ENT Flashcards
(16 cards)
- You are the ED intern on duty. You are asked to see and treat a 20 yoa man who has broken his nose playing football 3 hours previously. It has not stopped bleeding. You can ignore all other issues other than those related directly or indirectly to do with his nose. How will you proceed to assess and treat his nosebleed?
Epistaxis:
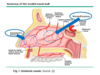
- 90% of bleeds arise anteriorly from Little’s area (Kiesselbach’s plexus)
- Kiesselbach’s plexus:
- Anterior ethmoidal artery (septal branch)
- Sphenopalatine artery (lateral nasal branch)
- Superior labial artery (septal branch)
- Greater palatine artery (septal branch)
- Kiesselbach’s plexus:
- 10% of bleeds arise posteriorly from Woodruff’s plexus:
- Usually the lateral wall but rarely the nasal septum
- Woodruff’s plexus:
- Sphenopalatine artery
- Posterior nasal artery
- Ascending pharyngeal artery
Assessment/ Management:
- ABDCE with concern re: airway and circulation
- Resus as appropriate
- Initial Tamponade + Treat Coagulopathy (CBC, PT/PTT, X-ray)
- Nose blowing
- Spray with oxymetazoline (alpha 1 agonist)
- Patient pinches alae tightly against septum and hold for 10 minutes
- Bend forward at the waist
- If bleeding stopes with conservative management
- Observe for 30 minutes for re-bleed
- Discharge with antibiotic ointment for 3 days
- Rhinoscopy
- Anterior bleed
- Cautery = chemical or electrical (silver nitrate or electrocautery)
- Anterior nasal packing = prep with topical anaesthetic and vasoconstrictor and leave for up to 3 days
- Nasal tampon
- Coat tampon with antibiotic ointment and expanding tampon by nfusing 10mL of saline
- Gauze packing
- Ribbon gauze with lubricant or antibiotic soak
- Nasal balloon catheters
- Soak catheters in sterile water – not saline, insert catheter and inflate with air
- Nasal tampon
- Persistent anterior bleeding – bilateral packing
- Follow up with ENT specialist in 1-3 days unless clear source identified and stable vitals
- Education about future epistaxis
- As above + to go to ED if bleeding continues
- Posterior Bleed
- Balloon catheter
- Shouldn’t be left for more than three days
- Insert catheter, inflate posterior balloon then anterior balloon (use air or water)
- Foley catheter
- Coat catheter with lubricant, insert and partially fill
- Patients with posterior bleed require hospitalization for monitoring
- Balloon catheter
- Surgical options
- Endoscopic ligation of sphenopalatine or anterior ethmoid artery
- Artery clipped or coagulated with diathermy
- Risks
- Blindness, decreased lacrimation, local infection, infraorbital nerve injury, sinusitis
- Angiographic embolization
- Catheter in internal maxillary artery and bleeding vessel is embolised
- No need for general anaesthesia
- Risks
- Cerebrovascular accidents, blindness
- Endoscopic ligation of sphenopalatine or anterior ethmoid artery
Prevention:
- Prevent drying of nasal mucosa with humidifiers, saline spray or topical ointments
- Avoidance of irritants
- Medical management of HTN and coagulopathies
Aetiology:
- Local Causes:
- Trauma
- Nose picking (most common)
- Fractures to the nasal septum, middle 1/3 of the face, or base of skull
- Foreign body in the nose
- Dry Nose (Rhinitis sicca)
- Vascular Malformations (e.g. nasal haemangioma, HHT)
- Nasal septal defects
- Infections
- Tumours of the nasopharynx
- Medications/ drugs (topical corticosteroids, cocaine)
- Trauma
- Systemic Causes:
- Bleeding disorders (e.g. Anticoagulation/ antiplatelets, VWD, severe thrombocytopaenia, haemophilia)
- HTN
- You are a GP, you are consulted by a 55yoa man who has a hoarse voice. What features of his history must you establish before deciding on your next steps?
