FunMed Pulmonary Flashcards
Adult ICU CAP treatment
- ICU: B-lactam + macrolide OR B-lactam + fluoroquinolone
- broaden antibiotics with Pseudomonas coverage, i.e., B-lactam
- Consider further testing if not improving (eg CT of chest); thoracentesis if pleural fluid is present
- Outpatient: macrolide +/- B-lactam; doxycycline
- Inpatient: B-lactam + macrolide OR a respiratory fluoroquinolone
- Supportive care
- Limit the number of paroxysms
- Observe the severity of cough and provide assistance when necessary; Elevate head
- Maximize nutrition, rest, and recovery
- Azithromycin is the treatment of choice for all patients.
- Trimethoprim-sulfamethoxazole if a hypersensitivity to macrolides
- Prophylaxis for exposed/susceptible persons is also azithromycin for 5 days

Treatment of Pertussis
- paramyxovirus
- annual outbreaks, winter, mid-October - January
- A leading cause of hospitalization in US children
- Can also cause upper and lower respiratory tract infection in adults
- increasingly recognized severity in those with comorbid conditions
Respiratory Syncytial Virus (RSV)
Use these for diagnosis of what?
- Radiographically presents with nodular, irregular, pleural thickening, poss pleural effusion, and pleural plaquing
- CXR
- CT
- Thoracentesis
- Surgical biopsy
- Usually necessary for diagnosis
- Difficult to diagnose
- PET
- Helpful in ?malignancy; staging; poss surgical candidate
Mesothelioma
•2-5mm radio-opaque nodules on CXR
Dust particles in the alveoli are ingested by macrophages which then become “coal macules”
- HIV testing
- Interferon-gamma release assay (IGRA)
- Acid-fast bacilli (AFB) smear and culture with drug susceptibility
Using sputum from the patient collected in the early morning on how many consecutive days?
Diagnostic Tests for TB
3 consecutive days

- Complications include
- Respiratory failure for a minority of patients
- Malignancy
- Bronchogenic adenocarcinoma
- Malignant Mesothelioma (cancer arising from the mesothelial surface of the pleural cavity)
- Concomitant tobacco use increases risk of malignancy even more
- Treatment is supportive and preventative
Pneumoconiosis – Asbestosis
PCR assay is faster and more sensitive, but Nasopharyngeal swab is criterion standard for diagnosis
CBC will show leukocytosis with absolute lymphocytosis
Positive tests must be reported to state and local public health authorities
Diagnosis of Pertussis
•Alveolar ventilation (⩒A) ultimately determines the
PaCO2
- Recurrent, alveolar hemorrhage
- Children or young adults
- Iron deficiency
- Celiac disease.
- Treatment of acute episodes of hemorrhage with corticosteroids. Recurrent episodes of pulmonary hemorrhage may result in interstitial fibrosis and pulmonary failure.
Alveolar Hemorrhage Syndrome: Idiopathic pulmonary hemosiderosis:
Renal involvement and anti-glomerular basement membrane antibodies are absent, in contrast to Goodpasture Syndrome
- Symptoms last 5-7 days
- Edema and obstruction of these upper airways.
- Viral infection of the larynx, trachea, and the upper bronchial tree
- Most common between 7 and 36 months of age
- Lungs are typically clear to auscultation
Acute Laryngotracheitis / Croup

- Slowly progressive constitutional symptoms
- Malaise
- Anorexia
- Weight loss
- Fever
- Night sweats
- Chronic cough, productive with blood streaked sputum
Presentation of TB
- Patients typically present decades after relevant exposure with:
- Wait for it…
- Slowly progressive dyspnea, dry cough, and inspiratory crackles on exam…
Restrictive Lung Diseases Interstitial Lung Disease/Diffuse Parenchymal Lung Disease
Occupational Lung Diseases
Pneumoconiosis – Asbestosis
Pediatric Pneumonia, drug of choice for each age group?
- <4 weeks:
- 4-12 weeks:
- 3mo-5 yrs:
- >5yrs:
- <4 weeks: ampicillin and gentamicin or cefotaxime
- 4-12 weeks: IV ampicillin
- 3mo-5yrs: oral amoxicillin (if outpatient)
- >5 yrs: oral amoxicillin +/- a macrolide if an atypical organism is likely
Virchow triad?
(1) venous stasis
(2) activation of blood coagulation
(3) vein damage

- 2-5mm radio-opaque nodules on CXR
- Nodular opacities occur primarily in the upper lung fields in simple version
- May become more widespread and then confluent with progression to large opacities in complicated version with progressive massive fibrosis
Pneumoconiosis – Coal Worker’s Lung
simple coal workers pneumoconiosis
complicated coal workers pneumoconiosis
Which Alveolar Hemorrhage Syndrome?
- Idiopathic, recurrent alveolar hemorrhage
- Glomerulonephritis - rapidly progressive
- Occurs in men 30-40 yo
- Hemoptysis usual presenting symptom
- Dyspnea, cough, hypoxemia, diffuse bilateral alveolar infiltrates
- Iron deficiency anemia and microscopic hematuria (glomerulonephritis)
Goodpasture syndrome
- Abrupt onset (w/in 4-6 hrs) of fever, chills, malaise, nausea, cough, chest tightness, dyspnea.
- Exam: basilar crackles and tachypnea.
- CXR frequently normal
- Potentially confused with a viral or bacterial infection and given antibiotics
- Treatment: remove from environment
- Symptoms subside within 12hrs to several days.
Disease may recur with reexposure
ACUTE Hypersensitivity Pneumonitis
- Transmitted via respiratory droplets
- Attacks ciliated epithelium
- Produces toxins —> inflammation and necrosis —> airway plugs, bronchopneumonia, and hypoxemia.
Pertussis
- Nasopharyngeal swab for culture is the Criterion standard for diagnosis but Takes a long time to get results and Must be cultured during catarrhal or paroxysmal phases
- PCR assays and antigen detection has Rapid results and More sensitivity and Can use later in the disease course
- CBC will show leukocytosis with absolute lymphocytosis
- Positive tests must be reported to state and local public health authorities
Diagnosis of Pertussis
- Since cause is most often viral, antibiotics not necessary.
- Avoid cough suppressants (try not to mess with the mucociliary clearance!)
- Okay to use at night if patient needs sleep
Treatment of Acute Bronchitis
Adult CAP Treatment
•Always cover _______?
Generally cover________?
- Outpatient:
- Inpatient:
- ICU:
S. pneumoniae
Atypicals
macrolide +/- B-lactam OR doxycycline
B-lactam + macrolide OR a respiratory fluoroquinolone
B-lactam + macrolide OR B-lactam + fluoroquinolone
- Most cases caused by RSV
- Edema and cellular debris cause obstruction of small airways.
- most often in infants and young children.
- Most commonly in first 2 years of life.
- Peak age is 6 months.
- Leading cause of infant hospitalization.

