Exam 2 Flashcards
Chapters: 10, 14, 32, 34, 35, 39, 42
What are some effective coping strategies for dealing with stress?
- Must focus on the principles of balance, relaxation, and nutrition
- An imbalance of activity and rest contributes to further physiologic and physical signs of stress
- Time management: prioritizing tasks, setting goals, increasing concentration skills, decreasing distractions, avoiding procrastination, setting boundaries, and maintaining self discipline
- Anger management: **may need the assistance from a professional for effective application** BUT expressing feelings in a calm and non-confrontational manner, exercising, identifying potential solutions, taking a time out, forgiving, diffusing the situation with humor, “owning” the negative feelings, and doing deep breathing exercises
- Nutrition management: eating a balanced diet (fruit, vegetables, legumes, fish, poultry, & whole grains), multivitamins, and herbal supplements
- Support Groups: **Social worker can help with this** they find legitimate support groups that are national recognized. This can help people feel like they are not alone
- CAM therapy: therapeutic touch, Reiki, biofeedback, massage therapy, relaxation, guided imagery; these are mind-body therapies and may require additional education to facilitate
Factors involved in coping with stress?
- Number, duration, and intensity of stressors
- Past experiences
- Current support system
- Available resources (financially)
What is Health Literacy?
AND
How should education be written for a patient?
the ability to obtain, process, and understand basic information and services needed to make appropriate health decisions and follow instructions for treatment
- Mutually agreeable outcomes
- Prioritize the learning objectives with clients needs
- Methods that emphasize the learning style
- Age appropriate
- Speak and write in the second person, not the third (your leg, NOT the leg)
- Avoid using all caps, minimize white space, and small type in print materials
- Provide electronic education resources
- Use reliable internet sources
- Organize learning activities to move from simple to more complex tasks (known to unknown concepts)
- Speak and write in active voice (“take the medication” and not “the medication should be taken”)
- Incorporate active participation
- Schedule teaching sessions at optimal times for learning
Physical signs of fluid excess?
AKA: Hypervolemia
- Vitals: Tachycardia, bounding pulse, hypertension, tachypnea, increased central venous pressure
- Neuromusculoskeletal: Confusion, muscle weakness
- GI: Weight gain, ascites (fluid in the gut)
- Respiratory: Dyspnea, orthopnea, crackles
- Other Findings: Edema, distended neck veins
Causes of Hypervolemia
FLUID RETENTION
- Heart failure, cirrhosis, and an increase in glucocorticosteroids can cause chronic stimulus to the kidney to conserve sodium and water
- Kidney failure can cause altered kidney function with reduced excretion of sodium and water
- Hypertonic fluid and burns can cause interstitial to plasma fluid shifts.
- Sodium bicarbonate antacids, hypertonic enema solutions can cause excessive sodium intake from IV fluids, diet, or medications
- Head injuries
- Barbiturates
- Anesthetics
- Water replacement without electrolyte replacement
- Syndrome of inappropriate ADH production
Physical Signs of Dehydydration?
AKA: Hypovolemia
Vitals: Hypothermia, tachycardia, thready pulse, hypotension, decreased central venous pressure, tachypnea, hypoxia
Neuromusculoskeletal: Dizziness, syncope, confusion, weakness, fatigue
GI: Thirst, dry mucous membranes, dry furrowed tongue, nause, vomiting, acute weight loss Renal: Oliguria (decreased production of urine)
Other: Diminished capillary refill, cool clammy skin, diaphoresis, sunken eyeballs, flattened neck veins, absence of tears, decreased skin turgor
Causes of dehydration?
- Hyperventilation
- Prolonged fever
- Diabetic ketoacidosis
- Enteral feeding without sufficient water intake
- Diarrhea, vomities, NG suctioning
- Diaphoresis
- Diuretic therapy, diabetes insipidus, kidney disease, adrenal insufficiency, osmotic diuresis
- Burns
- Loss from a wound
- Hemorrhage
- Anorexia, nausea, impaired swallowing, confusion, NPO
Importance of ambulation related to postoperative surgery?
think ABC – Airway, Breathing, Circulation
Big Picture:
-
Neurological: Altered sensory perception
- Ineffective coping
-
Cardiovascular-Orthostatic hypotension
- Less fluid volume in circulatory system
- Diminished autonomic response
- Decreased cardiac output leading to poor cardiac effectiveness, which results in increased cardiac workload
- Increased O2 requirement
- Increased risk of thrombus development
-
Respiratory-decreased oxygenation and carbon dioxide exchange
- Stasis of secretions and decreased and weakened respiratory muscles (can result in collapsed lung & hypostatic pneumonia)
-
Integumentary-increased pressure on skin
- Decreased circulation to skin causing pressure ulcers
-
Metabolic-altered endocrine system
- Loss of appetite
- Loss of weight
- Alterations in calcium, fluid, and electrolytes
- Reabsorption of calcium from bones
- Decreased urinary elimination of calcium resulting in hypercalcemia
-
Elimination
- Change in calcium metabolism with hypercalcemia resulting in renal calculi
- Poor perineal care, decreased fluid intake, catheter can cause UTIs
- Decreased peristalsis
- Constipation, then fecal impaction, then diarrhea
-
Musculoskeletal
- Decreased muscle endurance, strength, and mass
- Impaired balance
- Atrophy of muscles
- Osteoporosis
- Altered joint mobility
Explain evisceration and how it happens.
The displacement of organs outside the body. Risk factors; The presence of an evisceration is a surgical emergency. Usually trauma related.

