Disorders of appetite Flashcards
(38 cards)
what can disorders in appetite be due to problems with?
water intake
foot intake
can be more or less than normal
what is polydipsia?
excessive thirst or drinking
what is adipsia?
inappropriate lack of thirst with consequent failure to drink in order to correct hyperosmolality
what is anorexia?
lack or loss of apetite for food
what is obesity?
abnormal or excessive fat accumulation that presents a risk to health
what are the causes of primary polydipsia?
mental illness
brain injuries
organic brain damage
what mental illnesses can cause polydipsia?
- psychogenic polydipsia (or acquired)
- Schizophrenia
- Mood disorders - depression and anxiety
- Anorexia
- Drug use
what can cause secondary polydipsia?
- More common
- Medical issues that disrupt any step in osmoregulation or alter ADH can cause secondary polydipsia
what are the general cases for secondary polydipsia?
chronic medical conditions
medications
dehydration
what medical conditions can cause secondary polydipsia?
- Diabetes insipidus & mellitus
- Kidney failure
- Conn’s syndrome
- Addison’s disease
- Sickle cell anaemia
what medications can cause secondary polydipsia?
- Diuretics
- Laxatives
- Both result in dehydration
- Antidepressants
what can cause dehydration?
- Acute illness
- Sweating
- Fevers
- Vomiting
- Diarrhoea
- Underhydration
what is the difference between DM and diabetes insipidus?
Diabetes mellitus (DM):
- General population - common
- Related to high blood sugar
- Treatment of high blood sugar
Diabetes Insipidus (DI):
- General population - uncommon
- Related to pituitary problems
- Impaired ADH production
- Treatment with desmopressin
what are the most common signs of diabetes?
- Always tired
- Frequent urination
- Sudden weight loss
- Wounds not healing
- Sexual problems
- Always hungry
- Blurry vision
- Numbness or tingling hands and feet
- Always thirsty
- Vaginal infections
what can cause acute kidney failure that can lead to secondary polydipsia?
- Cancer
- Sepsis/ infections
- NSAIDS
- Urinary instructions
- Trauma
- Heat stroke
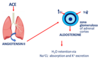
why does conn’s syndrome cause polydipsia?
primary aldosteroinism= overproduction aldosterone
aldosterone causes H2O retention via NaCl absorption and K+ excretion
what does addisons disease cause?
hypoadrenocorticoism
what are the problems caused by polydipsia?
- Kidney and bone damage
- Headache
- Nausea
- Cramps
- Slow reflexes
- Slurred speech
- Low energy
- Confusion
- Seizures
what are the biological effects of adipsia?
less water input
increased urine osmolality
stimulates the secretion of ADH
water retention
sensation of thirst decreases
what are the types of adipsia?
- type A-D (A most common)
- type A= psychogenic adipsia?
- type B= decreasing number osmoreceptors
- Type c= no osmoreceptors
- Type D= inappropriate secretion ADH
what are eating disorders?
mental disorders characterised by abnormal eating habits
what disorders are classified as eating disorders?
- Binge eating disorder
- Anorexia nervosa (fear of gaining weight- weight loss)
- Bulimia nervosa (desire for food but self induced vomiting/ laxatives)
- Pica (eating inappropriate things) (hair/soil/dust etc)
- Rumination syndrome (regurgitation and re eating)
- Avoidant/restrictive food intake disorder (narrow spectrum of food only eaten)
what are the signs of anorexia?
- Low BMI, continuous weight loss, amenorrhea, halitosis, mood swings, dry hair, skin & hair thinning
what are the causes of anorexia?
- Genetic, environmental, psychological, sociological



