Flow and flitration Flashcards
(29 cards)
Kidney functions
Integrated functions of the kidney
Excretion of metabolic products e.g. urea, uric acid, creatinine
Excretion of foreign substances (drugs) -pharmacokinetics
Homeostasis of: body fluids
Electrolytes ( cell volume) S
acid-base balance
Regulate blood pressure – cardiovascular
Secrete hormones (renin, erythropoietin) -endocrinology
Deifine glomerular filtration and freely filtred
- It is the formation of an ultrafiltrate of plasma in the glomerulus
- It is a passive process: by which fluid is ‘driven’ through the semipermeable (fenestrated) walls of the glomerular capillaries into the Bowmans capsule space by the hydrostatic pressure of heart
- Blood plasma passes from the bloodstream in to the glomerulus
- It is used as a parameter to see if someone has kidney failure ( an abrupt fall in glomerular filtration is renal failure)
- freely filtrated are the solutes that have the same concentration after the glomerulus filtration as they had in the plasma
Hydrostatic pressure plays a crucial role to this passive process ( think of a ballon with wholes and how applying pressure will influence the water going out
It will be tested Concentration of ions does not change as it passes through ( example with wine)
Glomerular filtration is the initial stage of filtration during which primary urine is produeced (= a clear fluid (ultrafiltrate), completely free from blood and proteins, is produced containing electrolytes and small solutes)
Permeable to; fluids and small solutes
but impermeable to; cells, large proteins

Basic renal Process
Amount excreted= amount filtered+ amount secreted - amount absorbed

Glomerular Filtration Pressures
The driving force for glomerular filtration pressure is the _hydrostatic pressure in glomerular capillaries (_Pgc) ( which is due to the blood pressure)
What determines the glomerular pressure
- hydrostatic pressure of tubule ( Pt) -> if there is a lot of liquid inside the tubule there will be a higher pressure
- Osmotic pressure of plasma proteins that opposes the hydrostatic pressure in glomerular capillaries ( becuase one has proteins and the other doesn’t) (πgc)
Together these two determine the ultrafication pressure (Puf)
Puf = Pgc- Pt- πgc
Ultimately, there is a net ultrafication pressure of 10-20 mmHg

Glomerular Filtration Rate (GFR)
GFR = Puf x Kf
- GFR = The amount of fluid filtered from the glomeruli into the Bowmans capsule per unit of time (ml/min).
- Convert pressure into flow rate ( surface are and size in holes in the membrane)
- Sum of filtration rate of all functioning nephrons
- Loss of nephrons = loss of surface area = fall in Kf = fall in GFR
- Index of kidney function
- Increase the holes
- Surface area à in kidney there are lots of nephrons (consists of million of those can be lost due to disease, or one kidney can be lost à leading to a decrease in the surface area
- Membrane permeability–> blood vessels can open up due to in inflammation
- If there is protein in urine there is inflammation because there are bigger holes in the vessels
Kf is an ultrafication co-efficient ( membrane permeability and filtration)
Any changes in filtration forces or Kf will result in GFR imbalances.
Kidney diseases may reduce number of functioning glomeruli = reduced surface area = Kf
Dilation of glomerular arterioles by drugs/hormone will Increase Kf
Renal blood flow
Renal Blood flow
- Rate of blood flow
- Cardiac utput 5 l pe min so kidney will have 1L per minute
- Plasma is the one filtered
- How to calculate how much plasma is the in blood -à calculate haematocrit about 60%
- About 20% is filtered by the glomerulus
- Delivers oxygen, nutrients and substances for excretion
- Renal blood flow (RBF) = approximately (1/5 of cardiac output)
- Filtration fraction (FF) = 0.2 (ratio between RPF and amount of filtrate filtered by glomerulus, which is normally 20%)
- Glomerular filtration rate (GFR) = RPF x FF and is approx. the volume of filtrate formed in 1 minute)
GFR depends on a number of factors:
- Glomerular capillary pressure (Pgc)
- Plasma oncotic pressure (πgc)
- Tubular pressure (Pt)
- Glomerular capillary surface area or permeability (Kf).
GFR is not a fixed value but is subject to physiological regulation. This is achieved by neural or hormonal input to the afferent/efferent arteriole resulting in changes in Puf.
Mechanisms of Autoregulation
- Myogenic mechanism: when there is high cardiac output
- The afferent arteriole is stretched
- Responds to the stretch by constriction to reduce the amount of flow and pressure
Vascular smooth muscle constricts when stretched.
Keeps GFR constant when blood pressure rises.
Arterial pressure rises → afferent arteriole stretches →
arteriole contracts → (vessel resistance increases)→ blood flow reduces and GFR remains constant:
Events affecting GFR
CauseEffect on GFR
Severe haemorrhage down
Obstruction in nephron tubule down
Reduced plasma protein concentration increase
Small increase in blood pressure np affect
In a normal individual carrying out a daily routine, GFR will be maintained at 120ml/min.
If asked to calculate include units
Renal clearance
Renal clearance
The rate at which a substance is removed by the plasma and excreted from the kidney
As substances in the blood pass through the kidney they are filtered to different degrees. The extent to which they are removed from the blood is called clearance. Clearance is the number of litres of plasma that are completely cleared of the substance per unit time.
Defined by equation: C = U x V ml/min
P
U = concentration of substance in urine
P = concentration of substance in plasma
V = rate of urine production
High clearance; vs Low clearance rate (=body retains the substance and it’s not excreted rapidly by the kidney)
Not everything is excreted from the body
e.g for Na, suppose P = 145mM, U = 290mM, V = 1ml/min.
Estimation of GFR using clearance
Estimation of GFR using clearance:
What substance do we measure if we want to calculate the GFR?
We need to measure a substance that is only filtered by the glomerulus (neither reabsorbed or filtered alter on) (Na is not useful cause it is reabsorbed)
If a molecule is freely filtered and neither reabsorbed nor secreted in the nephron then the amount filtered equals amount excreted. Thus, GFR can be measured by measuring clearance of this molecule
Examples
Inulin: - a plant polysaccharide
- freely filtered and neither reabsorbed nor secreted
- not toxic
- measurable in urine and plasma.
Gives a clearance value of 120.0ml/min which is GFR for average adult.
But not found in mammals so needs to be transfused therefore use an endogenous molecule with a similar clearance.
Practical measurement of GFR:
GFR in humans is normally estimated from creatinine clearance.
Creatinine:
- a waste product from creatine in muscle metabolism
- amount of creatinine released is fairly constant
- if renal function stable, amount creatinine in urine is stable
- low values of creatinine clearance may indicate renal failure
- high plasma creatinine may indicate renal failure
- If elevated creatine concertation –> kidney failure or if it is a really muscular guy
Renal Plasma Flow (RPF)
Renal Plasma Flow (RPF)
Measured by PAH (Para aminohippurate) clearance = 625ml/m
Everything that enters the kidney leaves in the urine
If measured the PAH it will give us the renal plasma flow
Filtered and actively secreted in one pass of the kidney, thus can be used to measure RPF.
In other words the all of the PAH is removed from the plasma passing through the kidney so its clearance equals the renal plasma flow.
Clearance, reabsorption and secretion
The amount of substance appearing in the urine reflects the combined effects of filtration, reabsorption from nephron tubule to blood and secretion from blood into the tubular fluid, such that:
Amount excreted = amount filtered - amount reabsorbed + amount secreted