Explain dehiscence and how it happens.
Def: the partial or total rupturing of a sutured wound; usually involves an abdominal wound in which the layers below the skin also separate.
Risk factors: (1) A patient who is at risk for poor wound healing (e.g., poor nutritional status, infection) is at risk for dehiscence. (2) Obese patients have a higher risk of wound dehiscence because of the constant strain placed on their wounds and the poor healing qualities of fat tissue

What are the ABG normal values?
pH: 7.35 (acidic) – 7.45 (basic)
PaCO2: 45 (acidic) –35 (basic)
- high PaCO2 = hypoventilation
- low PaCO2 = hyperventilation
PaO2: 80-95 mm Hg
Bicarbonate (HCO3-): 22 (acidic) -26 (basic)
- low HCO3- = metabolic acidosis
- high HCO3- = metabolic alkalosis
O2 Saturation: 95-99%
ABG Interpretation?
Uncompensated:
Abnormal pH & CO2 OR HCO3 NOT BOTH
Partially Compensated:
All 3 are abnormal
Fully Compensated:
Normal pH & Abnormal HCO3 AND CO2
What are the rights of delegation?
Right Task –The right task is one that you delegate for a specific patient such as tasks that are repetitive, require little supervision, are relatively noninvasive, have results that are predictable, and have potential minimal risk.
Right Circumstances – Consider the appropriate patient setting, available resources, and other relevant factors. In an acute care setting patients’ conditions often change quickly. Use good clinical decision making to determine what to delegate.
Right Person – The right person is delegating the right tasks to the right person to be performed on the right person.
Right Direction/Communication – You give a clear, concise description of the task, including its objective, limits, and expectations. Communication needs to be ongoing between the registered nurse and NAP during a shift of care.
Right Supervision/Evaluation – Provide appropriate monitoring, evaluation, intervention as needed, and feedback. NAP need to feel comfortable asking questions and seeking assistance.
Describe the process of informed consent, from both ethical and legal points of view. Include implications for nursing.
- Explanation of the patient diagnosis and proposed treatment or procedure
- The name and qualifications of the person who will perform the procedure or treatment
- Available alternatives to the recommended treatment
- Possible complications of the treatment or procedure
- Patient’s right to refuse treatment without having care discontinued
- Nursing implications: The doctor must explain the above information. The nurse’s role is to make sure the patient understands it. We sign consent as a witness to that.
What are Kubler-Ross stages of grief?
- Denial (cant believe it happened)
- Anger
- Bargaining (if I only had one, what if we try other treatment, what if we go to Sweden)
- Depression (Depressed about situation)
- Acceptance
Important to remember: People do not go through this in order: they could go through anger, bargaining, and back to denial. They can go in and out in whatever form works for patient and give patient the space to go through them. We want it to be a linear process, but it’s not.
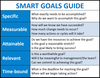
What are smart patient goals?
S: specific
M: measureable
A: attainable
R: realistic
T: timely
Examples:
Goal and Outcome #1: Patient will perform ROM exercises each hour during the shift.
Goal and Outcome #2: Patient will ambulate from bed to door twice by the end of shift.
Normal adult vital signs?
Blood pressure: 90/60 mm Hg to 120/80 mm Hg
Breathing: 12 to 18 breaths per minute; up to 22
Pulse: 60 to 100 beats per minute
Temperature: 97.8°F to 99.1°F (36.5°C to 37.3°C); average 98.6°F (37°C)
What is malignant hyperthermia?
Whare the signs and symptoms, and treatment?
