Chapter 18: Liver Diseases Flashcards
Regeneration of the liver occurs via 2 major mechanims, which are?
1) Proliferation of remaining hepatocytes
2) Repopulation from progenitor cells
Describe the priming, growth factor, and termination phases of hepatocyte proliferation in the regenerating liver?
1) Priming - IL-6 produced by Kupffer cells act on hepatocytes making parenchymal cells competent to receive/respond to GF signals
2) GF phase - factos such as HGF and TGF-α act on primed hepatocytes to stimulate cell metabolism and entrance into cell cycle
3) Termination - hepatocytes return tp quiescence

Which 3 serum enzyme measurements represent a response to disrupted hepatocyte integrity?
- ALT
- AST
- LDH
Serum measurements of which 2 enzymes look for damage to bile canaliculus?
- Serum alkaline phosphatase
- Serum γ-glutamyl transpeptidase (GGT)
Which 2 serum measurements assess hepatocyte metabolism; which is increased in liver disease and which is decreased?
- Serum ammonia –> increased in L.D.
- Aminopyrine breath test (hepatic demethylation) –> decreased in L.D.
Accumulation of fat (steatosis) and bilirubin (cholestasis) in hepatocytes represent _________ (reversible/irreversible) changes
Reversible
What is the predominant mode of hepatocyte death seen in ischemic/hypoxic injury and is a significant part of oxidative stress?
Necrosis
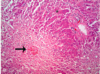
Which cells cluster at sites of hepatocyte injury and mark sites of hepatocyte necrosis?
Macrophages

Councilman bodies are the apoptotic bodies associated with what disease?
Yellow fever
What is the name of the apoptotic bodies seen in diseases such as acute and chronic hepatitis?
Acidophil bodies –> deeply eosinophilic staining
Is stem cell replenishment a significant part of parenchymal repair during hepatocyte regeneration?
- NO
- Hepatocytes are almost stem-cell like in their ability to continue to replicate even in the setting of years of chronic injury
Eventually, in chronic disease the hepatocytes reach replicative capacity (senesence) and stem cell activation occurs in the form of which reaction?
Ductular reactions
What is the principal liver cell type involved in scar deposition?
Hepatic stellate cell
The expression of which receptor by hepatic stellate cells is one of the initial changes during their activation into myofibroblasts?
PDGFR-β
What is seen encircling the surviving, regenerating hepatocytes in the late stages of chronic liver disease and give rise to the diffuse scarring described as cirrhosis?
Fibrous septa
Stellate cells transform into myofibroblasts that when stimulated by ________ can contract
Endothelin-1 (ET-1)

Chemotaxis of activated stellate cells to areas of injury are promoted by which factors?
- PDGF
- Monocyte chemotactic protein-1 (MCP-1)

If the chronic liver injury leading to scar formation is interrupted (i.e., clearance of hepatitis virus infection, cessation of alcohol use), which events occur leading to reversal of scar formation?
Which factor breaks the scars apart?
- Stellate cells stop being activated
- Scars condense –> become more dense and thin
- Metalloproteinases produced by hepatocytes break the scar apart
Acute liver failure (aka fulminant liver failure) is defined as occuring within what time period?
Associated disorders?
Pre-existing liver dysf.?
- Occurs within 26 weeks (6 months) of the initial liver injury
- Associated w/ encephalopathy and coagulopathy
- Absence of pre-existing liver disease
Acute live failure is caused by what type of tisuse injury?
Massive hepatic necrosis
What is the major cause of acute liver failure in the US?
What accounts for the rest of cases?
- Accidental or deliberate OD of Acetaminophen (major cause)
- Autoimmune hepatitis
- Other drugs/toxins
- Acute hepatitis A and B infections
With acetaminophen toxicity, how quicly does the liver failure occur?
Within one week of the onset of sx’s
In chronic inflammation which inflammatory cytokines are produced which act as stimuli for Stellate Cell activation?
- TNF
- Lymphotoxin
- IL-1β
What % of hepatic functional capacity must be lost before hepatic failure ensues?
80-90%