CPA #2 Flashcards
Shoulder Anatomy

How to screen for TART: Structural of the shoulder?
Shoulder height
Spine of scapula
Angle of scapula
Shoulder position in sagittal plane
What should you palpate for shoulder TART?
Joints: Glenohumeral, SC, AC
Myofascial: upper trapezius, levator scapulae, supraspinatus, deltoids, pectoralis, rhomboids
ROM Flexion and Abduction of Shoulder
180
ROM extension - shoulder
60
ROM horizontal adduction shoulder
130-140
ROM horizontal abduction shoulder
40-55
ROM internal and external rotation shoulder
90
Downward rotation of scapular motion testing
Turning on an anterior/posterior axis so that the scapula rotates in the frontal pane to tilt the glenoid fossa downward
Upward rotation of scapular motion testing
Turning on an anterior/posterior axis so that the scapula rotates in the frontal plane to tilt the glenoid fossa upward
Elevation of scapular motion testing
Superior/cephalad glide in a vertical direction along the coronal plane
Upper trapezius and levator scapulae
Depression of scapular motion testing
Inferior/caudal glide in a vertical direction along the coronal plane
Lower trapezius, lower rhomboids
Abduction (protraction) of scapular motion testing
Away from the spine, combined with a lateral tilt around the thorax
Serratus anterior
Adduction (retraction) of scapular motion testing
Moving closer to the spine
Rhmboids and middle trapezius
Backward tilt of scapular motion testing
Turning on a horizontal axis so that the posterior surface faces downward and the inferior angle is anterior
Forward tilt of scapular motion testing?
Turning on a horizontal axis so that the posterior surface faces upward and the inferior angle protrudes
Muscle Energy Steps Review

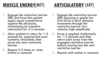
MET vs ART review
Hamstring Restriction Muscle Energy Practice
Diagnosis: left hip extension SD, left hamstring tenderpoint, left hamstring restriction
Physician: Standing, same side
Patient: Supine
Tx:
- Flex pt’s leg with knee extended. Support pt’s leg with arms or shoulder.
- Have patient puch heel towards table a/g physician counterforce for 3-5 seconds.
- Stop counterforce when pt relaxes
- Wait 1-2 seconds till tissues relax, take leg to next restrictive barrier.
- Repeat 3-5 times, ending with final push toward restrictive barrier.
- Reposition patient to neutral and reassess.

GH Joint Flexion/Extension SD MET
- Stabilize shoulder girdle with one hand, contact elbow with the other.
- Engage RB in flexion/extension based on diagnosis.
- Apply principles and steps of MET to the motions of the GH joint.
- Reassess

GH Joint IR/ER SD MET
- Stabilize shoulder girdle with one hand, contact wrist with the other.
- Engage RB in IR/ER based on diagnosis.
- Apply MET
- Reassess

GH Joint AB/ADduction SD MET
- Stabilize shoulder girdle with one hand, contact elbow with the other
- Engage RB in AB/ADduction based on diagnosis.
- Apply MET
- Reassess

GH Articulatory Tx: Spencer’s Technique
Patient: Lateral recument with shoulder to be treated up
Physician: Standing at side of table facing pt
Tx:
- Extension (every)
- Flexion (fine)
- Compression circumduction (cat)
- Traction circumduction (takes)
5a. Adduction and ER (an)
5b. Abduction (an) - IR (indoor)
- [Pump] traction with inferior glide (pee)

What does scapular elevation lead to in SC joint?
Inferior movement
Termed: SC ABduction

What does scapular depression lead to in SC joint?
Superior motion
Termed: SC ADduction

In 90 degrees shoulder flexion, what does protraction of the scapular lead to at the SC joint?
Posterior glide of the clavicle at the SC joint
Termed: SC Flexion

What does retraction of the scapula lead to at the SC joint?
Anterior glide of the clavicle at the SC joint
Termed: SC extension

SC Joint Abduction/Adduction Dx
- Pt is supine, examiner places index finger on clavicle head next to the sternum
- The pt then shrugs shoulder upward (abduction) and an inferior/caudal movement should be palpated with normal motion at SC joint
- Pt then lower shoulders downward (Adduction) and a superior/caphalad movement should be palpated

SC Joint Flexion/Extension Dx
- Pt is supine, examiner places index finger on the clavicular head next to the sternum; pt flexes shoulder to 90 degrees and reaches for ceiling forcefully (flexion)
- A posterior movement of the clavicle should be palpated with normal motion at SC joint
- Patient then lowers arm back toward the table (extension)
- An anterior movement of the clavicle should be palpated

SC Elevated/Adduction SD Articulatory Tx
- Pt lying supine with neck fully flexed by physician
- Physician places thumb over sternal end of clavicle exerting an inferior/caudal pressure
- Pt instructed to inhale and exhale fully. During exhalation, the physician springs the clavicle inferiorly to release restriction

SC Joint - Articulary Technique
Dx: Clavicle anterior and superior glide
- Pt supine, examiner opposite side of SD
- Pt helps to gap SC joint by ADducting the arm of the same side as the SD (using opposite hand to aid in the motion). Physician’s opposite hand may be placed on the table under pt’s axilla to create a fulcrum forthe pt to adduct a/g
- Articulatory springing is applied laterally, posteriorly, and inferiorly over medial end of clavicle uding hypothenar eminence
- Reassess

SC Elevated/ADducted SD MET
- Pt supine, examiner on same side as affected shoulder
- Dr. places one hand on proximal clavicular head. With the other, grasp pt’s wrist and hold arm extended and internally rotated
- Pt is instructed to raise arm a/g Dr.’s hand toward the ceiling (flexion at the shoulder) for 3-5 seconds then relax. Joint then brought to new barrier. Repeat until no new barriers or full ROM restored.