Acute Bronchiolitis
OSA: treatment (children)
●Much more likely to be treated surgically
○Good outcomes data in otherwise healthy children with adenotonsillar hypertrophy
●Other surgeries can be done for children with craniofacial abnormalities; case-by-case evaluation
●CPAP if no surgical option, especially in obese children
○Need frequent re-evaluation of mask fit
●Other lifestyle interventions
○Healthy diet, exercise, weight management
○Management of allergy/nasal congestion if present
○Orthodontia if needed otherwise
Adult CAP: diagnostic testing:
- CBC with differential and chemistries to?
- WBC differential can (sometimes) assist with differentiating?
- Must be true sputum rather than saliva. Criteria per high powered field?
- Blood cultures for high-risk patients or those suspected of?
- Nasopharyngeal swab for?
- Urine antigen testing for?
- Help assess the severity of illness
- Viral from bacterial etiology
- >25 WBCs and <10 squamous epithelial cells per HPF
- Sepsis
- PCR looking for viral infection and some atypicals
- Legionella and S. pneumoniae.
no current or recent hospitalization or stay in a long-term care facility
no antibiotic therapy in the past 3 months
not on chronic dialysis or home infusion therapy
no home wound care
no household contact with a multi-drug resistant organism
community-acquired pneumonia
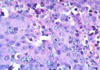
- Identification of _________ and ferruginous bodies on pathology aid diagnosis (though usually unnecessary)
- Respiratory failure for a minority of patients
- Bronchogenic adenocarcinoma
- Malignant _________?
Concomitant tobacco use increases risk of malignancy even more
asbestos fibers
Pneumoconiosis – Asbestosis
Mesothelioma
(cancer arising from the mesothelial surface of the pleural cavity)

An Immunologic reaction to an inhaled organic antigen
Hypersensitivity Pneumonitis
- Reticular and small nodular opacities bilaterally in the lower lung fields
- Calcified pleural plaques, also typically in the lower lungs
- Pleural effusions

Pneumoconiosis – Asbestosis

- Most patients recover in 3 days
- Malaise may persist for weeks
Rapid Diagnostic Testing takes about 15 minutes for results.
RT-PCR assay testing can take 4 to 8 hours; Some tests can differentiate between A&B, some can specify the strain of A; complex lab test and $$$
Viral Culture takes 10-14 days.
Influenza
- Chronic
- Simple version:
- Appears as innumerable, small, rounded opacities (<10mm) in the dorsal, upper lung fields.
- HRCT is helpful in evaluation
Pneumoconiosis – Silicosis
- It is VERY important to establish clearing of?
- A common presentation of lung tumor is post-obstructive?
- A follow-up CXR should always be done in ______ to document return to normalcy
- After hospitalization, follow up within ______ prevents re-admission
pneumonia
pneumonia
6-8 weeks
5 days
Dyspnea- tachypnea- chest pain may be your only clues for?
PE
A normal A-a gradient is less than?
Patient’s age divided by 4 + 4
- Characteristic linear IgG deposits detected by immunofluorescence in glomeruli or alveoli is diagnostic
- Combinations of immunosuppressive drugs and plasmapheresis work well for treatment
Diagnosis and treatment for the Alveolar Hemorrhage Syndrome, Goodpasture syndrome
What disease?

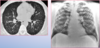
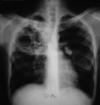
A representative anteroposterior chest x-ray in the exudative phase of ARDS
•Pressure-volume relationship in the lungs of a patient with acute respiratory distress syndrome (ARDS)

- Low grade malignant neoplasms
- Most common in GI tract
- Well-differentiated neuroendocrine tumors
- Central vs. peripheral pulmonary
Carcinoid/Bronchial gland tumors, aka: bronchial adenomas
★A leading cause of hospitalization in young children
★Nasopharyngeal swab for RSV rapid viral antigen test
★Treat with oxygenation, hydration, bronchodilators, suctioning
★Bronchiolitis/RSV
A chronic, immunologically mediated, granulomatous disease

•Inhalation causes lung pathology. However, skin contact can cause cutaneous nodules as well
Pneumoconiosis – Berylliosis
- Occurs most commonly in children <2 or 9 - 15 yrs
- Cough may or may not be productive
Labs and Chest X-ray are usually not necessary unless patient appears to be more acutely ill or fever is very high.
Physical Exam shows:
- Wheezing
- Rhonchi
- Fever
Acute Bronchitis
- Symptoms: Gradual/insidious onset of: productive cough, dyspnea, fatigue, anorexia and weight loss.
- Exam: tachypnea, diffuse crackles.
- PFTs: restrictive, decreased DLCO.
- CXR: normal to micronodular or reticular opacities.
- HRCT: diffuse micronodules
- BAL: marked lymphocytosis
- Tissue pathology: noncaseating granulomas
- Treatment: remove exposure. glucocorticoids may be required. Improvement in symptoms and function takes longer than with acute HP, weeks to months.
SUBACUTE Hypersensitivity Pneumonitis
•CURB-65:
for what?
- Confusion
- Urea (BUN) >19
- Respiratory rate >30
- Blood pressure: systolic <90, diastolic <60
- 65 years of age or older
Adult CAP
The most common cause of death from ARDS is?
severe irreversible hypoxemia accounts for only?
multi-organ failure secondary to sepsis
9% to 19% of deaths
- Typical lesion is a granuloma with central caseation necrosis.
- Bacilli proliferate locally and spread through the lymphatics to a hilar node, forming the Ghon complex.
Pathophysiology of TB
Symptoms: URI symptoms, Wheezing, Cough, Dyspnea, Irritability, Poor feeding, Low grade fever, Apnea
Exam Findings
Tachypnea (can be up to 60-80 breaths per minute!), Nasal flaring, Use of accessory muscles for respiration, Diffuse wheezing
•Fine rales, Tachycardia, Fever (but not always), Hypoxia
Presentation of Bronchiolitis
Carcinoid Syndrome
Rare (<10%)
Name four Symptoms?
- Flushing
- Diarrhea
- Wheezing Bronchospasm
- Hypotension
Avoid triggers
Treat allergic rhinitis causing PND, treat GERD
QUIT SMOKING!!!!!!!!!
Allergy Desensitization if indicated
Vaccination: Pneumococcal and influenza
Asthma - prevention/treatment
★Supportive care, cool mist humidifier, bronchodilators as needed
★Antibiotics are NOT needed! This is most likely a viral infection
★Most common in the first 2 years of life
★Bronchiolitis/RSV
Pediatric pneumonia
•Transmitted upper airway noise is difficult to differentiate from lower respiratory abnormalities
•Listen to the chest, then hold your stethoscope up to the cheek
The mechanisms of lung parenchyma damage and role of airway changes following smoke inhalation injury. This is looking at what happens when thermal injury and chemical injury occur.

Cast formation!

Names of the three types of Mesothelioma?
1st. Most common, >50%?
2nd. Worst prognosis and resistant?
3rd. ?
All progress rapidly and are painful.
1st. Epithelial
2nd. Sarcomatoid
3rd. Biphasic


What type of Non-Squamous Cell Carcinoma?
- Can grow anywhere in the lungs, ie.e, central or peripheral
- Is heterogeneous, i.e., undifferentiated
- Rapid doubling time
- Metastasize early
Large Cell
- Prognosis:
- Course is variable and if disease responds to glucocorticoids then may live with it chronically.
- If fail glucocorticoids then may try Methotrexate or other immunosuppressive agents but no clear evidence showing efficacy
- Some patients experience progressive deterioration of lung function and development of pulmonary fibrosis
- No increased risk of cancer
Pneumoconiosis – Berylliosis
the minimum age for flu vaccine?
6 months
Xray shows normal or hyper-inflation
More done to rule out pneumonia or
Other complications
Chest x-ray in Asthma
★A self-limiting cough lasting more than 5 days and up to 3-4 weeks
★Most commonly caused by a virus (Rhinovirus, adenovirus,…)
★Occurs most frequently in children
★Virus disrupts the mucociliary clearance in the airways
★Causes cough and wheezing
★Supportive care, cool mist humidifier, bronchodilators as needed
★Antibiotics are NOT needed! This is most likely a viral infection
★Acute Bronchitis Pearls
•reticular opacities are more often in the middle and upper lung fields as opposed to the bases. Also see hilar adenopathy.
Sarcoidosis
Pleurodesis (though rare)
to seal lung to pleura using talc
○OSA is diagnosed when
there are 5 events (apnea, hypopnea, desaturation) per hour in a patient with typical symptoms; or 15 events per hour regardless of symptoms
Presentation of Mesothelioma
Bi or unilateral?
chest pain pleuritic or non-pleuritic?
usually present with?
Unilateral - 60% right sided, 5% bilateral
Non-pleuritic chest pain
pleural effusion
Tracheobronchomalacia- uncommon disease of the central airways resulting from softening or damage of the cartilaginous structures of the airway
Tracheal Stenosis - narrowing of the trachea
Chronic cough
GERD
DD for Asthama
Complication of Influenza?
- Associated with aspirin use in the management of viral infections
- Occurs in young children
- Consists of rapidly progressive hepatic failure and encephalopathy
- 30% mortality rate.
Reye syndrome
- What disease?
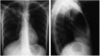
CXR usually diagnostic with these common patterns:
- Patchy…?
- Lobar…?
- Diffuse…?
- Pleural…?
- Patterns can be suggestive of but not…?