Definition: Malignant hyperthermia is a rare inherited disease and potentially life-threatening condition that occurs when inhaled general anesthesia is administered OR a neuromuscular agent is administered. When this happens surgery stops and anesthesia is discontinued.
Signs & Symptoms: (during an acute episode)
- High fever (febrile)
- Cyanosis
- Muscle rigidity
- Hypertension
- Tachycardia
- Tachypnea (abnormal rapid breathing)
- Hyperkalemia (high potassium level)
- Dysrhythmias
- Acidosis
- These signs must be recognized early so treatment can begin promptly—still have a chance of dying even if treatment is started. Very serious illness!
Treatment consist of:
- Oxygen
- IV fluids
- Cooling the patient
- Dantrolene sodium (Dantrium) is used to alleviate muscle spasms
Physical signs and symptoms of stress. Are labs affected?
Keep in mind we see lab changed with acute pain—-chronic pain wouldn’t have this b/c body would have compensated for it and caught up
-
Nervous system response to stress
- Physical signs from sympathetic nervous system stimulation
- Transmits stimuli to brain
- Fear can modify the perception of a stressor.
- Hypothalamus has functions to adapt to stress.
- Nervous system direct stimulation or release of hormones:
- Increased heart rate, cardiac output, blood flow to muscles
- Dilation of bronchi, increased respiratory rate
- Pupillary dilation
Immune system response to stress
- Pain, vasodilation, and swelling
- Mobilization of white blood cells, lymphocytes
Endocrine system response to stress:
- Adrenal medulla releases hormones
- Sympathoadrenal response
- Hypothalamic-pituitary-adrenal complex
- Psychological and physiologic stressors can trigger HPA
- Corticosteroid release
- Hyperglycemia
Recall the common lab values for:
WBC
RBC
HCT
HGB
Platelets
WBC:
4,500-10,000
Importance: leukocytes. They help fight infections
“left shift”= LOTs of cells on left side (immature) and not as many on the right side (mature)—fighting infection making more
RBC:
Male: 4.5-5.5 Female: 4.0-4.9
Red blood cells are an important element of blood. Their job is to transport oxygen to the body’s tissues in exchange for carbon dioxide, which is carried to and eliminated by the lungs. Red blood cells are formed in the red bone marrow of bones.
Hct (Hematocrit):
M: 41-50% F: 36-44%
A hematocrit test measures how much of your blood is made up of red blood cells. Red blood cells contain a protein called hemoglobin that carries oxygen from your lungs to the rest of your body. Hematocrit levels that are too high or too low can indicate a blood disorder, dehydration, or other medical conditions.
Hgb (Hemoglobin):
M: 13.5-16.5 F: 12.0-15.0 Pregnant: 10-15
Is a protein in your red blood cells that carries oxygen to your body’s organs and tissues and transports carbon dioxide from your organs and tissues back to your lungs. If a hemoglobin test reveals that your hemoglobin level is lower than normal, it means you have a low red blood cell count (anemia).
Platelets:
100,000-450,000
tiny blood cells that help your body form clots to stop bleeding; When your skin is injured or broken, platelets clump together and form clots to stop the bleeding. When you don’t have enough platelets in your blood, your body can’t form clots. A low platelet count may also be called thrombocytopenia. If the platelets are too high–thrombocytosis. More likely to have clots and could be an indication of cancer.
Normal lab values for
K+
Na+
Cr
BUN
Ca++
Mg++
Cl-
Glucose
Serum Electrolytes/Blood Chemistries
Potassium (K+)
3.5-5.5
Potassium is an electrolyte that’s essential for proper muscle and nerve function. Even minor increases or decreases in the amount of potassium in your blood can result in serious health problems. Your doctor may order a potassium test if they suspect you have an electrolyte imbalance or as part of a routine check-up. Hyper/hypokalcemia