Red flags:
- Recent neck trauma
- Lasting more than 4 weeks without URTI symptoms and with other symptoms of malignancy
- Night sweats, weight loss, enlarged lymph nodes
History:
- Hoarse Voice
- Symptoms onset and duration (acute vs chronic 3wks)
- Sudden or gradual
- Pattern (worse at end of day)
- Triggers
- Vocal abuse, URTI, allergens, medications
- Associated symptoms
- Cough
- Dysphagia
- GORD
- Haemoptysis
- Neck lumps
- Sore throat
- Shortness of breath
- Weight loss
- MHX/SHx
- Hypothyroid/hyperthyroid
- Asthma ICS
- GORD/ Sinus disease
- SHX
- Smoking/ Alcohol
- Occupation – politician, teacher, singer
- Risk factors for malignancy
- Smoking (past or present)
- Moderate to heavy alcohol use
- Poor nutrition
- Work place exposure to irritants e.g. wood, dust, paint fumes, chemicals
- Asbestos exposure
- Ethnicity: African American and caucasions`
Indications for referral:
- S- smoker or Stridor
- C- constant/ persistent, coughing up blood
- A – Acute onset
- L – loss of weight
- D – dyspnoea or dysphagia
- You are the ED intern on duty. Your patient is a 30 year old man who has had a sore throat for 3 days, which is getting worse. He has difficulty opening his mouth, ear pain on the right and can’t swallow his saliva. On examination he has a temperature of 39 degrees celsius, pulse 115bpm. Oral examination reveals a unilateral, left sided tonsillar swelling with a diffuse, oedematous bulge superior and lateral to the tonsil. The uvula is deviated to the right. What is the diagnosis? What is the cause of the problem?
Likely diagnosis: Tonsillitis complicated by peritonsillar abscess (Quinsy)
Quinsy triad: Trismus, uvular deviation, dysphonia
Signs of peritonsillar cellulitis or abscess:
- Unilateral tonsillar displacement
- Asymmetrical pharyngeal swelling
- Trismus (lockjaw)
- Drooling of saliva and severe unilateral ear and neck pain
- Muffled or hot potato voice
Red flags:
- Signs of peritonsillar abscess
- Swelling causing acute upper airways obstruction or dehydration due to swallowing difficulty
- Stridor or respiratory distress
Cause
Aeitology – most common deep neck infection
- Acute bacterial tonsillitis
- Streptococcus Pyogenes (most common)
- Streptococcus Anginosus
- Streptococcus Viridans
- Staphylococcus Aureus
- Haemophilus spp.
- Can also occur without preceding infection rarely
- Obstruction of Weber glands (salivary glands of the soft palate)
- Smoking is a risk factor
Explanation of symptoms
- Sore throat and difficulty swallowing from the acute infection
- Difficulty opening his mouth (trismus) due to involvement of the motor branch of CN V leading for spasm of the muscles of mastication
- Ipsilateral ear pain due to referred pain
- The uvula is deviated to the contralateral side due to palsy of CN X on the right side
- You are the ED intern on duty. Your patient is a 30 year old man who has had a sore throat for 3 days, which is getting worse. He has difficulty opening his mouth, ear pain on the right and can’t swallow his saliva. On examination he has a temperature of 39 degrees celsius, pulse 115bpm. Oral examination reveals a unilateral, left sided tonsillar swelling with a diffuse, oedematous bulge superior and lateral to the tonsil. The uvula is deviated to the right. What is the diagnosis? What is the management
Likely diagnosis: Tonsillitis complicated by peritonsillar abscess (Quinsy)
Quinsy triad: Trismus, uvula deviation, dysphonia
Signs of peritonsillar cellulitis or abscess:
- Unilateral tonsillar displacement
- Asymmetrical pharyngeal swelling
- Trismus (lockjaw)
- Drooling of saliva and severe unilateral ear and neck pain
- Muffled or hot potato voice
Red flags:
- Signs of peritonsillar abscess
- Swelling causing acute upper airways obstruction or dehydration due to swallowing difficulty
- Stridor or respiratory distress
Assessment:
- Fever,
- Appearance of tonsils and pharynx
- Cervical lymphadenopathy
- Systemic signs
- Hydration
- Modified centor score
Management:
- ABCDE – airway
- IV fluids
- Analgesia, rest
- Antibiotics if 3 or more on Modified Centor Score or at risk of nonsupportive complications
- Streptococcal pharyngitis and tonsillitis – benzathine penicillin IM single dose
- Symptomatic therapy
- Paracetamol/NSAIDs
- Medicated lozenges – antiseptic, anti-inflammatory, anaesthetics
- If recurrent
- Referral for tonsillectomy

- You are on-duty in A & E. Your next patient is a 3 year old child with rapidly progressive airway obstruction, looking toxic, drooling, tachycardic and tachypnoeic, sitting up leaning forward looking worried. The child is not immunised. What is the most important differential diagnosis? What will you do?