- Adult CAP
- patchy airspace opacities
- lobar consolidation with air bronchograms
- diffuse alveolar or interstitial opacities
- pleural effusion
- diagnostic for specific etiologies

fever, fatigue and productive cough between 5 days and 3-4 weeks
- 90% viral
- inflammation of trachea, bronchi, and bronchioles.
- self-limiting
Acute Bronchitis
Prevention of what disease?
- DTaP vaccine: Recommended at the ages of ________ and __ - __ months and at age __ - __ years; it is not recommended for children aged 7 years or older
- Tdap vaccine: Recommended for children aged __ -__ years who are not fully vaccinated; as a single dose for adolescents 11-18 years of age; for any adult 19 years of age or older; and for pregnant woman regardless of vaccination history, including repeat vaccinations in subsequent pregnancies

Prevention of Pertussis
2, 4, 6, and 15-18 months
4-6 years
7-10
A multisystem granulomatous disorder of unknown etiology
Sarcoidosis
These are risks for?
- Age <3 months
- Low birth weight
- Gestational age of <29 weeks
- Low socioeconomic group
- Crowded living conditions
- Parental smoking
- Chronic lung diseases
- Neurologic diseases
- Congenital Heart disease with pulmonary hypertension
- Immunodeficiencies
- Airway anomalies
Acute Bronchiolitis

Adult Inpatient CAP
•Inpatients can be converted to oral antibiotics when:
1.
2.
3.
- Hemodynamically stable
- Able to ingest and absorb oral medications
- Clinically improving
Respiratory Failure
- Type I =
- Type II =
- Type III =
- Type IV =
hypoxemia
hypercapnia
Perioperative (atelectasis)
Shock (Hypoperfusion)
recurrent episodes of apnea lasting at least 10 seconds, associated with oxygen desaturation in the blood; or hypopnea, defined as decreased airflow and drop in saturation of at least 4%
Obstructive sleep apnea: definition
A 6-month-old boy presents to the ER with his parents with acute onset of rhinorrhea, cough, and wheezing. The symptoms have quickly progressed and the patient now has dyspnea and irritability. The mother states that her child was born at 34 weeks gestation with a small patent foramen ovale that they are hoping will close with age. On examination, the child’s temperature is 38oC or 100.4oF. There are rhonchi heard in all lung lobes. His respiratory rate is 50 breaths per minute, and he exhibits flaring of nares and use of accessory muscles of respiration resulting in intercostal and supraclavicular retractions. Widespread fine rales are heard at the end of inspiration and in early expiration. The expiratory phase is prolonged and wheezing is audible throughout the lung fields.
What is the most likely diagnosis?
What test or tests should be performed? Chest X-ray (?),
Treatment in this child will include what?
Is there a vaccine that this child missed?
Would this child have qualified for Synagis?
Acute Bronchiolitis
RSV rapid viral antigen nasal swab
Hospitalization, Humidified oxygen, nebulized bronchodilators, nebulized ribavirin, IV hydration, nasopharyngeal suctioning.
No vaccine for RSV.
Yes, premature and small congenital heart defect. Should have been started on Synagis at the beginning of the RSV season.
Adult CAP Treatment
- Traditional duration of treatment is ________, but when using a respiratory fluoroquinolone________ is sufficient IF uncomplicated
- Patient should be improving and afebrile ________ to stop ABx
10-14 days
5 days
48-72 h
- May have Fatigue, Malaise, Fever or Weight Loss
- Skin lesions
- Cervical Lymphadenopathy
- Visual changes, dry eyes
- Dry mouth, parotid swelling
- Palpitations, syncope
- Joint pain or swelling
- Muscle weakness
- Hepatomegaly and tenderness
Sarcoidosis: Extrapulmonary findings
Symptoms include: Malaise, Fever, Night Sweats, Weight loss, Productive cough, Blood-streaked sputum;
Exam: Cervical lymphadenopathy and apical rales.
Tuberculosis
★Virus disrupts the mucociliary clearance in the airways.
What disease?
★Acute Bronchitis Pearls
Airway Edema + Accumulation of cellular debris in small airways —-> obstruction —-> V/Q mismatch = wasted perfusion, a right-to-left shunt, and hypoxemia early in the course of the disease
Pathophysiology of Acute Bronchiolitis


Sarcoidosis
Chronic, immunologically mediated, granulomatous disease
Pneumoconiosis – Berylliosis
REMEMBER IT THIS WAY:
Eosinophils, think
Granuloma, think
Angiitis, think
asthma
nodules in lungs
vasculitis of arteries
- pO2 < 60 mmHg and/or
- pCO2 > 50 mmHg
Respiratory Failure
Pleural effusion
- Transudative =
- Exudative =
- If moderate or greater, should be_________?
(clear) fluid is an inflammatory reaction
(purulent) fluid = empyema
tapped and evaluated
moderate to severe acute exacerbation of COPD
2 or more of the following get what?
increased sputm, dyspnea or sputum purulence
ABs
- Symptoms:
- # 1 Weight loss/anorexia/asthenia
- # 2 A cough
- Dyspnea
- Chest pain
- Symptoms more likely if prior COPD dx
- Exam:
- Lymphadenopathy
- Hepatomegaly
- Clubbing fingers
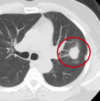
NSCLC
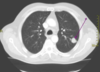
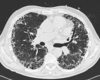
CT of Non-Small Cell Squamous Cell Carcinoma
Pathologic condition in which alveoli are perfused with blood, but not ventilated.
Pulmonary Shunting
ECG is typically normal except in advanced disease, where right ventricular hypertrophy (right axis deviation, incomplete right bundle branch block) and right atrial enlargement (peaked P wave in the inferior and right-sided leads)
Pulmonary Hypertension
People with AIDS are 20-40 times more likely than immunocompetent persons to develop
- HIV infection
- Intravenous drug abuse
- Incareration
- Household contacts with TB
- Homelessness/Shelter living
- Travel to an endemic area
- Alcoholism
- Diabetes mellitus
- Silicosis
- Immunosuppressive therapy
- Tumor necrosis factor–alpha antagonists
- Cancer of the head and neck
- Hematologic malignancies
- End-stage renal disease
- Intestinal bypass surgery or gastrectomy
- Chronic malabsorption syndromes
- Low body weight
- Smoking - Smokers who develop TB should be encouraged to stop smoking to decrease the risk of relapse
- Age below 5 years
Risk Factors for TB
TB is the leading cause of death in HIV positive people.
This treatment for which neoplastic lung disease?
- Surgery (Only Stage I), Mediastinal Staging always indicated preop, Always followed by chemo
- Smoking Cessation
- Systemic Chemotherapy +/- radiation
- Good initial response but often recurrence
- Pain management
- Palliative care referral usually indicated
Small Cell
Inpatient treatment:
- Oxygen
- Racemic epinephrine via NEB
- Corticosteroids
- Intubation/ventilation
Most patients can be treated at home:
- Cool, humidified air
- Corticosteroids
- Single dose dexamethasone
- Single dose racemic epi
Treatment for Croup
Exam Findings
- Fever
- Tachycardia
- Flushed face
- Conjunctival erythema
- Pharyngeal injection
Influenza
Board buzz words for?
Egophony
Pleural friction rub
Dullness to percussion
Other symptoms to expect?
pleural effusion
- Dyspnea
- Cough
- Chest pain
- Absent or diminished breath sounds over the effusion
- Bronchial breath sounds
- Tracheal shift (large effusion)
Nebulized Ribavirin
= a broad-spectrum antiviral agent used in severe cases of RSV
●High cost
Lack of demonstrated benefit in decreasing hospitalization or mortality