Sodium (Na+)
135-145
Hypernatremia involves dehydration, which can have many causes, including not drinking enough fluids, diarrhea, kidney dysfunction, and diuretics. Mainly, people are thirsty, and if hypernatremia worsens, they may become confused or have muscle twitches and seizures. Blood tests are done to measure the sodium level.
Serum Creatinine (Cr)
0.6-1.35
Doctors measure the blood creatinine level as a test of kidney function. The kidneys’ ability to handle creatinine is called the creatinine clearance rate, which helps to estimate the glomerular filtration rate (GFR) – the rate of blood flow through the kidneys.
Blood Urea Nitrogen (BUN)
Adults: 7-18
Child: 5-20
Infant: 5-15
Measures the amount of nitrogen in your blood that comes from the waste product urea. If your levels are off the normal range, this could mean that either your kidneys or your liver may not be working properly.
Calcium (Ca++)
8.5-10.9
Ordered to screen for, diagnose, and monitor a range of conditions relating to the bones, heart, nerves, kidneys, and teeth. The test may also be ordered if a person has symptoms of a parathyroid disorder, malabsorption, or an overactive thyroid.
Magnesium (Mg++)
1.5-2.5
Magnesium is an important electrolyte needed for proper muscle, nerve, and enzyme function. It also helps the body use energy and is needed to move other electrolytes (potassium and sodium) into and out of cells. Magnesium is vital to regulating blood pressure and maintaining bone strength.
Chloride (Cl-)
95-105
Chloride is an electrolyte that helps balance the amount of fluid inside and outside of cells. It also helps maintain blood volume, blood pressure, and the pH of body fluids.
Glucose
70-110
A blood glucose test measures the amount of glucose in your blood. Glucose, a type of simple sugar, is your body’s main source of energy. Your body converts the carbohydrates you eat into glucose. Glucose testing is primarily done for people with type 1 diabetes, type 2 diabetes, and gestational diabetes.
Indications for various glucose lab tests (fasting, capillary, glycosylated hemoglobin, glucose tolerance)?
Fasting CBC- preferred method for diagnosing diabetes, because it is easy to do, convenient, and less expensive than other tests.
Capillary (e.g. Accu-Chek)- is important for everyday monitoring of glucose levels
Glycosylated hemoglobin, glucose tolerance (Hemoglobin A1c)—used to test used to determine how well your diabetes is being controlled (FOR LONG TERM GLUCOSE CONTROL)
Hemoglobin A1c has many other names such as glycohemoglobin, glycated hemoglobin, glycosylated hemoglobin, and HbA1c.
- Hemoglobin A1c is a protein on the surface of red blood cells that sugar molecules stick to, usually for the life of the red blood cell (about three months).
- The higher the level of glucose in the blood, the higher the level of hemoglobin A1c is detectable on red blood cells.
- Hemoglobin A1c levels correlate with average levels of glucose in the blood over an approximately three-month time.
Signs, Symptoms, & Causes of hypokalemia
Hyponatremia (not enough sodium)
Underlying causes:
- Hypovolemic, Hyponatremia Diuretics
- GI fluid loss (vomitng, diarrhea)
- Profuse diaphoresis
- Hypervolemic, Hyponatremia Water Intoxication
- Prolonged use of hypotonic IV solutions
- SIADH (Syndrome of Inappropriate Antidiuretic hormone secretion: A condition in which high levels of a hormone cause the body to retain water.)
Clinical Manifestations:
- Lethargy, confusion, weakness, muslce cramping, seizures, anorexia, nausea, vomiting, osmolarity <280
Interventions:
- Monitor vital signs
- Monitor I&Os
- Monitor lab results (e.g. serum sodium & osmolality)
- Encourage foods high in sodium
- Restrict water intake
- Administer hypertonic IV solutions as ordered