Most important differential diagnosis: epiglottis
Pathophysiology:
- Bacteria invades tissue of the epiglottis and/or surrounding supraglottic structures (i.e. arytenoids, aryepiglottic folds, and vallecular) this leads to supraglottic inflammation nd oedema, narrowing of the airway and airway obstruction (partial or complete)
Aetiology
- Traditionally haemophilus influenzae type b (Hib) – uncommon now due to immunisation
- Most cases now involve: strep pyogenes, strep pneumoniae, staph aureus, non-typable H influenzae
Clinical Features
- Most common in 1-4yr
- Rapid onset high fever
- Toxic appearance, anorexia, restlessness
- Cyanotic/pale
- Stridor, slow breathing, lungs clear with decreased air entry
- Pefers sitting up /tripod
- Open mouth, drooling, tongue protruding,
- Sore throat/ dysphagia
Management
- Have the parent stay with the child and assist to prevent anxiety and further obstruction of the airway
- Call for urgent review by paediatrician, ENT, anaesthetic +/- ICU teams
- The first priority is management of the airway by experienced and appropriately trained staff
- Once the airway is secured
- Empirical IV Abx – ceftriaxone
- IV fluids if required
- IV corticosteroid – dexamethasone (controversial but widely used).
- Immunise patient and close contacts (if Haemophilus influenza type B)
- Lana is a 52 year old female who is day 1 post total thyroidectomy. You are the RMO in-charge of the ward and have been called by the NUM to assess Lana urgently. Lana is having difficulty breathing and her neck looks significantly swollen. What is the most likely diagnosis? What will you do?
Most likely: post-op haematoma – rare, but lethal complication
Presentation:
- Neck swelling
- Symptoms/signs of airway obstruction due to mass like effect
- Most occur in 4-6 hrs post-op
Management:
- Review patient immediately
- MET call, anaesthetics, ICU, surg registrar
- Keep patient calm, elevate the head of the bed, give high flow O2
- Establish IV access if not already present
- Remove dressings, cut sutures to open the wound and allow blood to drain
- The patient will likely return to theatre for exploration of the wound and to achieve haemostasis
- Heather is a 4 year old girl who had a tonsillectomy 7 days ago. She presents to the ED with bleeding per orally. She has bled around 2 cupfuls of fresh blood in 30 minutes. You are one of the emergency department doctors. Heather is in waiting room. What is the diagnosis? What is your management plan?
Diagnosis: post tonsillectomy haemorrhage
Background
- 1-2% of operations
- Reduced risk if on antibiotics, adequate oral intake and adequate analgesia
- Primary – within 24hrs
- Secondary – 24hrs – 14days most commonly 6-10days
Assessment:
- ABCDE
- Amount of blood is usually more in children because they tend to swallow rather than spit
- History
- Time of operation
- Analgesia given (ibuprofen/ aspirin)
- Past history/ bleeding disorders
- Inter-current illness / URTI / febrile illnesses
- Estimated blood loss
- Examination
- Calm manner (for parents and child)
- Vitals (HR, RR, BP, cap refill, Pallor, fever)
- Look at back of throat for signs of active bleeding and/ or clot
Management:
- ABCDE / Met call if indicated
- Notify ENT registrar +/- anaesthetics +/- paediatrics
- Early IV access
- FBC, coagsm Group and Hold
- Fluids
- Consider packed cells
- Co-phenylcaine spray to oropharynx or adrenaline
- Apply a swab held in artery forceps or similar instrument to an area of bleeding or over the tonsillar beds and push laterally not posteriorly
- A 45 year old male comes to your GP practice with a 2 month history of hoarse voice. He has recently developed a swelling on the left side of his neck. He is a heavy smoker and consumes substantial alcohol daily. You are the doctor examining him. What is the most likely diagnosis and examination findings and what are relevant investigations/referrals for him?