- Imaging:
- CXR:
- Basilar predominance of Reticular opacities indicative of Idiopathic Pulmonary Fibrosis
Most patients can be treated at home:
- Cool, humidified air
- Corticosteroids
- Single dose dexamethasone IM
- Single dose of racemic epinephrine
Treatment of Croup
- organisms are transmitted via respiratory droplets
- Attack ciliated epithelium in airways
- Produce toxins, resulting in inflammation and necrosis of the walls of small airways
- Leads to plugging of airways, bronchopneumonia, and hypoxemia.
Pathogenesis and Presentation of Pertussis
- Primary tumor arising from the pleural lining of lung or thorax
- can be either parietal or visceral
- 75% are diffuse/malignant
- Men:Women ratio?
- 60-80% have h/o?
20 - 40 year?
Is tobacco a risk?
Mesothelioma
3:1 ratio
h/o Asbestos exposure
latent period
no
- Imaging on CXR is more variable than the other disorders but does tend more to the upper lung fields. Can appear as nodular, ground glass, or linear opacities
- Hilar and mediastinal lymph node enlargement is common
Pneumoconiosis – Berylliosis
most common and quintessential histologic form of Idiopathic Pulmonary Fibrosis
Usual Interstitial Pneumonia
- Epidemiology:
- Men>Women
- 55-60 yo
- Signs & Symptoms:
- Insidious onset dry, hacking cough and SOB
- Inspiratory crackles on exam
Functional Classification of Pulmonary Hypertension
Class I:
Class II:
Class III:
Class IV:
without limitation
slight limitation
marked limitation
inability to perform any physical activity
- CXR findings in Hyaline Membrane Disease
- Why do we care about this disease in the pre-term infant?
- Diffuse bilateral atelectasis, which has the appearance of “ground-glass”, patchy alveolar opacities, or “whiteout”, all representing diffuse confluent alveolar filling.
- Most common cause of respiratory distress in the preterm infant
●Most commonly used is the STOP-Bang mnemonic
○Do you Snore loudly (can be heard through closed doors?)
○Are you Tired, fatigued, or sleepy during the day?
○Has anyone Observed that you stop breathing during sleep?
○Do you have high blood Pressure?
○Body mass index over 35
○Age over 50
○Neck circumference >16” female, >17” male
○Gender = male?
●Scoring:
○0-2 = low risk, 3-4 = moderate risk, 5-8 = high risk
OSA: screening tools
- Latent - No active disease; cannot transmit the organism to others.
- Contained but not eradicated
- Viable organisms may lie dormant within granulomas for years.
- Reactivation of disease may occur if the host’s immune defenses become impaired.
Pathophysiology of TB
- Overall presentation is similar to Sarcoidosis…BUT!….
- There’s a specific test!
- Blood test, low sensitivity. High specificity. Repeat negative or borderline tests. Two negative tests is a ‘negative’
- Tissue pathology shows noncaseating granulomas
Berylliosis
•BeLPT - Beryllium Lymphocyte Proliferation Test
- Bed Rest
- Hydration
- Oxygenation
- Antipyretics/Analgesics
- Prescription antiviral drugs: Neuraminidase inhibitors, Oseltamivir (Tamiflu, oral), Zanamivir (Relenza, inhaled), Peramivir (Rapivab, IV)
- Must be administered within 24-48 hours of symptom onset.
Treatment of Influenza
- Palivizumab (Synagis) is available in the United States for prevention of
- Decreases hospitalization rates
- Decision to use this drug is based on:
- The age of the child at the onset of RSV season
- The child’s medical history
RSV disease in high-risk infants.
Surface proteins on Influenza A include (i.e., H1N1)
hemagglutinin and neuraminidase
These proteins are critical for virulence and are major targets for the neutralizing antibodies of acquired immunity to influenza. Used to identify Influenza A subtypes
The two types of Non-Squamous Cell Carcinoma?
- Adenocarcinoma
- Peripheral, i.e., starts in the cells that line the alveoli of the lungs
- Large cell carcinoma
- Central or peripheral, i.e., can grow anywhere in the lungs
Alteration in the structure and function of the right ventricle (RV) of the heart caused by pulmonary hypertension associated with diseases outside the heart.
Cor pulmonale (“pulmonary heart disease”)
- Imaging shows
- Reticular and small nodular opacities bilaterally in the lower lung fields
- Calcified pleural plaques, also typically in the lower lungs
- Pleural effusions

Pneumoconiosis – Asbestosis
Chest X-ray: may show hyperinflation with scattered consolidation or lobar consolidation from a secondary infection

Acute Bronchiolitis
- obstructive, asthma-like
- caused by inhalation of cotton fibers.
- chest tightness, cough, wheezing and dyspnea
- worse on Mondays or first day back
- May progress to chronic bronchitis/COPD.
Byssinosis
Empyema should always be drained by________to clear infection?
tube thoracostomy


Asthma Differential Diagnosis: Vocal fold dysfunction syndrome
- adduction of the true vocal cords on inspiration and abduction on expiration
- causes inspiratory airway obstruction and stridor that is often mistaken for asthma
- more common among women aged 20 to 40
- associated with anxiety, depression, posttraumatic stress disorder, and personality disorders
- Symptoms are usually inspiratory stridor and less often expiratory wheezing, hoarseness, throat tightness, a choking sensation, and cough
- Diagnosis is made by observing inspiratory closure of the vocal cords with direct laryngoscopy. Often not suspected until pt fails to improve on asthma treatment.
- Treatment :counseling from a speech therapist on special breathing techniques,
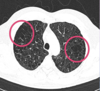
- Chest X-ray or CT scan
- Caseating granuloma in the apical lung
- Miliary granulomas
- Hilar and paratracheal lymphadenopathy
- Calcified granuloma + associated lymph node = Ghon Complex
- Segmental atelectasis
- Pleural effusion
Radiograph shows right apical thick-walled cavity and surrounding lung consolidation
Diagnostic Tests for TB
The radiograph shows a classic posterior segment right upper lobe density consistent with active tuberculosis.
Infected end organs typically have high regional oxygen tension.
Mediastinal, retroperitoneal, and cervical lymph nodes
Vertebral bodies
Adrenals
Meninges
GI tract
Pathophysiology of TB
What stain?
IGRA •Interferon-gamma release assay with antigens specific for Mycobacterium tuberculosis (blood test) - more specificity
AFB •Acid-fast bacilli smear and culture with drug susceptibility - Use sputum from patient collected early morning on 3 consecutive days
•HIV testing
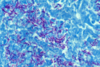
Ziehl-Neelsen stain
Diagnostic Tests for TB
- Diagnosis:
- Based on H&P (absence of historical features indicative of other similar presenting disorders) and imaging findings but must also have tissue for path
- Must demonstrate noncaseating granulomas
- TB test to rule out TB (a caseating granulomatous disease)
- CBC to rule out lymphomas
- Treatment:
- Glucocorticoids (Prednisone)
- Immunosuppressive therapy if ineffective (Methotrexate)
Sarcoidosis
Pathophysiology: 3 different types of inhalation injury?
- Thermal injury
- Chemical irritation
- Systemic toxicity/impaired tissue oxygenation (fire releases poisons)
Symptoms
- Sudden onset of symptoms
- Fever/chills
- Sore throat
- Myalgias
- Frontal or retro-orbital headache
- Nasal discharge
- Weakness and severe fatigue
- Nonproductive cough and other respiratory symptoms
- Red, watery eyes
- Nausea, vomiting, diarrhea (children)
Influenza
Physical Exam in what disease?
- Jugular venous distention
- Accentuated pulmonary valve component of the second heart sound
- Right-sided third heart sound
- Tricuspid regurgitation murmur
- Hepatomegaly
- Lower extremity edema
- Cyanosis can occur in patients with an open patent foramen ovale and right-to-left shunt due to increased right atrial pressure
Pulmonary Hypertension
Parainfluenza viruses are the most common agents, along with adenovirus, respiratory syncytial virus (RSV), and (rarely) Mycoplasma pneumoniae.
- 5% of children will have during their second year of life.
- Symptoms last for 5-7 days
- Inspiratory stridor
Chest X-ray shows “Steeple sign” =
Acute Laryngotracheitis / Croup
•A viral infection of the larynx, trachea, and the upper bronchial tree
subglottic narrowing in the neck; lungs usually appear normal