Renal dignostics
RENAL DIAGNOSTICS
A fall in GFR is the cardinal feature of renal disease
If GFR falls, excretory products will build up in the plasma.
A raised plasma concentration of creatinine is diagnostic of renal disease.
Excretion of many other substances will also be impaired in renal failure - including some drugs. This needs to be taken into account when calculating drug doses - PHARMACOKINETICS.
Osmolarity
Osmolarity = measure of the solute concentration in a solution (osmoles/liter; 1 Osmole = 1 mole of dissolved solutes per liter); depends on the number of dissolved solutes present. The greater the number of dissolved particles, the greater the osmolarity
Water flows across a semi permeable membrane from a region of low osmolarity to a region of high osmolarity
If we increase salt we have to increase water and this leads to increased volume
If we decrease water we need to decrease water leading to a decrease in less volume
On an average day we consume 20-25% more water and salt than we need to replace that lost.
- Must get rid of the excess volume
- Must get rid of any excess water
- To keep osmolarity up
- Must get rid of any excess salt
- To stop osmolarity going too high
So we must get rid of the excess water so that you don’t blow up like a balloon and then you need to keep everything in balance.
If you don’t get rid of excess water you will dilute your body salt and the cells will expand,
if you don’t get rid of excess salt the cells will shrink.

Plasma compsition
Normal plasma osmolarity = 285-295 mosmol/l
Sodium ~ 140 mmol/l
chloride ~ 105 mmol/l
bicarbonate ~ 24 mmol/l
potassium ~ 4 mmol/l
Glucose ~ 3-8 mmol/l
Calcium ~ 2 mmol/l
Protein ~ 1 mmol/l
Water: most abundant component of the plasma and ECF
Sodium: most prevalent solute in the plasma and ECF
Water balance is used to regulate plasma osmolarity
The level of salt determines the ECF volume
Intracelluar 65% =25 L sadium low, potassium high
Extracellualt fluid 35% =15

How to ger rid of water
- Skin and sweat: variable but uncontrollable
- Normally about 450 mls/day
- Faeces: uncontrollable
- normally about 100 ml/day
- Respiration: uncontrollable
- 350mls/day
- Urine output: variable and controllable
- 1500 mls/day
Water reabsorption
We reabsorbed water everywhere except for the ascending Loop of Henle

Size of medulla
The larger the medulla the more concentrated the urine
Not only the size but it also depends on how active the transporters are
The relative thickness of the medulla is related to urine-concentrating ability because the medulla contains the loops of Henle. Hence larger animals, even the camel, cannot produce urine as concentrated as that of smaller mammals, because their kidney medulla is relatively small compared with its cortex. S

Urea transporters
UT-A1/3 KO
- Severe reduction in ability to concentrate urine
- Reduced urea in the inner medulla
- Increased water intake by 20%
- No ability to reduce urine output if water restricted for 24h
- Collecting duct
UT-A2 KO
- Very mild phenotype only observable on a low protein diet
- Loop of Henle
UT-B KO
- Increased urine production
- Reduced urine concentrating ability
- Weight loss
Point mutations in UT-A2 have been observed: Reduced blood pressure (reduce of more fluid)
Loss of function mutations in UT-B are observed: Reduction in urine concentrating ability (decrease ability to concentrate urine)
Disorders of Water balance

Dehydration

Maximal Antidiuresis

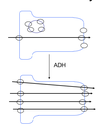
ADH -negative feedback
-Feedback control via ADH keeps plasma osmolarity in a normal range (and determines urine output and water balance)

Water Diuresis ( low ADH)

Water permeability