ChemPath: Metabolic Disorders and Screening 2 Flashcards
Why is it difficult to get an ammonia sample?
You need a free flowing sample, which needs to be put in ice and rushed to the laboratory
What is the main role of the urea cycle?
Taking ammonia and producing urea
How many enzymes are there in the urea cycle?
7
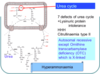
Name three other diseases that count as urea cycle defects.
- Lysinuric protein intolerance
- Hyperornithaemia-hyperammonaemia-homocitrullinuria
- Citrullinaemia type II
What do all urea cycle disorders result in?
High ammonia
NOTE: this is toxic
What is the mode of inheritance of all of these urea cycle defects?
Autosomal recessive
What is an exception to the recessive mode of inheritance of Urea Cycle Disorders?
Ornithine transcarbamylase deficiency (X-linked)
How does the body get rid of excess ammonia?
- An ammonium group is attached to glutamate to make glutamine
- So, plasma glutamine in hyperammonaemic conditions will be high
NOTE: the amino acids within the urea cycle will be high or absent. You can also measure urine orotic acid.
What is the treatment of urea cycle disorders?
- Remove ammonia (using sodium benzoate, sodium phenylacetate or dialysis)
- Reduce ammonia production (low protein diet)
Why might patients with urea cycle disorders have a slight build?
Patients may subconsciously avoid protein becuase they know it makes them feel ill
List the key features of urea cycle disorders.
- Vomiting without diarrhoea
- Respiratory alkalosis
- Hyperammonaemia
- Encephalopathy
- Avoidance or change in diet
What tends to cause hyperammonaemia with metabolic acidosis and a high anion gap?
- Organic acidurias
- Also caused by defects in the complex metabolism of branched chain amino acids
List three branched chain amino acids.
- Leucine
- Isoleucine
- Valine
Describe the breakdown of leucine.
- An ammonia group will be broken off by a transaminase and a high energy protein group will be added
- This produces a breakdown product called isovaleryl CoA
- This is then converted by isovaleryl CoA dehydrogenase
- Molecules with high energy groups cannot traverse the cell membrane, so they need to be converted to other molecules:
- Export from cell as: isovaleryl carnitine
- Excrete as: 3OH-isovaleric acid (cheesy smell) and isovaleryl glycine

Describe the presenting features of organic acidurias in neonates.
- Unusual odour
- Lethargy
- Feeding problems
- Truncal hypotonia/limb hypertonia
- Myoclonic jerks
Describe the chronic intermittent form of organic acidurias.
- Recurrent episodes of ketoacidotic coma
- Cerebral abnormalities
What is Reye syndrome?
Rapidly progressive encephalopathy that can be triggered by aspirin use in children (also triggered by antiemetics and valproate)
Describe the features of Reye syndrome.
- Vomiting
- Lethargy
- Increased confusino
- Seizures
- Decerebration
- Respiratory arrest
What would constitute the metabolic screen for Reye syndrome?
- Plasma ammonia
- Plasma/urine amino acid
- Urine organic acids
- Plasma glucose and lactate
- Blood spot carnitine profile (stays abnormal in remission)
NOTE: the top 4 need to be measured during an acute episode because the abnormal metabolites will disappear after a few days
What do defects in mitochondrial fatty acid beta-oxidation cause?
- Hypoketotic hypoglycaemia
NOTE: this means that you are unable to make ketones in between meals as an alternative energy source
Which investigations are useful for defects in mitochondrial fatty acid beta oxidation?
- Blood ketons
- Urine organic acids
- Blood spot acylcarnitine profile
What is galactosaemia?
A disorder of galactose metabolism resulting in high levels of galactose in the blood
What is the most severe and most common form of galactosaemia?
Galactose-1-phosphate uridyl transferase (Gal-1-PUT) deficiency
NOTE: high galactose-1-phosphate results in liver and kidney disease
Describe the presentation of galactosaemia.
- Vomiting
- Diarrhoea
- Conjugated hyperbilirubinaemia
- Hepatomegaly
- Hypoglycaemia
- Sepsis (galactose-1-phosphate inhibits the immune respose)