- African Americans>Caucasians
- Female slightly > male
- Presents between 20-30 years of age (though can present into the 60s)
- Another Idiopathic Disease
- Multisystem inflammatory disorder characterized by noncaseating granuloma formation
Sarcoidosis
Samter’s triad:
aspirin sensitivity, asthma, nasal polyps
- Chronic
- Complicated version (Progressive Massive Fibrosis)
- The small nodules of Simple version progress and coalesce into larger nodules (>1cm) that evolve into conglomerate masses
- Looks similar to malignancies

Pneumoconiosis – Silicosis
catarrhal, paroxysmal, and convalescent stages
Pertussis
2 weeks each, 6 total
3 Determinants of Ventilation?
- Tidal volume (Vt )
- Dead space volume (Vd)
- Respiratory frequency ( f )
- Supportive care
- Limit the number of paroxysms
- Observe the severity of cough and provide assistance when necessary; Elevate head
- Maximize nutrition, rest, and recovery
- Azithromycin is the treatment of choice for all patients.
- Trimethoprim-sulfamethoxazole if a hypersensitivity to macrolides
- Prophylaxis for exposed, susceptible persons is also azithromycin for 5 days
Treatment of Pertussis

If HIV negative: 6 to 9 mo regimen
2 months Isoniazid, Rifampin, Pyrazinamide, and Ethambutol.
If I-sensitive, stop E
•If I and R sensitive, drop P and continue I and R 4 months more
*Treatment must extend 3 months beyond documentation of negative sputum
Treatment of Active TB

Hyaline Membrane Disease?
Most common cause of?
Results in?
Deficiency of surfactant production
respiratory distress in the preterm infant
poor lung compliance and atelectasis
•Injury and damage occurs to the alveolar epithelial or capillary endothelial cells leading to inflammation (alveolitis) and eventually fibrosis
All Interstitial Lung Diseases: shared pathophysiology
A 70-year-old white female presents to the urgent care complaining of muscle aches, a severe headache, a non-productive cough, and chills. She states she woke up that morning feeling miserable. She also complains of a sore throat and a runny nose. She states she is so tired her husband had to drive her to the urgent care. She is relatively healthy but does take Toprol for hypertension. She had been out shopping with her daughter the last two days and felt fine. On exam, her temperature is 103oF, pulse is 95 bpm, respirations are 28 breaths per minute, pulse ox is 90%, and BP is 135/88. The patient appears acutely ill and diaphoretic. You hear scattered rhonchi and fine rales bilaterally in the lungs. Pharynx is erythematous and conjunctiva are injected.
What is the most likely diagnosis?
What test or tests should be performed?
Treatment in this patient will include what? Hospitalization (?),
Why does this patient qualify for a neuraminidase inhibitor?
Is there a vaccine that this patient may have missed?
What is the most likely diagnosis? Influenza
What test or tests should be performed? Chest X-ray, Rapid Influenza diagnostic test, Influenza RT-PCR and culture
Treatment in this patient will include what? Hospitalization (?), Humidified oxygen, IV hydration, Analgesics/Anti-pyretics, Neuraminidase inhibitor (Oseltamivir = Tamiflu, oral)
Why does this patient qualify for a neuraminidase inhibitor? Less than 24 hours since onset of symptoms.
Is there a vaccine that this patient may have missed? Flu vaccine.
- A paramyxovirus
- An orthomyxovirus (single stranded RNA virus) that if not neutralized by secretory antibodies, invades airway and respiratory tract cells.
Respiratory Syncytial Virus (RSV)
Influenza
Case Study
- 57 yo male with 30 pack/year history presents with new bothersome productive cough x 3 days with fever 101F. No other symptoms. No pertinent medical history. PE wnl
- What do you order???
- Diagnosis???
- Treatment???

CXR
Classic RML Pneumonia
- Outpatient: macrolide +/- B-lactam; doxycycline
- Inpatient: B-lactam + macrolide OR a respiratory fluoroquinolone
- ICU: B-lactam + macrolide OR B-lactam + fluoroquinolone
Dead Space Volume
- Anatomical =
- Alveolar =
- Physiological =
volume of air in conducting airways
gas volume in unperfused alveoli
anatomical + alveolar
What is one of the most important prognostic factors for pulmonary hypertension?
Right ventricular function
•A 6-week disease divided into catarrhal, paroxysmal, and convalescent stages, each lasting 1-2 weeks.
Pathogenesis and Presentation of Pertussis
What may be used to collect pleural fluid for culture or other testing, or can be therapeutic if the amount of fluid is large and causing lung compression?
What disease?
Thoracentesis
Adult CAP
Mendelson’s Syndrome?
CXR?
Acute Aspiration of Gastric Contents
(One of the most common causes of ARDS)
Patchy alveolar opacities in dependent lung zones
What disease?
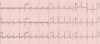
Electrocardiogram demonstrating the changes of __________________ (long arrow) with strain in a patient with __________________. Right axis deviation (short arrow), increased P-wave amplitude in lead II (black arrowhead), and incomplete right bundle branch block (white arrowhead) are highly specific but lack sensitivity for the detection of right ventricular hypertrophy.

Electrocardiogram demonstrating the changes of right ventricular hypertrophy (long arrow) with strain in a patient with primary pulmonary hypertension. Right axis deviation (short arrow), increased P-wave amplitude in lead II (black arrowhead), and incomplete right bundle branch block (white arrowhead) are highly specific but lack sensitivity for the detection of right ventricular hypertrophy

What disease?
★Chest X-ray typically shows ____________; and Ghon complex, which is?

Tuberculosis
apical caseating granuloma in the lung
a calcified focus of infection and associated lymph node

●Snoring: usually bothersome to partner, loud enough to be heard through a closed door (in adults). Snoring more than 3 times per week (in children)
OSA: history and symptoms
Normal pulmonary artery systolic pressure at rest is ____________, with a mean pressure of __________?
Pulmonary hypertension reached at pressures of?
15–30 mmHg
10-18 mmHg
>30 mmHg systolic or mean pressure >20 mm Hg.
- 6 to 9 month regimens (HIV negative)
- 2 months of daily isoniazid, rifampin, pyrazinamide, and ethambutol.
- Once the isolate is determined to be isoniazid-sensitive, ethambutol may be discontinued.
- If the isolate is susceptible to isoniazid and rifampin, the second phase of therapy consists of isoniazid and rifampin for a minimum of 4 additional months, with treatment to extend at least 3 months beyond documentation of negative sputum cultures.
Treatment of Active TB
S
P
H
E
R
E
of Lung CA complications?
- SVC syndrome
- Pancoast Tumor
- Horner Syndrome: miosis, partial ptosis, anhidrosis
- Endocrine
- Recurrent Laryngeal Nerve
- Effusions
40 - 80% of exudative pleural effusions are?
malignant
>90% of malignant pleural effusions are exudative.
Most commonly, lung cancer (1/3) and breast cancer.
•Only one with a specific test and what is it?
___________________which is a blood test with low sensitivity and high specificity. Must repeat negative or borderline tests. Two negative tests is a ‘negative’
- Also perform test on BAL effluent
- No increased risk of cancer
•BeLPT - Beryllium Lymphocyte Proliferation Test for Berylliosis
Alveolar inflammation leads to?
recruitment of inflammatory cells

