is idiopathic and no congenital abnormality
Severe idiopathic polyhydramnios is associated with increased perinatal mortality (due to preterm labour and likely congenital malformation)
What is an amniotic fluid embolism?
Obstetric emergency in which amniotic fluid enters the maternal circulation, causing cardiorespiratory collapse
What is the aetiology of an amniotic fluid embolism?
Aetiology is unclear → may be due to strong uterine contractions, excessive amniotic fluid and disruption of vessels supplying the uterus
- Entry of amniotic fluid or foetal debris into the maternal circulation provokes either an anaphylacticoid reaction or activation of the complement cascade
What are the RFs for an amniotic fluid embolism?
- multiple pregnancy,
- increasing maternal age,
- IOL,
- uterine hyperstimulation,
- uterine rupture,
- placenta praevia,
- placental abruption,
- polyhydramnios,
- trauma
What is the epidemiology of amniotic fluid embolism?
Rare → 2/100,000 pregnancies
What are the signs and symptoms of amniotic fluid embolism?
- Can occur at any time, but the vast majority occur in labour/puerperium
- Sudden onset dyspnoea
- Chest pain
- Collapse
- DIC (may be the first sign in some patients; almost all patients develop it within 4hrs)
- Foetal distress
-
On examination:
- Low BP, high RR, high HR, cyanosis
What are the Ix for ?amniotic fluid embolism?
- Ix are similar to those done in cardiac arrest and other emergency scenarios
- Bloods: FBC, U&E, cross match, clotting studies, ABG
- ECG → ischaemic changes
- CXR → pulmonary oedema
- Definitive diagnosis confirmed on post mortem
- Foetal squamous cells and debris in the pulmonary vasculature
What is the Mx of amniotic fluid embolism?
Largely supportive; manage in ICU
ABCDE, senior help
- A: maintain airway patency
- B: high-flow O2 +/- intubation
- C: 2 large-bore cannulae, fluid resuscitation, consider pulmonary artery catheter and ionotropic support, correct coagulopathy with blood products if necessary
Delivery
- Emergency C-section
- If cardiac arrest/severe maternal compromise: perimortem section (facilitate CPR of mother)
What are the complications and prognosis of amniotic fluid embolism?
Complications:
- Cardiac arrest
- DIC
- ARDS, renal failure
- Death
Very poor prognosis up to 40% mortality (most in 1st hour)
What is uterine rupture?
Full-thickness disruption of the uterine muscle and overlying serosa
- Incomplete: peritoneum overlying the uterus is intact uterine contents remain within the uterus
- Complete: peritoneum is also torn uterine contents can escape the peritoneal cavity
What are the RFs for uterine rupture?
- previous C-section (esp midline incisions),
- previous uterine surgery,
- induction/augmentation of labour,
- obstruction in labour,
- multiparity
Epidemiology of uterine rupture?
- Uncommon → 2/10,000 pregnancies in UK overall;
- 10x more common in VBAC
What is the main prevention method to prevent uterine rupture?
- reducing rates of primary C-section
- being cautious in VBAC
Symptoms of uterine rupture?
- Severe abdo pain which persists between contractions
- Shoulder-tip pain (from diaphragmatic irritation),
- Vaginal bleeding
What is seen O/E in uterine rupture?
- Signs of hypovolaemic shock if significant haemorrhage (tachycardia, HTN, slow cap refill)
O/E
- Regression of the presenting part
- Abdo palpation may reveal scar tenderness and palpable foetal parts (if foetus is extruded from uterus)
- Signs of foetal distress
Ix for uterine rupture?
- Continuous CTG for all women at risk of uterine rupture
- Foetal distress is an early indicator
- Sometimes abnormal CTG prompts C-section, and uterine rupture is noted intra-operatively
- USS if suspicion of uterine rupture before labour (rare)
Mx of uterine rupture?
-
ABCDE, senior help
- A: Maintain airway patency
- B: 15L 100% O2 through non-rebreathe mask
- C: Assess circulatory compromise (cap refill, HR, BP, ECG)
- Insert 2 large bore cannulae
- Circulatory resuscitation cross-matched blood when available (O-ve/crystalloids/colloids before)
- D: Monitor GCS
- E: Expose patient to identify other bleeding sources
-
Urgent laparotomy and emergency C-section
- Uterus either repaired or removed
Prognosis of uterine rupture?
High maternal and foetal morbidity and mortality
What is cord prolapse?
The umbilical cord descends through the cervix, with (or before) the presenting part of the foetus
What are the types of cord prolapse?
- Occult (incomplete): cord descends alongside the presenting part, but not beyond it
- Overt (complete): cord descends past the presenting part and is lower than the presenting part in the pelvis
- Cord presentation: presence of the cord between the presenting part and the cervix
Aetiology of cord prolapse?