SC Horizontal Extension SD MET
- Pt supine, examiner on side of affected shoulder
- One hand on restricted clavicle, other hand placed behind axilla to cover axilla. Pt holds physician’s shoulder with hand of affected shoulder
- Flex the calvicle toward the manubrium until movement is palpated in the SC joint by pulling scapula anteriorly
- Posterior force simultaneously applied to proximal calvicle from anterior to posterior to engage RB
- Apply MET by having pt pull their shoulder down toward the table

AC Joint Dx
Reference point: Distal end of clavicle
Inspect for asymmetry: superior/inferior; step-off
Palpate
Motion screen: cross arm adduction test; +test: pain
Assess glide springing inferiorly on distal clavicle
→Resistant to springing inferiorly: clavicle superior
→Presence of sprining inferiorly: clavicle inferior
AC - Superior Clavicle ART
- Pt supine with Dr. on same side
- Dr.’s fingers monitoring AC joint and other fingers on superior aspect of clavicle; the other hand graps the pt’s forearm proximal to the wrist
- Apply a traction force in a caudad direction to gap AC joint (use enough force to register a change with the monitoring hand)
- While maintaining the traction fforce, maximally flex the arm
- Reassess

AC Joint - Direct - seated ART
Dx: Right clavicle superior glide
- Grasp elbow or forearm of dysfunctional side
- Grasp dysfunction clavicle between thumb and fingers of free hand (thumb on posterior/superior surface of distal clavicle - NOT on scapula)
- Apply anterior/inferior pressure with thumb on lateral (or posterior) aspect of clavcile while flexing pt’s elbow, extending and adducting the humerous (to gap AC j)
- Dr. holds clavcile antero-inferior (with thumb). Shoulder is extended into a circulatory sweep, posterior, superior, then anteromedial while maintaining adduction and capsular tension
- Recheck

External and internal rotation ofthe humerous leads to what rotation of the clavicle at the AC joint?
External and internal rotation (respectively)
AC Joint IR/ER Evaluation
- Pt seated, physician stands behind pt
- One hand contacts and stabilizes the calvicular side of the joint with index finger over the AC joint, noting if patient has tenderness
- Note asymmetry of joint gap compared to opposite side
- Flex, abduct (approx 45 degrees) to maximally engage the AC component of GH rotation
- IR and ER to assess for 90 degrees
- Note restriction of motion and ease of motion
- Name dysfunction based on the direction of ease of motion (IR or ER)

AC Internal Rotation SD MET
- Pt seated, physician stands behind pt
- Dr. places hand on clavicle just medial to AC joint while grasping wrist with other hand
- Add compressive force to stabilize clavicle/AC joint while flexing, abducting and ER to RB
- Apply the principles of MET by having the pt IR a/g Dr.’s resistance for 3-5 seconds
- Repeat 3-5 times or until motion is fully restored
- Reassess

AC External Rotation SD MET
- Pt seated, physician stands behind pt
- Dr. places hand on clavicle just medial to AC joint while grasping wrist with other hand
- Add compressive force to stabilize clavicle/AC joint while flexing, abducting and IR to RB
- Apply the principles of MET by having the pt ER a/g Dr.’s resistance for 3-5 seconds
- Repeat 3-5 times or until motion is fully restored
- Reassess

Principles governing the elbow joint
- SD is found in the minor gliding motions of the joint, not the major motions
- SD of the ulnohumeral joint is usually primary and SD of the radioulnar joints is usually secondary
- Impaired function of any joint of the arm produces compensatory changes in nearby/distal joints (ie can cause secondary SD)
Note**: There is reciprocal or couple motion between the elbow and forearm/wrist. Reference point for naming dysfunction is distal ulna.
What is anterior radial head elbow SD?
East of motion with anterior glide and supination
What is posterior radial head elbow SD?
Ease of motion with posterior glide and pronation
Elbow Extension SD
Patient seated. Physician seated or standing.
- Place elbow into flexion barrier
- Pt gently attempts to extend eblow for 3-5 seconds while physician applies isometric counterforce
- Pt relaxes
- Repeat
- Reassess

Elbow Flexion SD
Patient seated, standing, or supine; shoulder flexed to 90; elbow extended.
Physician: seated or standing
- Elbow into extension barrier
- Pt flexes a/g Dr. counterforce
- Pt relaxes
- Repeat until SD is alleviated
- Reassess

Elbow ADduction SD
Pt: seated, supine or standing; elbow flexed to 30
Physician: seated or standing
- Place elbow in abduction barrier
- Pt attempts to adduct elbow for 3-5 seconds with physician giving counterforce
- Pt relaxes
- Repeat
- Reassess

Elbow ABduction SD
Pt: seated, standing, or supine; elbow flexed to 30
Dr: seated or standing
- Place elbow into adduction barrier
- Pt abducts a/g Dr. counterforce
- Pt relaxes
- Repeat
- Reassess













































