Fever Flashcards
(37 cards)
Meningitis
What is the definition of Meningitis?
What are the possible causes of meningitis and how servere are they?
- This occurs when there is inflammation of the meninges covering the brain, this can be confirmed by finding WBC in the CSF.
- Viral infections are the most common pathological cause, most are also self resolving.
- Bacterial meningitis has more serious consequences.
- Tuberculosis meningitis is rare in countries with low TB rates and mainly affects children under 5 years.
- Fungal and parasitic meningitis are rate and mostly affect children who are immunocompromised.
- Noninfectious meningitis can be caused by malignancy and autoimmune disease.
Meningitis
- What age group is meningitis most common in?/ What is it’s mortality and morbidity?
- What is the pathophysiology of meningitis?
-
Age group and mortality:
- Over 80% of patients with bacterial meningitis in the UK are below the age of 16. It has a mortality of 5 to 10% with over 10% of survivors being left with long term impairment.
- Pathophysiology:
- This will usually follow bacteraemia.
- A lot of the damage from the infection is from the host’s response to the infection and not the organism itself.
- Inflammatory mediators and activated leukocytes along with endothelial damage will cause cerebral oedema raised ICP and reduced cerebral blood flow.
- The inflammatory response below the meninges will cause vasculopathy resulting in cerebral cortical infarction
- Fibrin deposits may block the the resorption of CSF by the arachnoid villi, resulting in hydrocephalus.
Meningitis
- What are the common bacterial meningitis organisms at diferent ages?

Meningitis
- What are the presenting symptoms of Meningitis?
Shown below, including the differences in the CSF for each type of meningitis. The early signs and symptoms are non specific, especially in the very young. Classic headache, photophobia and neck stiffness will only be described by those old enough to talk. Still other causes can also give neck stiffness.
Children may have signs of sepsis/shock, look for:
- Tachycardia
- Tachypnea
- prolonged capillary refill time
- Hypotension.
- Any febrile child with purpura at any age should be assumed to be due to meningococcal sepsis, even if they don’t look unwell at the time.
- Signs associated with neck stiffness:
- Brudzinski sign: flexion of the neck with the child supine causes flexion of the knees and hips
- Kernig sign: with the child lying supine and with the hups and knees flexed there is back pain on extension of the knee.

Meningitis
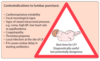
- What are the contraindications for an LP in meningitis?
Meningitis
- What are the investigations in bacterial meningitis and their results?
- What are the main options for meningitis besides and LP?
Essential ones are shown in the figure, along with their characteristic findings. Exceptions do occur. Also in the figure are the list of contraindications for doing an LP, this should not be done to prevent coning of the cerebellum through the foramen magnum.
In these cases a LP should be postponed until the child has stabilised. Without an LP a diagnosis can be made in about half of the cases:
- Blood culture and PCR
- Rapid antigen screens performed on blood and urine samples
- Throat swabs can be obtained for bacterial culture and viral PCR
- Serological diagnosis can be made with convalescent serum 4 weeks to 6 weeks after the presenting illness if necessary.

Meningitis
What are the main cerebral consiquences of bacterial meningitis?
Cerebral complications:
- Hearing loss: due to inflammatory damage to the cochlear hair cells may lead to deafness.
- Local vasculitis. This may lead to cranial nerve palsies or other focal lesions.
- Local cerebral infarction. This may result in focal or multifocal seizures, which may subsequently lead to epilepsy.
- Subdural effusion. Particularly associated with Haemophilus influenzae and pneumococcal meningitis. This is confirmed by CT scan. Most resolve spontaneously but may require prolonged antibiotic treatment.
- Hydrocephalus. May result from impaired resorption of CSF (communicating hydrocephalus) or blockage of the ventricular outlets by fibrin (non-communicating hydrocephalus). A ventricular shunt may be required.
- Cerebral abscess. The child’s clinical condition deteriorates with the emergence of signs of a space-occupying lesion. The temperature will continue to fluctuate. It is confirmed on CT scan. Drainage of the abscess is required.
Meningitis
What is the management for Bacterial Meningitis?
Management:
- Third generation cephalosporin – cefotaxime or ceftriaxone
- Beyond neonatal period dexamethasone administered as well to minimise risk of long term complications
- Younger than 1 month, Gentamicin and Benzylpenicillin
- (If are under a year, give Ampicillin)
- The choice of antibiotics will depend on the causative organism. A third generation cephalosporin e.g. Ceftriaxone is the preferred choice to cover most of the common bacterial causes.
- Increase in pneumococcal resistance to penicillin and cephalosporins worldwide but low rates in the UK.
- length of the course of antibiotics will depend on the organism and clinical response
Meningitis
- What propholaxis should be offerent and when?
Prophylaxis:
- Rifampicin to eradicate nasopharyngeal carriage (not required if 3rd gen cephalosporin given).
- Household contacts of patients who have had group C meningococcal meningitis should be vaccinated.
Meningits
- What proportion of CSN infections are viral?
- How severe is viral meningitis
- How is Viral meningitis diagnosed?
Viral meningitis:
- Up to ⅔ of central nervous system infections are viral. Causes can be EBV, adenovirus and mumps. Mumps meningitis is now rare due to the MMR vaccine.
- Viral meningitis is usually much less severe than bacterial meningitis and most cases make a full recovery.
- Diagnosis of viral meningitis is by PCR of CSF, stool, urine nasopharyngeal aspirate and throat swabs as well as serology.
Outline the traffic light system for fever
Include the Colour, activity, respiratory, hydration and other features of the patient