Pathogens different depending on age of
<4 weeks: perinatally acquired Group B strep (first 24 hours); Gram negatives, Chlamydia pneumoniae (2-4 weeks)
4-12 weeks: more typical respiratory pathogens: S pneumo, S aureus, H influenzae, RSV
3 months - 5 years: 90% are viral. RSV commonest especially winter and early spring; influenza, parainfluenza, rhinovirus, enterovirus. Bacteria are typical respiratory bacteria: S pneumo, S aureus, H influenzae
•School-age - adolescent: Mycoplasma pneumoniae is commonest (atypical); influenza, typical respiratory bacteria also occur.
Pathogens different depending on age of
<4 weeks: perinatally acquired Group B strep (first 24 hours); Gram negatives, Chlamydia pneumoniae (2-4 weeks)
4-12 weeks: more typical respiratory pathogens: S pneumo, S aureus, H influenzae, RSV
3 months - 5 years: 90% are viral. RSV commonest especially winter and early spring; influenza, parainfluenza, rhinovirus, enterovirus. Bacteria are typical respiratory bacteria: S pneumo, S aureus, H influenzae
•School-age - adolescent: Mycoplasma pneumoniae is commonest (atypical); influenza, typical respiratory bacteria also occur.
•Primary screening method for TB infection (active or latent)
A positive test cannot determine between active and latent infections.
•Mantoux tuberculin skin test with purified protein derivative (PPD)

TREATMENT:
- Bed Rest
- Hydration
- Oxygenation
- Antipyretics/Analgesics
- Neuraminidase inhibitors
O-amivir
Z-amivir
P-amivir
•Must be administered within _________ of symptom onset?
Treatment of Influenza
- Oseltamivir (Tamiflu, oral)
- Zanamivir (Relenza, inhaled)
- Peramivir (Rapivab, IV)
24-48 hours
Optimal duration of anticoagulation therapy for venous thromboembolism is unknown.
Generally, though…
After first episode when there is a reversible risk factor?
After first episode of idiopathic thrombosis?
In patients with nonreversible risk factors or recurrent disease?
6 months
12 months
6–12 months
Antigenic drift =
Antigenic shift =
Mutation: drift = inaccurate viral RNA polymerase frequently produces point mutations in certain error-prone regions in the genes.
Gene sharing: shift = influenza genes between 2 strains are reassorted, presumably during coinfection of a single host.
Palivizumab (Synagis)
- Decreases hospitalization rates
- Decision to use this drug is based on age of child at ______ and medical history
Prevention of Acute Bronchiolitis/RSV
Not a vaccine. Monthly shots of a prophylactic monoclonal antibody.
fibrous magnesium silicate
asbestos fibers
- Most commonly caused by respiratory syncytial virus (RSV).
- Edema and accumulated cellular debris cause obstruction of small airways.
- Occurs most often in infants and young children.
- Most commonly in the first 2 years of life.
- Peak age is ~6 months.
- Leading cause of infant hospitalization.
Acute Bronchiolitis
- Diagnosis:
- Can be made on H&P and imaging alone as long as all features are present. Otherwise may require tissue for pathology via Bronchoalveolar Lavage or Transbronchial Biopsy or Surgical Lung biopsy
- Treatment and Prognosis:
- No medical management***
- Lung transplant is definitive treatment
- 5yr survival after transplant: ~50%
Idiopathic Pulmonary Fibrosis (Usual Interstitial Pneumonia)
Must be truly idiopathic: must rule out other Interstitial Diseases
- Dormant tubercle bacilli are reactivated
- Mycobacteria are released into the surrounding tissue and bloodstream causes a vigorous, nonspecific immune response
- Host becomes symptomatic and highly contagious

•Secondary Tuberculosis
Most common causes of transudatie and exudative Pleural Effusions?
Transudative: Heart failure (> 90% of cases)
Exudative: Pneumonia (parapneumonic effusion) and Cancer
Alveolar Hemorrhage Syndromes
Autoimmune causes
Anti-basement membrane antibody disease…aka?
and
Nonimmune causes
Children or young adults
Anti-glomerular basement membrane antibodies are absent
Goodpasture syndrome
Idiopathic pulmonary hemosiderosis
Croup
Inspiratory or Expiratory stridor?
Inspiratory stridor
●cyanide disrupts cellular function by inhibiting _________________, which prevents cellular oxygen utilization.
cytochrome oxidase
●Classic signs
●There may be a faint “bitter almond” smell noted on the patient’s breath or in vomitus
●This is a “classic sign,” but is not a reliable indicator
COPD chest X-ray findings

Hyaline Membrane Disease treatment antenatally?
Corticosteroids to the mother to accelerate lung maturation
Asthma Differential Diagnosis: Vocal fold paralysis
- May be unilateral (more common) or bilateral
- Etiology: ⅓ cancer, ⅓ trauma; ⅓ idiopathic
- Symptoms: unilateral paralysis, the voice may be hoarse and breadth bilateral paralysis, voice is of good quality but of limited intensity and pitch; may have stridor and dyspnea
- Diagnosis: laryngoscopy, but identification of the cause typically requires imaging (eg, MRI)
- Treatment: unilateral paralysis, surgical procedures to move cords closer together
- For bilateral paralysis, surgical procedures and measures to maintain airway foreign body aspiration laryngotracheal masses tracheal narrowing airway edema (eg, angioedema or inhalation injury)
•
- Diffusion Impairment
- Alveolar hypoventilation (normal A-aDO2)
- High altitude
Causes of Hypoxemia
i.e.,
Ventilation/Perfusion (V/Q) Mismatch
- Imaging on CXR is more variable than the other disorders but does tend more to the upper lung fields. Can appear as nodular, ground glass, or linear opacities
- Hilar and mediastinal lymph node enlargement is common
- The cutaneous nodules are on the exposed areas of skin (generally fingers and forearms) and smaller than those in Sarcoidosis
Berylliosis
•Historically was known as “Consumption”
85% of patients present with pulmonary complaints.

Tuberculosis (TB)
- Incubation period 1–4 days.
- Aerosol transmission may occur 1 day before onset of symptoms.
- Viral shedding continues for 5-10 days.
Influenza

- Presence of Amylase in Pleural effusion suggests?
- Presence of LOW Glucose in Pleural effusion suggests?
- Presence of Protein in Pleural effusion suggests?
- pancreatitis, pancreatic tumor, adenocarcinoma of the lung or pancreas, or esophageal rupture.
- if MUCH less than serum, then consider empyema (glucose consumed by bacteria)
- high in TB
Orthomyxovirus
single- or double-stranded RNA virus?
What are used to distinguish the 3 types?
___________ is most common type in humans and is genetically labile, with mutation rates as high as 300 times that of other microbes?
Influenza Virus
Single-stranded
Core nucleoproteins: A, B, and C.
Influenza A