Signs, Symptoms, & Causes of Hypernatremia
Hypernatremia (too much sodium)
Underlying Causes:
(Excess sodium due to)
- Excessive sodium intake
- Hypertonic IV solutions
- Hypertonic enteral feedings without adequate water
(Excessive loss of water due to)
- Diarrhea
- Inadequate intake of water
- Insensible loss due to fever
Clinical Manifestations:
- Thirst, dry sticky mucous membranes, weakness, elevated temperture
- Severe hypernatremia causing confusion and irritability, decreased levels of consciousness, hallucinations, and convulsion
- Serum osmolarity >300
Interventions:
- Monitor vital signs
- Monitor level of consciousness
- Monitor I&Os
- Monitor lab results (e.g. serum sodium & osmolarity)
- Limit salt intake and foods high in sodium
- Increase water intake
- Administer hypotonic IV solutions as ordered

What are the signs, symptoms, and causes of Hypokalemia?
Hypokalemia (loss of potassium)
Underlying Causes:
(Loss of potassium due to)
- Vomiting, gastic suction, diarrhea
- Laxative abuse, frequent enemas
- Use of potassium-wasting diuretics
- Inadequate intake seen in anorexia, alcoholism, debilitated parents
- Hyperaldosteronism
Clinical Manifestations:
- Weak, irregular pulse
- Fatigue, lethargy
- Anorexia, nausea, vomiting
- Muscle weakness & cramping
- Decreased peristalsis (hypoactive bowel sounds)
- Paraesthesia
- Cardiac dysrhythmias
- Increased risk of digitalis toxicity
Interventions:
- Monitor vital signs especially heart rate and rhythm
- Monitor cardiac rhythm w/ ECG
- Monitor lab results (e.g. potassium levels)
- Assess signs of digitalis toxicity
- Encourage foods high in potassium
- Administer potassium supplements as ordered: IV potassium is diluted properly and administered slowly usually by infusion NEVER ADMINISTER POTASSIUM AS AN IV BOLUS OR IV PUSH

What are the signs, symptoms, and causes of hyperkalemia?
Hyperkalemia
Underlying causes:
- Renal failure
- Massive trauma, crushing, injuries, burns
- Hemolysis
- IV potassium
- Potassium-sparing diuretics
- Acidosis-especially diabetic ketoacidosis
Clinical Manifestations:
- Anxiety
- Irritability
- Confusion
- Dysrhythmias (bradycardia, heart block)
- Muscle weakness, flaccid paralysis
- Paresthesia
- Abdominal Cramping
Interventions:
- Monitor vital signs (especially heart rate and rhythm)
- Monitor cardiac rhythm with ECG
- Monitor lab results (e.g.potassium levels)
- Limit potassium-rich foods
- Administer cation-exchange resins (Kayexalate) as ordered
- Administer glucose and insulin as ordered (potassium moves back into cell)

