Female Reproductive System Flashcards
Label the anatomy of the female reproductive system?


Functions of the ovaries?
- Produce gametes (AKA oogenesis, in females)
- Produce steroids, mainly oestrogens and progestogens (mainly progesterone)
Structure of the ovaries?
Medulla - forms the core of the organ and contains loose CT, contorted arteries, veins and lymphatics; it is continuous with the hilum of the organ
Cortex - contains scattered ovarian follicles, in a highly cellular CT stroma. Outer shell is a dense CT layer (tunica albuginea), which is covered by a single layer of cuboidal cells (germinal epithelium)
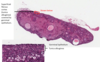
What is the germinal epithelium of the ovarian cortex?
AKA ovarian surface epithelium Holdover from a time when they were thought to give rise to gametes, i.e: the term germinal epithelium is a misnomer
Development of female ova during the embryonic development of a female?
Early, around week 6, germ cells from the yolk sac invade the ovaries and proliferate, via mitosis, to form oogonia (small diploid cell that goes on to become a primordial follicle)
These undergo development and division, via meiosis, to form mature oocytes (AKA ova)
Define oogenesis?
Development of oocytes (female germ cells), from oogonia
Define folliculogenesis?
Growth of the follicle, which consists of the oocyte and any assoc. support cells
No. of germ cells present, in both ovaries combined, during different stages of follicular development?
In a 6 week embryo, there are 1700 (in the form of germ cells)
At 7 months in utero, there are 5,000,000 (in the form of oogonia)
At birth, there are 1,000,000 (in the form of primary oocytes)
At puberty, there are 500,000 (in all types of follicles)
At menopause, there are few germ cells
Apoptosis of oognonia and oocytes is termed what?
Atresia
The cell is resorbed following cell death
Describe the process of meiosis beginning in the oocytes
Before birth, meiosis begins in the oocytes but it halts at prophase I
If the oocyte undergoes further development, meiosis will restart but many remain in this state for several decades (until fertilisation occurs, once a sperm is met)
E.g: in a 20 year old female, ~15 follicles restart development per day, dropping to ~1 per day in a 40 year old
Stages in follicular development?
Pre-antral follicles:
- Primordial follicle
- Primary follicle
- Late primary follicle
Antral follicles:
- Secondary follicle
- Mature Graafian follicle

What cells must the oocyte assoc. with?
Pre-granulosa cells (follicle cells) - these are squamous but, if the follicle enters the growth phase, they become cuboidal If the oocyte fails to assoc. with these cells, it will die

Structure of primary follicle?
Defined by the cuboidal granulosa cells (AKA follicular cells), forming the zona granulosa In the primary follicle, stromal cells are assoc. with the outside of the follicle and will go on to form the theca folliculi
The oocyte has enlarged and a layer of special EC matrix, the zona pellucida, is beginning to form between the oocyte and granulosa cells

Further development of the primary follicle, into a late primary follicle?
Granulosa cell layer proliferates (this is a hallmark of late primary follicles, i.e: instead of having one granulosa layer, they have more), so now termed the theca folliculi
Inner layers of the adjacent stromal cells (theca folliculi) transform to form a layer, called the theca interna; this goes on to secrete oestrogen precursors, which will be converted to oestrogen by granulosa cells
Outer layers remain fibroblast-like and form the theca externa

Development of the secondary follicle?
As the follicle enlarges, an antrum (space), filled with fluid, begins to form and enlarge in the granulosa cells layer, forming a secondary follicle
Overall, the follicle enlarges, as the antrum enlarges, and the granulosa and thecal layers (theca interna and theca externa) continue to proliferate

What are Graafian follicles?
The very largest antral follicles; these can reach 20mm in diameter
NOTE - the cumulus oophorus is a cloud of granulosa cells surrounding the follicle

What is the secondary oocyte and how does it form?
NOTE - this is note the same as a secondary follicle
1 day before ovulation, the oocyte in the largest Graafian follicle completes meiosis 1; instead of producing 2 equal cells, it produces:
- 1 cell called the secondary oocyte, which is similar in size to the original primary oocyte
- 1 tiny polar body, which carries the second nucleus away to degenerate
Once the secondary oocyte forms, what happens to it?
It begins the 2nd phase of meiosis but stops at metaphase II
It will only complete meiosis to become a fully mature oocyte after it has been released (during ovulation) and fertilised by a sperm, resulting in production of a 2nd polar body
What is follicle stigma?
Indicates imminent rupture of the follicle, resulting in release of the oocyte and the granulosa cells surrounding it, which are then referred to as the corona radiata
What happens to the follicle after ovulation?
Transforms into the corpus luteum with the theca and granulosa cells secreting oestrogens and progesterone, helping to prepare the uterus for implantation
What happens to the follicle if no implantation occurs?
Becomes a white-coloured CT, called the corpus albicans
What happens to the follicle if implantation occurs?
Placenta secretes HCG, preventing degeneration of the corpus luteum for a time and so maintains progesterone levels, which, in turn, maintains the pregnancy
Journey of the ovum, from the ovaries?
Funnel-shaped infundibulum moves so that its opening is adjacent to the site where the follicle ruptures
Ovum moves down the tube, propelled by gentle peristalsis and currents created by the ciliated epithelium; secretory cells in the epithelium secrete nutrients
Fertilisation usually occurs in the ampulla and the fertilised ovum is then transported to the uterus, for implantation
Histology of the ampulla of the uterine tube?
Mucosa is folded and lined by simple columnar epithelium, with ciliated cells and secretory cells (both secretion and ciliogenesis are cyclic)
This is surrounded by smooth muscle (2 layers)





