chapters 9-11 Flashcards
(204 cards)
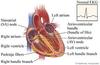
right side of the heart
receives blood from the peripheral organs and pumps it through the lungs
left side of the heart
receives oxygenated blood from the lungs and pumps it back to the peripheral organs
atria
primer pumps that fill the ventricles with blood
ventricles
contract and impart high blood pressure to the blood which is responsible for propelling the blood through the circulatory system.
Heart conduction
the heart has its own special conduction system that maintains its own rhythmicity and transmits action potentials throughout the heart.
Similarities between cardiac and skeletal muscle
- both are striated
- both have actin and myosin filaments that interdigitate and slide along each other during contraction
Unique characteristics of cardiac muscle
- has intercalated discs between cardiac muscle cells (these discs have very low electrical resistance allowing an action potential to travel freely between cardiac muscle cells)
- the cardiac muscle is a syncytium of many heart muscle cells in which the action potntial spreads rapidly from cell to cell
role of the A-V bundle
slowly conducts impulses from the atria to the ventricles
- this is an exclusive pathway because the atrial synctium and ventricular synctium are normally insulated from one another by fibrous tissue.
resting membrane potential of cardiac muscle
-85 to -95 millivolts
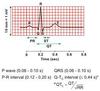
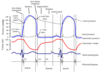
Action potential of cardiac muscle
105 millivolts
for how long does the membrane remain depolarized in the atria?
0.2 seconds
for how long does the membrane remain depolarized in the ventricles?
0.3 seconds
what causes an action potential in SKELETAL muscle?
entry of sodium through fast sodium channels which remain open for only a few 10,00ths of a second
what causes an action potential in CARDIAC muscle?
cardiac muscle also has fast sodium channels that open at the initiation of an action potential, but
cardiac muscle also has unique slow CALCIUM channels, or calcium-sodium channels
how do the slow calcium-sodium channels work?
calcium and sodium ions flow through the slow channels into the cell after the initial spike of the action potential, and they maintain the plateau.
Calcium that enters the cell through these channels also promotes cardiac muscle contraction
What else contributes to the plateau of the action potential in cardiac muscle? (prevents return of the membrane potential)
a decrease in the permeability of cardiac muscle cells to potassium ions
when the slow calcium-sodium channels close after 0.2 - 0.3 seconds, the potassium permeability increases rapidly and thus returns the membrane potential to its resting level.
what promotes cardiac muscle contraction?
diffusion of calcium into the myofibrils
the action potential spreads into each cardiac muscle fiber along the transverse (T) tubules, causing the longitudinal sarcoplasmic tubules to release calcium ions into the sarcoplasmic reticulum.
these calcium ions catylyze the chemical reactions that promote the sliding of the actin and myosin filaments along one another to cause muscle contraction.
What is an additional means of entry of calcium into the sarcoplasm that is unique to cardiac muscle?
the T tubules of cardiac muscles have 25x as great a volume as those in skeletal muscle
these t tubules contain large amounts of calcium that are released during the action potential.
the t tubules open directly into the extracellular fluid in cardiac muscle - so their calcium content is ver dependent upon extracellular calcium concentration
at the end of the plateau of the action potential, the influx of calcuim ions into the muscle fiber abruptly stops, and calcium is pumped back into the sarcoplasmic reticulum and T tubules, ending the contraction
cardiac cycle
the events that occur at the beginning of a heartbeat and last until the beginning of the next heartbeat are called the cardiac cycle.
how does each heart beat begin?
with a spontaneous action potential that is initiated in the sinus node of the right atrium near the opening of the superior vena cava

what happens after the action potential is initiated in the sinus node of the right atrium?
the action potential travels through both atria and the A-V node and bundle into the ventricles
what is the delay between atrial and ventricular contraction?
a delay of more than 1/10 of a second occurs in the A-V node and bundle, which allows the atria to contract before the ventricles contract.
when do the ventricles fill with blood?
during diastole
when do the ventricles contract?
during systole