What are the sings, symptoms, and causes of hypocalcemia?
Hypocalcemia
Underlying causes:
- Hypoparathyriodism
- Pancreatitis
- Vitamin D Deficiency
- Inadequate intake of calcium-rich foods
- Hyperphosphatemia
- Chronic alcoholism
Clinical manifestations:
- Confusion, anxiety
- Numbness and tingling of extremities
- Muscle cramps that progress to tetany & convulsions
- Hyperactive reflexes
- Cardiac dysrhythmias
- Positive Chvostek & Troussea signs
Interventions:
- Monitor heart rate and rhythm
- Monitor cardiac rhythm with ECG
- Instiuite fall and seizure precautions
- Administer oral and/or IV calcium supplements as order
- Encourage calcium rich foods

What are the signs, symptoms, and causes of Hypercalcemia?
Hypercalcemia
Underlying causes:
- Prolonged bed rest
- Hyperparathyroidism
- Bone malignancy
- Piget disease
- Osteoporosis
Clinical Manifestations:
- Lethargy, stupor, coma
- Decreased muscle strength and tone
- Anorexia, nausea, and vomiting
- Constipation
- Pathologic fractures
- Dysrhythmias
- Renal calculi
Interventions:
- Monitor heart rate and rhythm
- Monitor cardiac rhythm with ECG
- Encourage increased fluid intake
- Increase patient acitivity including active ROM

What are the signs, symptoms, and causes of Hypomagnesemia
Hypomagnesemia
Underlying causes:
- Decreased intake
- TPN without magnesium
- Decreased absorption
- Nasogastric suction
- Prolonged diarrhea
- Laxative abuse
- Malabsorption syndrome
- Ulcerative colitis
- Crohn’s disease
- Increased renal excretion
- Diuresis
- Loop and thiazide diuretics
Clinical manifestations:
- Irritable nerves and muscles
- Hyperactive deep tendon reflexes
- Seizures
- Dysrhythmias (especially tachyarrhythmias)
- ECG changes
- Altered consciousness
- Mood swings
- Delusions, hallucinations
- Dysphagia, nausea, vomiting
Interventions:
- Assess vital signs (esp. heart rate and rhthym)
- Monitor cardiac rhythm with ECG
- Assess mental status, changes in LOC
- Monitor lab results (potassium and calcium)
- Assess swallowing before medication admin, food, or fluid
- Institute seizure precautions
- Administer oral or IV supplements as ordered

What are the signs, symptoms, and causes of Hypermagnesemia
Hypermagnesemia
Underlying causes:
- Excessive intake of magnesium containing antacids or cathartics
- TPN with too much magnesium
- Prolonged use of IV magnesium sulfate
- Renal failure
- Severe dehydration
- Adrenal insufficiency
- Leukemia
Clinical manifestations:
- Warm, flushed appearance
- Nausea, vomiting
- Drowsiness, lethargy
- Decreased muscle strength
- Generalized weakness
- Decreased deep tendon reflexes
- Hypotension
- Dysrhythmias (bradycardia & heart block)
- Slow, shallow respirations; respiratory arrest
Interventions:
- Assess vital signs (esp. heart rate and rhythm)
- Monitor cardiac rhythm with ECG
- Assess mental status, changes in LOC
- Assess neuromuscular strength and activitiy
- Encourage increased oral intake, increased IV fluids
- Administer loop diuretics as ordered
- Provide respiratory support (supplemental oxygen or mechanical ventilation) as needed

Signs and symtoms of hypo/hyper glycemia

Explain how we assess pain?

What is the nursing process and what do the steps mean?