Occult or overt occurs when membranes have ruptured; cord presentation may occur with intact membranes
Foetal hypoxia occurs via 2 main mechanisms:
- Occlusion: presenting part presses onto the umbilical cord, occluding blood flow to the foetus
- Arterial vasospasm: exposure of the umbilical cord to the cold atmosphere results in umbilical arterial vasospasm, reducing blood flow to the foetus
RFs for cord prolapse?
- breech presentation (esp footling),
- abnormal/unstable lie,
- artificial rupture of membranes (esp when presenting part is high in the pelvis),
- polyhydramnios,
- prematurity
Signs and symptoms of cord prolapse?
- Consider in the presence of a non-reassuring foetal HR pattern and absent membranes
- Bradycardia is strongly associated
- Confirm by external inspection or on VE
Ix for cord prolapse?
- Clinical diagnosis
- CTG
Mx of cord prolapse?
- Senior help
- Avoid handling the cord to reduce vasospasm
- Manually elevate the presenting part (lift off cord) by VE
- Move patient into left lateral position with head down and pillow under hip, or knee-chest position → relieves pressure on cord from the presenting part
- Emergency C-section; vaginal/instrumental if fully dilated and delivery is imminent
Complications and prognosis of cord prolapse?
Mortality rate for neonate is high (91/1000)
- Largely because cord prolapse occurs more frequently in preterm babies, who are often breech, and may have other congenital abnormalities
What is shoulder dystocia?
After delivery of the head, the anterior shoulder of the foetus becomes impacted on the maternal pubic symphysis, or (less commonly) the posterior shoulder becomes impacted on the sacral promontory
Aetiology of shoulder dystocia?
Delay in delivery of the foetal shoulders leads to foetal hypoxia
- Applying traction to the foetal head can result in foetal brachial plexus injury
RFs for shoulder dystocia?
previous shoulder dystocia,
macrosomia,
DM,
maternal obesity,
IOL/augmentation,
prolonged labour,
secondary arrest,
instrumental delivery
Epidemiology of shoulder dystocia?
0.6% of all deliveries
Signs and symptoms of shoulder dystocia?
- Delay delivery of the shoulders following the head with the next contraction
- Failure of restitution: foetal head remains in OA position following extension (doesn’t turn to look at side)
- Turtle neck sign: foetal head retracts slightly back into pelvis, so neck is no longer visible
Ix for shoulder dystocia?
- Clinical diagnosis
- CTG
Mx for shoulder dystocia?
Immediate steps:
- Senior help
- Advice mother to stop pushing if possible (can worsen impaction)
- Make woman lie flat
- Avoid downwards traction on the foetal head (increases risk of brachial plexus injury)
- Consider episiotomy (makes access for manoeuvres easier)
1st line manoeuvres:
- McRoberts procedure: hyperflex maternal hips (knees to shoulders) to widen pelvic outlet
- 90% success rate
- Suprapubic pressure: sustained or rocking pressure behind anterior shoulder to release it
2nd line (internal) manoeuvres:
- Posterior arm: insert hand posteriorly into sacral hollow and grasp posterior arm to deliver
- Internal rotation (corkscrew/Woods screw manoeuvre): apply pressure simultaneously in front of one shoulder and behind the other to move the baby 180⁰
- If all the above fails move patient onto all 4s and repeat (may widen pelvic outlet)
If this fails:
- Zavenelli manoeuvre: push foetal head back into pelvis for C-section
Post-delivery:
- Active management of 3rd stage of labour (increased risk PPH)
- PR exam to exclude 3rd degree tear; consider physio review (risk of pelvic floor weakness, nerve damage)
- Paediatric review assess for brachial plexus injury, humeral fracture, hypoxic brain injury
- Debrief mother and partner, advise of risk of recurrence
Complications of shoulder dystocia?
- Maternal:
- 3rd/4th degree tears,
- PPH,
- psychological trauma
- Foetal:
- brachial plexus injury (Erb’s palsy),
- hypoxic brain injury,
- humerus or clavicle fracture
What is PPH? What are the types of PPH?
Primary PPH: loss of >500ml of blood per vagina within 24hrs of delivery (>1000mL following C-section)
- Minor PPH: 500-1000ml blood loss
- Major PPH: >1000ml blood loss
Secondary PPH: excessive vaginal bleeding in the period from 24hrs after delivery to 6 weeks postpartum
Causes of primary PPH?
Remember the 4Ts: tone, tissue, trauma, thrombin
-
Tone (uterine atony):
- Most common cause
- Uterus fails to contract adequately following delivery, due to lack of tone in uterine muscle
- RFs: age >40, BMI >35, previous PPH
- Uterine overdistension: multiple pregnancy, polyhydramnios, macrosomia
- Uterine muscle exhaustion: prolonged/rapid labour, grand multiparity, oxytocin use
- Uterine distortion: fibroids, placenta praevia, placental abruption
- Intra-amniotic infection: fever, PROM
-
Tissue:
- Retained placental products (membranes, cotyledon, succenturiate lobe)
- Retained blood clots in an atonic uterus
- Gestational trophoblastic disease
- Abnormal placentation
-
Trauma:
- Damage sustained to reproductive tract during delivery (vaginal/cervical tears, uterine rupture)
- RFs: instrumental deliveries, episiotomy, C-section
-
Thrombin:
- Coagulopathies and vascular abnormalities which increase the risk of PPH
- Vascular: placental abruption, HTN, pre-eclampsia
- Coagulopathies: VWD, haemophilia, ITP, DIC, HELLP
What are the causes of secondary PPH?