Common disease:
What are the signs and syptoms of:
- Meningoccoal disease
- Meningitis
- Herpes siplex
- Pneumonia
- UTI
- Septic arthritis
- Kawasaki disease

Coryza/common cold
What are the symptoms, signs, investigations and mangement of Coryza/common cold?

Pharyngitis
What are the symptoms, signs, investigations and magement of Pharyngitis?

Tonsilitis
What are the symptoms, signs, investigations and mangement of Tonsilitis?

Septicaemia
What are the symptoms, signs, investigations and mangement of Septicaemia?
Antinbiotics:
- Meningococal infection: IM Penicillin or IV Cephtriexone (follow it up with a men C vaccine)

Fever and rash
What are the common bacterial, viral and other causes of maculopapular and vesicular, bullous and pustular rashes?

Herpes simplex
What are the symptoms, signs, investigations and mangement of Herpes simplex?

EBV
What are the symptoms, signs, investigations and mangement of EBV?

Parovirus B19
What are the symptoms, signs, investigations and mangement of Parovirus B19?
Also called the fith disease since it was the fith disease described in a group of illnesses with similar rashes.
Also called “slapped cheek syndrome”
self resolving

Enteroviridae
What are the symptoms, signs, investigations and magement of Enteroviridae?

Varicella Zoster
What are the symptoms, signs, investigations and magement of Varicella Zoster?
Treament and prevention:
- Key clinical features – fever and itchy, vesicular rash which crops for up to 7 days. Median incubation time of 14 days.
- In the immunocompromised, primary varicella infection may result in severe progressive disseminated disease, which has a mortality of up to 20%. The vesicular eruptions persist and may become haemorrhagic.
- Oral acyclovir has highly variable absorption and therefore limited benefit, and is not reccomended in the UK.
- Children who are immunocompromised should be treated with IV acyclovir. This can be changed to oral valaciclovir at a later point if organ dissemination has occured.
- Human Varicella Zoster immunoglobulin is recommended for high risk individuals with deficient T cell function following contact with chickenpox.
- Be aware that a temperature that goes down and then back up could be due to a secondary bacterial infection.
- School exclusion for 5 days from when the lesions first appeared

Measles
What are the symptoms, signs, investigations and magement of Measles?
Clinical features:
shown in the image.
Complications:
- Encephalitis, occurs 8 days after the onset of the illness, 1 in 5000 affected, 15% mortality and 40% left with long term complications
- Subacute sclerosing paraencephalitis (SSPE), rare occurs in 1 in 100,000 but will manifest 7 years after the measles infection (most infections are below age of 2 years). Progresses to dementia and death, diagnosis is clinical with high Measle antibody levels and classic EEG tracing. Now rare due to the MMR vaccine
Treatment:
- supportive, children admitted to hospital should be iscolated.
- In those who are immunocompromised, ribavirin can be given which is an antivrial drug.
- Vitmain A can module the Immune response, should be given in low income countires.

Mumps
What are the symptoms, signs, investigations and management of Mumps?
Mumps is an acute systemic infectious disease caused by an RNA paramyxovirus. It is spread by the resp droplet route. Before the vaccine it used to affect mostly children and would cause parotid gland swelling.