Adult HCAP: treatment
- Broader antibiotic coverage from 3 categories:
- Duration of antibiotics _______ days depending on need for Pseudomonas coverage
- A first antipseudomonal agent (which also covers typical respiratory pathogens); e.g. imipenem, piperacillin-tazobactam
- A second antipseudomonal agent; usually a fluoroquinolone
- Coverage for MRSA; vancomycin or linezolid
8-15 days
- Fever
- Tachycardia
- Flushed face
- Conjunctival erythema
- Pharyngeal injection
Presentation of Influenza
Treatment of pulmonary vasculitis usually requires?
Given until complete remission is obtained and then is slowly tapered, and often replaced with ___________ or _________ for maintenance therapy.
corticosteroids and cyclophosphamide
methotrexate or azathioprine
Pediatric pneumonia
•All young infants (<12 weeks) should be
hospitalized
•Children over 5 rarely require hospitalization
- An obstructive, asthma-like, disorder caused by inhalation of cotton fibers.
- Presents with chest tightness, cough, wheezing and dyspnea
- Usually worse on Mondays or first day back after a break/vacation
- If left untreated and without job change, could lead to chronic bronchitis/COPD.
Byssinosis

CXR in Interstitial Lung Disease showing:
- Reticular and nodular opacities
- Pattern and distribution of opacities on CXR can help differentiate which form it is.
Nebulized Ribavirin =
a broad-spectrum antiviral agent used in severe cases of RSV
●High cost
●Lack of demonstrated benefit in decreasing hospitalization or mortality
- Most common type of lung CA in US
- Most common histology in NON-SMOKERS
- Starts in the cells that line the alveoli of the lungs/peripheral
- Metastasizes to distant organs
- Often brain
- Common path of colon CA

Non-Squamous Cell Carcinoma: i.e., Adenocarcinoma
What disease?
________ingested by macrophages which then become macules: 2-5mm radio-opaque nodules on CXR
Nodular opacities occur primarily in the upper lung fields
May become more widespread and then confluent with progression to large opacities
Pneumoconiosis – Coal Worker’s Lung
Clinical Course of?

ARDS
- The exudative phase is the acute, early phase
- A proliferative phase ensues within 7 days – prominent interstitial inflammation and early fibrotic changes
- Most patients recover approximately 21 days after the initial pulmonary injury; however, some enter the fibrotic phase (substantial fibrosis and bullae formation)
- Central vs. peripheral pulmonary
- Men=Women
- Usually younger; <60 yo
- Usually asymptomatic
- No known exposure/risk factors
Carcinoid Bronchial gland tumors, aka, bronchial adenomas
Adenoma is a benign tumor of glandular tissue
- Carries a poor prognosis in that it progresses and frequently results in respiratory failure
- Survival after onset of symptoms is typically less than 4 years.
•Acute Silicosis
Complications of what cancer?
- Pain
- Superior vena cava syndrome
- Hoarseness (recurrent laryngeal nerve, vagus nerve)
- Horner Syndrome
- Arrhythmias
- Dysphagia
- Multiple Paraneoplastic Syndromes
- Weakness and weight loss (due to aggressiveness of cancer)
Mesothelioma
CXR for what disease shows “Steeple sign” and what is it?
Croup
= subglottic narrowing in the neck; lungs usually appear normal

Solitary Pulmonary Nodule
- Size?
- Etiology?
- Risk Factors/History?
- Symptoms?
- Imaging?
- Treatment?
- Biopsy?
- Risks?
- <3 cm (if >3cm, lesion is not called nodule anymore, it’s called a called mass)
- >2cm <3cm = 80 % malignancy rate
- Cancer/Malignancy, Granuloma, Fungal infection, TB, Benign Tumor, Foreign body (rare)
- Environmental, Occupational, Smoking, Infections, Cancers
- Almost always asymptomatic/incidental finding
- CXR, CT, PET, review old imaging
- PET detects increased glucose metabolism
- High sensitivity and specificity
- PET detects increased glucose metabolism
- what’s their risk?
- low - serial imaging every 3 for 12 then 6 till 24
- after 24, considered benign
- intermediate - PET scan, biopsy
- high - surgical referral for diagnosis/treatment
- low - serial imaging every 3 for 12 then 6 till 24
- •CT guided lung biopsy/transthoracic needle aspiration (TTNA)
- Biggest risk are bleeding and pneumothorax

Interstitial Lung Disease, general findings
- Imaging: HRCT - High Res CT
- Reticular pattern
- Honeycombing
- Traction bronchiectasis
- Often in patients with poor dentition or periodontal disease
- Cough produces foul-smelling sputum
- Pneumonia and abscess usually in the dependent lung zones
What disease?
Treat with?
Adult pneumonia: anaerobic infection
penicillin or clindamycin
- Usually bronchial origin; central
- Often narrows bronchus
- More likely to have metastasis at presentation
- Rapid doubling time
- High growth fraction
- Early metastases
Small Cell
heparin followed by 3-6 months of oral warfarin results in an 80–90% reduction in the risk of
both recurrent venous thrombosis and death from PE.
- Radiologic findings in which disease?
- Focal lucencies scattered in lungs consistent with pathologic changes
- Often predominates in upper zones of each lobe.
- May reveal large bullae or blebs
- Loss of vasculature in affected areas
- Mostly ordered to assess for which form?
- and to rule out?

chest CT in COPD
emphysema
bronchiectasis
- A bacterial infection that affects airways lined with ciliated epithelium.
- Most common in the unimmunized.
- Highly contagious
- Half of all cases occur before 2.
- Adults and adolescents are reservoirs of infection.
Pertussis (Whooping Cough)

Essentials of Diagnosis for what? (must know)
Dyspnea, fatigue, chest pain, and syncope on exertion.
Electrocardiographic evidence of right ventricular strain or hypertrophy and right atrial enlargement.
Enlarged central pulmonary arteries on chest radiograph.
Elevated right ventricular systolic pressure on two-dimensional echocardiography with Doppler flow studies.
Pulmonary Hypertension
- A group of chronic fibrotic lung diseases
- Result from inhalation of inorganic dusts typically associated with specific occupations
- Symptomatology and onset can vary
- Chest radiographs generally show diffuse nodular opacities
- Prognosis varies
- Treatment is supportive
Pneumoconiosis
★A self-limiting cough lasting more than 5 days and up to 3-4 weeks
What disease?
★Acute Bronchitis
- Insidious onset of cough, dyspnea, fatigue, weight loss.
- Differentiation from IPF may be difficult, imaging is very similar.
- BAL: Low CD4 to CD8 ratio.
- There are HP antibody panels that include the most frequent antigens that can aid in diagnosis
- Tissue pathology: noncaseating granulomas, destruction of alveoli, bronchiolitis obliterans
- Treatment: chronic glucocorticoids.
- Removal from exposure still necessary but doesn’t help as much.
Chronic Hypersensitivity Pneumonitis
•palivizumab
prophylactic monthly monoclonal antibody shots against RSV
- Effective in high-risk infants (congenital heart and lung diseases, Down syndrome)
- No proven efficacy among adults with RSV
★Symptoms include: Malaise, Fever, Night Sweats, Weight loss, Productive cough, Blood-streaked sputum; Exam: Cervical lymphadenopathy and apical rales.
Tuberculosis
Four stages of what?
1) Cancer only in pleura, lateral, only one side
2) ipsilateral, spread within lung or LN on the same side
3) Spread to contralateral side, anywhere in chest wall, pericardium or ABD cavity
4) Widespread disease

Mesothelioma

- Usually unexpected/incidental
- Almost always asymptomatic/incidental finding
- Otherwise can have similar symptoms as will discuss in malignancy/compression symptoms if large