Most likely diagnosis: Laryngeal SCC with cervical lymph node involvement
- More than 90% of laryngeal cancer is SCC
- Directly linked to tobacco and excessive alcohol use
- Glottic carcinoma associated with hoarseness of voice
- Usually 6-7th decade of life
Examinations:
- Perform head and neck examination
- Change in voice
- Cervical lymphadenopathy
- Signs of airway obstruction
- Diminished breath sounds, stridor
- Weight loss or cachexia
- Parotid or thyroid masses
- Determine characteristics of swelling
- Respiratory system
Investigations:
- Refer to ENT
- Laryngoscopy
- FNA of neck mass
- Imaging
- Neck CT with contrast
- Chest CT with contrast
- USS/MRI neck
- Whole body PET/CT
Usual presentation of laryngeal SCC:
- Hoarse voice
- Dysphagia
- Haemoptysis
- Mass in neck
- Throat pain
- Ear pain
- Airway compromise
- Aspiration
- A 45 year old female comes to your GP practice with a 1 year history of a midline neck swelling. She also gets tremors and says that her heart races at times and has lost some weight that she is pleased about. What are the relevant investigations that are related to this case?
Investigations:
- Blood
- FBC, UEC
- TSH
- fT4, T3
- thyroid antibodies
- TRAb
- Anti-TSH – grave’s
- Anti-TPO – Hashimoto’s
- Other
- ECG
- Imaging
- Neck USS +/- FNA or core biopsy
- CT neck
- Radioisotope thyroid scan

- Liam was involved in a fight yesterday at the local pub and was slapped in the face. He had a sharp shooting ear pain following the slap and says that he cannot hear too well since then. He also says that he cannot pop his ear drums since that incident. He comes to your practice. What is the most likely diagnosis and what will you expect from the examination point of view? What will be your advice?
Most likely: traumatic perforation of the tympanic membrane
- Caused by: explosions, open handed slap to the ear, head trauma, basilar #, sudden negative pressure,, iatrogenic
Examination findings:
- Otoscopy showing a tympanic membrane perforation
- There may be blood or serous discharge
- Webers Test – localised to abnormal ear
- Rinne’s Test – negative (bone conduction > air conduction)
Advice:
- Tympanic membrane usually heals spontaneously
- Keep water out of the ear
- Represent in ongoing pain – Abx if it becomes infected
- Follow up otoscopy and audiometry in 4 weeks
- Avoid bar fights in the future

- You are working as rural relief resident in a remote town GP practice. A 12yo aboriginal boy is brought in by his mum to see you as he is complaining of poor hearing in his right ear that is getting gradually worse. He gives a history of constant offensive discharge from the same ear with frequent infections. You look into his ear and see some dry white crusting wax at the top of his ear drum.

Most likely diagnosis: cholesteatoma
- Collections of desquamating stratified squamous epithelium found in the middle ear or mastoid air cells
- Congenital occur most frequently in children and young adults.
- Acquired originate from perforated or retraction of the TM allowing migration of the epithelium into the middle ear
Next steps:
- Audiometry
- High resolution CT scan of temporal bone
- Referral to ENT specialist for surgical management
- DW-MRI to exclude ddx
- Advise the family of the significance of the issue and complications
- Continued enlargement – hearing loss, nerve palsy (CN VI and VII), vertigo
- Secondary infection – potentially life threatening (meningitis, brain abscess)
- Ongoing post-operative follow up to monitor for recurrence

- You are working in emergency and you see a 4yr old boy with fever, left otalgia and acute left facial nerve palsy. What is the most likely diagnosis? What condition could this develop into that causes swelling behind the ear and the ear to stick out/forwards?
Most likely: acute otitis media
- Clinical features
- fever
- Otalgia
- Preceding URTI symptoms
- Bluging tympanic membrane
- Erythema and injection of the TM
- Irritability, sleep disturbance, decreased appetite
- Causes
- Viral – AOM preceeded by viral URTI
- Haemophilus influenzae
- Moraxella catarrhalis
- Streptococcus pneumoniae
Complications: mastoiditis (EMERGENCY)
- Serious infection of mastoid bone
- Infection spreads from middle ear cavity into the mastoid – this leads to accumulation of pus under tension and resorption of the bony walls – destruction of air cells – empyema mastoid
- Rare
- More common in children, but can affect any age
- Symptoms include:
- High fever that does not respond quickly to anti-pyretics
- Persistent throbbing ear pain (otalgia)
- Marked tenderness over the mastoid antrum
- Redness or fluctuance of the post auricular region
- Red and bulging, or perforated tympanic membrane
- The pinna may be pushed down and forward due to swelling in the post auricular region. Examination from behind may be required to assess this.