What are some Isotonic solutions?
1. Normal Saline (NS; 0.9 NaCl in Water)
Use for:
- increasing circulating plasma volume when red calls are adequate
- Shock
- Fluid replacement w/ diabetic ketoacidosis
- Hyponatremia
- Blood transfusions
- Resuscitation
- Metabolic Alkalosis
- Hypercalcemia
2. Lactated Ringer’s (LR; NS w/ electrolytes and buffer)
- Water replacement
- Raises total fluid volume
- DKA after inital NS and before dextrose infusion
- Hypertonic dehydration
- Sodium & Chloride depletion
- Gastric fluid loss from nasogastric suctioning or vomiting
3. Normosol-R
- Replaces fluid and buffers pH
- Indicated for replacement of acute extracellular fluid volume losses in surgery, trauma, burns, or shock
- Used in an adjunct to restore decrease in circulatory volume in patients with moderate blood loss
4. D5W
This is a weird one. Considered isotonic but becomes free water after dextrose is metabolized; then acts as a hypotonic solution. Because it does not contain sodium, continued use can lead to hyponatremia, Useful in IV medication administration.
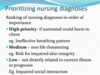
Nursing diagnosis prioritization (think in the sense of goal achievement)
It is something nurses can fix without the doctor’s order, we think about our patient’s strengths and weaknesses
General how pain effects each system

Effects of opioids (therapeutic side and adverse effects)
Opioid analgesics are the MOST effective agents for reliefing moderate to severe pain.
Examples: morphine, hydromorphone, oxycodone, fentanyl, and meperidine–best at relieving severe pain
They change a person’s perception of pain while relieving the pain
Adverse effects: Respiratory depression, seizures, nausea, vomiting, constipation, itching, and urinary rentention.
**Narcan (Naloxone) is used for the treatment of opioid analgesic overdose.
Do not give opioid meds if a patient is already really hypotensive or has a low respiratory rate
PCA: Usage and indication plus appropriate patients for PCA. Directions to patient and family
Patient Controlled Analgesia (PCA) is an IV device that allows pt. to take active role in pain control. We use PC to better control pain and there is a correlated to improved patient satisfaction. Pressing button delivers pain medicine (a predetermined dose of narcotic analgesic delivered). The physician writes an order (medication, amount, delivery mode), the nurse programs the machine, provides patient and family education, the patient presses button to receive medication, the machine has a lockout so the patient cant OD.
What is Perioperative care?
- Perioperative nursing (Pre Op Area): The care nurses provide before, during, and after surgery
-
Perioperative period: The three phases a patient goes through when having surgery
- Preoperative phase: The first phase of surgery
-
Intraoperative phase (in the OR): The second phase of surgery
- Anesthesia: An agent that makes the patient insensitive to pain and sensation
- Postoperative period (Where you recover): The third phase of surgery
Explain safety and accountability in the operating room.
Communication is important in the OR to ensure patient safety. If the sterile field or technique is broken, the behavior that does not follow pt safety guidliness is addressed immediately, such as with the following examples, “you contaminated your gloves” and “the pt’s arm is not straight; it needs to be repositioned.” The communication style of the nurse can have a positive impact on patient outcomes. Being assertive rather than aggressive is viewed more positively.
After surgery why is early ambulation so important?
Helps to prevent:
- Constipation
- Deep vein thrombosis
- Atelectasis
- Pneumonia
- Urinary stasis
Signs of complicated grief?
Definition: “unresolved grief”, occurs when the affected person is not able to process through the normal stages of grieving. It is characterized by distressing symptoms lasting at least 6 months after the death of a signficiant person.
Four types of complicated grief have been identified:
1. Chronic grief: grief reactions that do not diminish over time and continue for an indefinate period or very long period of time.
2. Delayed grief: suppression of grief reaction while the grieving person consciously or unconsciously avoids the pain that has occured with the loss.
3. Exaggerated grief: survivor is overwhelmed by grief and cannot function in daily life. They may use self-destructive behaviors such as drugs or alcohol as a coping mechanism. Potential for suicide is HIGH.
4. Masked grief: behaviors of the survivor interfere with normal functioning, but that person is not aware that these behaviors are concealing the actual grieving process.
**Complicated grief reactions are uncharcterisitc of the normal grief process and may include a greater intensity of denial, anger, or shock; verbaliziation of helplessness/hopelessness; panic attacks, substance abuse, chronic depression. If not fixed it can lead to long-lasting physical problems and serious mental health issues.