- Uterine infection (endometritis)
- Retained placental fragments or tissue
- Abnormal involution of the placental site (inadequate closure or sloughing of the spiral arteries at the placental attachment site)
Epidemiology of PPH?
5% of deliveries
Signs and symptoms of primary PPH?
- Vaginal bleeding (often severe)
- Dizziness, palpitations, SOB if severe
- On examination:
- General: tachypnoea, prolonged cap refill, tachycardia, low BP, pallor
- Abdo: may show atonic uterus (above umbilicus), ?signs of uterine rupture
- Speculum: assess for sites of local trauma causing bleeding
- Vaginal: evacuate clots from cervix (inhibits contraction)
- Examine placenta to ensure it is complete
Signs and symptoms of secondary PPH?
- Vaginal bleeding (usually less severe than primary PPH)
- Spotting with occasional gush of fresh blood; 10% present with massive haemorrhage
- Symptoms of cause, e.g. endometritis may present with fever, lower abdo pain, foul smelling lochia
- On examination:
- Lower abdo tenderness (endometritis)
- Uterus may still be high (sign of retained placenta)
- Speculum exam to assess amount of bleeding; do high vaginal swab at the same time
Ix for PPH?
- Basic obs
- FBC
- Cross match 4-6 units blood
- Coagulation profile
- U&Es
- LFTs
- Blood cultures (if pyrexial)
- USS can show retained placental tissue
Mx of primary PPH?
-
Prevention:
- Active management of 3rd stage of labour reduces risk by 60%
- IM oxytocin (10 units in vaginal delivery; 5 units in C-section)
- Active management of 3rd stage of labour reduces risk by 60%
-
Immediate management:
- ABCDE, get senior help
- A: Maintain airway patency
- B: 15L 100% O2 via non-rebreathe mask
- C: Assess circulatory compromise, insert 2 large bore cannulas as take blood samples, give cross matched blood/O -ve blood (until then give warmed crystalloid and colloid)
- D: Monitor GCS
- E: Expose patient to identify bleeding sources
-
Uterine massage
- Bimanual compression to stimulate uterine contraction
- Insert gloved hand into vagina and form a fist inside the anterior fornix to compress the anterior uterine wall; other hand applies pressure to abdo at posterior aspect of uterus
-
Give drugs to increase myometrial contraction
- Syntocinon, ergometrine (contraindicated in HTN), tranexamic acid, misoprostol
- Transfer to theatre
- ABCDE, get senior help
-
Definitive management (depends on underlying cause):
- Uterine atony: intrauterine balloon tamponade, haemostatic suture around uterus, uterine artery ligation, hysterectomy (last resort)
- Trauma: repair laceration, hysterectomy (last resort in uterine rupture)
- Tissue: removal of placenta/retained products
- Thrombin: correct clotting abnormalities with blood products
- IV antibiotics
Mx of secondary PPH?
- Antibiotics (usually ampicillin and metronidazole) for endometritis and retained tissue
- Uterotonics (syntocinon, ergometrine, misoprostol)
- Surgical measures if excessive or continuing bleeding (see above)
- Massive secondary PPH resuscitation (as described above)
Complications and prognosis of PPH?
Complications:
- Death (a leading cause of maternal mortality)
- Hysterectomy
- VTE
- Renal failure
- Sheehan’s syndrome (pituitary hypoperfusion causing pituitary necrosis and hypopituitarism)
25% recurrence rate
RFs for shoulder dystocia?
previous shoulder dystocia,
macrosomia,
DM,
maternal obesity,
IOL/augmentation,
prolonged labour,
secondary arrest,
instrumental delivery
What is the Mx of VTE in pregnancy?
Prophylaxis:
- All women risk assessed in early pregnancy, then repeated in intrapartum and postnatal periods
- All women: advised to avoid dehydration, mobilisation
- If LMWH is contra-indicated: compression stockings
Treatment:
- Massive PE:
- ABCDE, senior help
- IV unfractionated heparin; rarely may need thrombolysis
- Haemodynamically stable:
- SC LMWH (enoxaparin)
- Given on clinical suspicion (before diagnosis confirmed)
- If confirmed VTE:
- Continue LMWH until 6wks postpartum; can convert to warfarin 3wks after delivery
- Discontinue at start of labour or 24hrs before planned delivery
- NB NOACs are not licenced in pregnancy; warfarin is teratogenic
- SC LMWH (enoxaparin)