- You are working in emergency and you see a 4yr old boy with fever, left otalgia and acute left facial nerve palsy. What is the most likely diagnosis? How would you manage this boy?
Most likely: acute otitis media
Management:
- Analgesia
- Paracetamol 15mg per kg four times a day
- Antibiotics (amoxycillin) if
- ATSI
- <6mo
- Systemic symptoms: high fever, severe pain or discharging ear
- Recurrent AOM (3 episodes in 6mo)
- Bilateral otitis media
- High risk populations:
- Arrange hearing test and manage hearing loss accordingly
- If chronic consider non-urgent ENT assessment
- Urgent referral to ENT if suppurative complication develops or facial palsy develops
- Advice about
- Cease Swimming
- Avoid Flying
- Discuss prevention
- Keep air dry with swimming aids, shower cap or gently dry with hairdryer on low setting
- Ensure hand hygiene, especially after handling respiratory secretions, nasal discharge or sued tissues
- You are working in emergency and you see a 4yr old boy with fever, left otalgia and acute left facial nerve palsy. What is the most likely diagnosis? What dangerous complications can result from this condition?
Most likely: acute otitis media
Complications
- Extracranial
- Hearing loss
- Balance and motor problems
- TM perforation, sclerosis
- Middle ear atelectasis
- Cholesteatoma
- Extension to adjacent structures – mastoiditis, petrositis, labyrinthitis
- Facial nerve compression and palsy
- Intracranial
- Meningitis
- Epidural abscess
- Brain abscess
- Lateral sinus thrombosis
- Subdural empyema
- Carotid artery thrombosis
- You are the surgical ward resident. A nurse calls you saying that a patient who had frontal sinus surgery this morning had a fall in the toilet. They have also been bleeding intermittently throughout the day. What will you do?
Review patient urgently. On the phone ask if patient is conscious/unconscious and for the patients vitals, site of bleeding, and ask nurse to gather patient notes and bedside notes.
- ABCDE
- History
- Why did they fall?
- Head injury? LOC?
- Dizziness, SOB, palpitations
- Precipitating factors
- Where si the bleeding?
- PMHx – bleeding disorders, seizures, falls
- Examination
- Vitals (incl sitting and standing BP)
- Cardiorespiratory
- Neuro
- Check the surgical site
- Check notes
- Operation report
- Fluid balance
- Medications
- Investigations
- FBC, UEC, VBG, COags, BSL, Group and hold
- ECG
- Consider imaging depending on the history and examination findings
- CT head?
- Discuss with ENT registrar
Important causes of post-operative collapse
- Cardiovascular – MI, Arrythmia, fluid overload, PE, stroke
- Respiratory – respiratory depression, hypoxia
- Surgical/ infective – hypovolaemia, sepsis, severe local infection
- Metabolic – electrolyte abnormalities, BSL abnormalties, adrenal insufficiency
- Drugs – drug reaction
Frontal sinus surgery specific: intracranial haemorrhage, external haemorrhage, CSF leak, damage to ocular structures, meningitis, epistaxis
- A 65 yoa lady has presented with a lump in her right cheek, centred near the angle of the mandible. What is the differential diagnosis?
obstructive, neoplastic, infective, inflammatory, skin
Obstructive:
- Sialolithiasis (salivary duct stones)
- Chronic sialadenitis (salivary gland infection)
- Salivary duct stenosis
Neoplastic:
- Parotid pleomorphic adenoma
- Parotid adenolymphoma (Warthin’s tumour)
- Parotid adenocarcinoma
- Parotid metastasis
- Lymphadenopathy
Infective;
- Parotitis/ acute sialadenitis
- Lymphadenopathy
- mumps
Inflammatory:
- Sjogren’s syndrome
- Lymphadenopathy
Skin:
- Lipoma
- Epidermoid cyst
Given this ladies age it would be important to rule out neoplastic causes. Focused history and examination + investigation with tissue sample (FNA)