- “coin lesion”
- isolated
- <3 cm•>3cm —> MASS

Toxic lung injury due to Nitrogen dioxide inhalation
- Leads to increased tissue permeability → pulmonary edema
- Presents with dyspnea, cough, crackles on exam, occasionally wheezing as well
- Treatment is with glucocorticoids ASAP to prevent progression to bronchiolitis obliterans, a common late complication.
Silo-filler’s Disease
Rapid viral antigen testing (nasopharyngeal swab) for?
RSV//Acute Bronchiolitis
Exam finding of what disease?
- Post-tussive apical rales
- Malnourished appearance
- Painless, Cervical and SupraclavicularLymphadenopathy
- Exam findings dependent on other involved organs
Exam finding of TB
PE gets?
Admitted
HR/Helical CT Angio
Anticoagulation
Vaccine not recommended if < 6 months?
Influenza vaccine
Adenoma is?
Carcinoid is?
a benign tumor formed from glandular structures in epithelial tissue.
a tumor of a type occurring in the glands of the intestine (especially the appendix) or in the bronchi, and abnormally secreting hormones.
- More important to try to identify the causative organism
- Empiric therapy less likely to be effective
- Sputum evaluation, urine antigen testing, bronchoalveolar lavage may be done
- Thorascopic lung biopsy may be needed
- Imaging (CXR, chest CT) usually nonspecific, but should be done to assess for pulmonary emboli and to define the pattern/distribution of infiltrate
- These patients require specialty care from a team including Pulmonary, Infectious Disease, Oncology if applicable
Adult pneumonia: immunocompromised host
Treatment of ARDS?
- Mechanical ventilation = cornerstone of treatment
- •use low tidal volumes to prevent barotrauma
- Treat the underlying condition
- Supportive care
- Hemodynamic monitoring
- Oxygenation
- Fluid management
- Infection prevention
- DVT and GI prophylaxis
- Nutritional support
○Diffuse, patchy, interstitial infiltrate in
atypical pneumonia
Venous admixture =?
- amount of mixed venous blood required to mix with pulmonary capillary blood to produce observed A-aDO2
- The result of mixing of shunted non-reoxygenated blood with reoxygenated blood distal to the alveoli
Venous Admixture explains why the pO2 decreases from the heart to the systemic arteries.
Occupational Lung Disease secondary to inhalation of Inorganic Dusts
Pneumoconiosis
•Often years after cessation of job associated with exposure
Pneumoconiosis – Silicosis
- Supportive Care
- Antipyretics
- Bronchodilators
- Steroids (if severe coughing with wheezing)
- Cool mist humidifier
- Encourage immunizations (specifically for diphtheria, pertussis, and influenza)
- Since cause is most often viral, antibiotics are usually not necessary.
- Avoid use of cough suppressants (try not to mess with the mucociliary clearance!)
- Okay to use at night if patient needs sleep
Treatment of Acute Bronchitis
Pulmonary Embolism
- Treatment of choice?
- Thrombolytic therapy
- Inferior vena cava filter
- Pulmonary embolectomy
- Anticoagulation: not definitive therapy but a form of secondary prevention. It slows additional thrombus formation, allowing endogenous fibrinolytic mechanisms to lyse existing clot. Heparin followed by 3-6 months of oral warfarin results in an 80–90% reduction in the risk of both recurrent venous thrombosis and death from PE
- Accelerates resolution of emboli within the first 24 hours compared with standard heparin therapy. No difference in outcome or improved mortality compared with heparin and warfarin. Thrombolytic therapy is for patients at high risk for death where rapid resolution of thrombus may be lifesaving.
- For recurrent thromboembolism despite adequate anticoagulation. Temporary placement/not long-term (ie pre-surgery if high risk)
- Emergency procedure of last resort with a very high mortality rate. It is performed only in a few specialized centers. Catheter devices are used to fragment and extract thrombus through a transvenous approach
Farmers and bird lovers get this.
Exam with basilar crackles and tachypnea.
Acute form has an abrupt onset (w/in 4-6 hrs) of fever, chills, malaise, nausea, cough, chest tightness, dyspnea.
Chronic has Low CD4 to CD8 ratio
CXR frequently normal
Potentially confused with a viral or bacterial infection and given antibiotics
Treatment is removal from environment where exposure occurred and not return. Symptoms subside within 12hrs to several days.
Disease may recur with reexposure
Tissue Pathology shows noncaseating granulomas
Hypersensitivity Pneumonitis
★A self-limiting cough lasting more than 5 days and up to 3-4 weeks
★Most commonly caused by a virus (Rhinovirus, adenovirus,…)
★Occurs most frequently in children
★Virus disrupts the mucociliary clearance in the airways
★Causes cough and wheezing
★Supportive care, cool mist humidifier, bronchodilators as needed
★Antibiotics are NOT needed! This is most likely a viral infection
★Acute Bronchitis Pearls
The virus infects the respiratory epithelial cells of the small airways, leading to necrosis, inflammation, edema and mucus secretion. The combination of cellular destruction and inflammation leads to obstruction of the small airways. The physiologic and clinical results consist of hyperinflation, atelectasis, and wheezing. In severe cases, interstitial inflammation and alveolar infiltrates also develop. Regrowth of the epithelial cell layer does not occur until approximately 2 weeks after infection, with compete recovery requiring 4 to 8 weeks.
Edema and accumulation of cellular debris in small airways leads to obstruction causing a ventilation-perfusion mismatch with wasted perfusion, a right-to-left shunt, and hypoxemia early in the course of the disease.
Etiology of Bronchiolitis

Sarcoidosis
Directly observed therapy (DOT) =
a healthcare worker physically observes the patient ingest antituberculous medications in the home, clinic, hospital, or elsewhere; improves adherence to treatment. Multi-drug resistant TB may require up to two years of treatment.
- Should be suspected in:
- Adults with snoring, daytime fatigue, headaches, hypertension
- Children with adenotonsillar hypertrophy, snoring, fatigue
- Adults and kids with observed apneic episodes >10 seconds
- Adults and kids with craniofacial abnormalities
- Exam and labs usually nonspecific, done to rule out other contributing factors
- Office questionnaires helpful, sometimes required for pre-op evaluation
- Gold standard for diagnosis is overnight polysomnography
- CPAP and weight loss most effective treatments in adults
- Adenotonsillectomy most effective treatment in (otherwise healthy) children
Obstructive sleep apnea: summary
- A bacterial infection that affects airways lined with ciliated epithelium.
- Most common in unimmunized infants and adults.
- Highly contagious
- Adults and adolescents are reservoirs of infection.
Bordetella pertussis
aka
Whooping Cough

DTaP and Tdap vaccinations for what?
But?

Prevention of Pertussis
★Neither immunization nor disease confers lasting immunity
●Standard/most effective treatments are nocturnal CPAP and weight loss
●Surgical ○Commonest procedure is uvulopalatoplasty to remove redundant tissue
OSA: treatment (adult)
What disease?
Symptoms: URI-like, Wheezing, Cough, Dyspnea, Irritability, Poor feeding, Low grade fever, Apnea
Exam: Tachypnea, Nasal flaring, Accessory muscles use, Diffuse wheezing, Fine rales, Tachycardia, Fever (but not always), Hypoxia
Bronchiolitis
- Age <3 months
- Low birth weight
- Gestational age of <29 weeks
- Low socioeconomic group
- Crowded living conditions
- Parental smoking
- Chronic lung diseases
- Neurologic diseases
- Congenital Heart disease with pulmonary hypertension
- Immunodeficiencies
- Airway anomalies
Risk Factors for Acute Bronchiolitis
- Cough lasting > 5 days and up to 3-4 weeks
- Symptoms include: fever, fatigue, and a productive cough.
- 90% are viral in origin, and 10% are bacterial.
- Infection leads to inflammation of the trachea, bronchi, and bronchioles.
- Usually self-limiting and resolves over time.
Acute Bronchitis

GOLD III
SEVERE COPD
FEV1 =?
30% - 50% predicted
GOLD I
MILD COPD
FEV1 = ?
>80% predicted
GOLD IV
VERY SEVERE (end stage) COPD
FEV1 =
Or
FEV1 =
<30% predicted OR
<50% WITH chronic resp failure
GOLD II
MODERATE COPD
FEV1 =
50% - 80% predicted
type II pneumocytes
5% of alveolar area
60% of cells
Secrete ‘surfactant’


