Data interpretation Flashcards
Types of AKI

Name causes of anaemia:
Microcytic
Normocytic
Macrocytic

Causes of thrombocytosis and thrombocytopaenia:

Causes of hyponatraemia

Causes of abnormal potassium

Which WBCs are raised in
- bacterial infection
- viral infection
- > what else is it affected by?
When are neutrophils decreased
Bacterial
- Neutrophils
- also raised in tissue damage and steroid use
Viral
- Lymphocytes
- also raised in lymphoma and chronic lymphocytic leukaemia
Neutrophils are low in
- viral infection
- Chemo/radiothx
- Clozapine
- Carbimazole
What to be aware of with a raised urea?
Maybe because of AKI or upper GI bleed.
So if abnormal urea and normal creatinine (in patient who is not dehydrated), check haemoglobin
-> if dropped -> Upper GI Bleed probable
Liver function tests
which are used for what pathology?
Hepatocyte injury or cholestasis
- bilirubin
- ALT/AST
- ALP
Synthetic function
- Albumin
- Vit-K dependent clotting factors measured with PT/INR
- CF II, VII, IX, X
What does a raised bilirubin on its own indicate?
post-hepatic jaundice - rarely due to liver. It usually indicates haemolysis - as bilirubin is a breakdown product
What does a raised Alk Phos indicate?
Not necessarily post-hep jaundice:
ALKPHOS
Any fracture
Liver damage
K for kancer/krebs
Paget’s disease of bone and Pregnancy
Hyperparathyroidism
Osteomalacia
Surgery
Specific causes of deranged liver function tests
Prehepatic
Intrahepatic
Posthepatic

What’s the target range for TSH? How do you respond to changes?
Target range: 0.5-5
if <0.5 -> decrease dose by smallest increments offered
if >5, increase dose by smallest increment offered
Causes of hypo and hyperthyroidism (1ary and 2ary)

Main pathologies to consider on CXR (for PSA)
pneumonia
pulmonary oedema
Signs of pulmonary oedema on XR
- cardiomegaly (should be <50% of lung witdth on PA)
- bilateral and fluffy oedema (rather than unilateral -> pneumonia)
- dull costophrenic angles
Then, ABCDE
Alveolar oedema (bat wings), Kerley B Lines, Cardiomegaly, Diversion of blood to upper lobes, pleural effusions
ABGs - describe the steps for looking at them.
Check inspired O2 conc. (FiO2)
- pt on O2 should have higher FiO2
- Calculate: if PaO2 > FiO2 - 10, patient is not hypoxic. If PaO2 lower -> hypoxia
Check for resp failure
Type 1 vs Type 2 resp failure
Check acid-base status by looking at pH
acidosis vs alkalosis?
only PaCO2 abnormal - resp cause
only HCO3 abnormal - metabolic cause
Think about causes
Respiratory alkalosis caused by rapid breathing, whether due to disease or anxiety.
Respiratory acidosis has the same causes as type 2 respiratory failure.
Metabolic alkalosis caused by vomiting, diuretics and Conn’s syndrome.
Metabolic acidosis has multiple causes and the most frequent are lactic acidosis, DKA, renal failure and ethanol/ methanol/ethylene glycol intoxication. One can use the anion gap to narrow the cause (but this is beyond the scope of this book).
Which drugs have a narrow therapeutic index?
Most common ones are digoxin, lithium, phenytoin, theophylline and some Abx (gentamycin and vancomycin)
How to monitor drugs with therapeutic index? 3 basic principles
- If inadequate response to the drug and low serum drug level then increase dose. In general increase the dose by the smallest possible increment. This is especially important if the drug exhibits zero-order kinetics (such as phenytoin), as a small dose increase will lead to a large clinical effect (with higher risk of toxicity).
- If adequate response to the drug and normal or low serum drug level then no change to the dose is required, i.e. clinical response is more important. There is no point in increasing the dose just to get the patient into what is generally considered a ‘therapeutic’ range – it’s already therapeutic!
- If adequate response to the drug and high serum drug level then decrease the dose. If there is evidence of toxicity (see later in chapter) and clearly if the level is very high then omitting the drug for a few days is appropriate. The only exception to this is gentamicin, where a high serum level (without signs of toxicity) should pre-empt a decrease in frequency by 12 h rather than reducing the dose, e.g. changing from every 24 h (daily) to every 36 h (see below for explanation).
Signs of drug toxicity for:
Digoxin
Lithium
Phenytoin
Gentamycin
Vancomycin

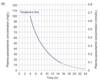
How to use paracetamol nomogram

Manage over-anticoagulation with Warfarin using INR

What do you do in case of a major warfarin bleed?
If there is a major bleed ie causing hypotension or bleeding into confined space:
- stop warfarin
- give 5-20 mg IV Vit K
- give prothrombin complex (ie Beriplex)
Target INR
2.5
unless recent thromboembolism on warfarin or metal replacement heart valve -> 3.5


