Cardiac Flashcards
(70 cards)
What is ischemic heart disease
characterized by an imbalance between metabolic oxygen demand and myocardial oxygen supply
- Metabolic oxygen DEMAND that EXCEEDS oxygen SUPPLY
- Most commonly caused by
-
Narrowing of coronaries →
- Atherosclerosis of the coronary arteries
-
Narrowing of coronaries →
- Can also be caused by:
- Severe hypertension or tachycardia
- extra demand on heart/O2 supply
- Coronary artery vasospasm (or plaques that lead to vasospasm)
- Supply reduced
- Severe hypotension (decreased supply to heart)
- Reduced supply
- Hypoxia
- Anemia
- Reducing O2 carrying capacity
- Severe AI or AS
- Aortic insufficiency (regurgitation)/Stenosis
- Severe hypertension or tachycardia
Incidence of ischemic heart disease?
-
Incidence
- Present in 10 million American adults
- 1.5 million suffer from MI
- 1/3 mortality
- Major cause of perioperative morbidity and mortality
- Overall incidence in surgical pts: 30% of surgical patients
Risk factors for ischemic heart disease?
MAJOR
- **increasing age
-
**male gender
- (men > 60 yo → assume they have some sort of atherosclerosis)
- Hypercholesteremia (increased LDL → more plaques)
- Diabetes
- Hypertension (increased demand)
- Cigarette Smoking
- Vascular disease → narrowing
- Positive family hx (genetic predisposition
Other:
- Obesity
- (probably have hyperlipidemia, hypercholesteremia)
- Cerebral Vascular Disease
- Peripheral vascular disease
- (for this and CVD, if they have atherosclerosis in one part of the body they probably have it in another part)
- Menopause
- Risk equalize with men
- Use of high estrogen contraceptives
- Sedentary lifestyle
- Psychosocial characteristics (high stress)
What happens when ischemic chest pain present (flowchart)?
- Angina is one of the biggest sign of ischemic heart disease
- New or changed angina = Acute Coronary Syndrome
- Acute onset of S/D issue
- New or changed angina = Acute Coronary Syndrome
GET 12 lead EKG!!!
- No ST segment elevation and negative troponin/ CK-MB = unstable angina
- Signals an impending MI
- If no ST segment elevation and positive troponin/ CK-MB= NSTEMI (myocardial infarction)
- ST segment elevation and positive troponin/ CK-MB= STEMI (ST elevated myocardial infarction)
Gold Standard- Troponin/CK-MB test
- get a 12 lead and follow this algorithm and get a cardiology consult
- ST elevation not always present in MI
- **if they tell you that their chest pain has changed –> DO NOT do the case

Pathogenesis of unstable plaques and thrombus formation?
MI→ formation of cardiac plaque that formed over time
- Body detects and grows collateral vessels over time → typically enough supplemental O2
- These are not the issue (acutely)
Atherosclerotic plaque
- Why is unstable angina not good?
- Because at any moment that person can have an MI – very high risk
- What is an unstable plaque?
- An atherosclerotic plaque with lipids inside and a thin fibrous cap
- The type of plaque is important
- Vulnerable plaques= rich lipid cores and thin fibrous caps
Athersclerotic plaque with lipid core and thin fibrous cap (typical culprit for MI)
- Causes shear force → anything causes blood to come through quicker or constriction (excited/stressed)
- Inflammation
- Apoptosis
- Macrophage- derived degradative enzymes
- (^) Responses to lipid rich core → thin fibrous cap gets sheared off and allows for rupture of plaque
- Increased inflammation with release of multiple cytokines, platelet activation and adherence → production of thrombin and vasoconstrictors (vasospasms)
- Thrombus formation over lesion plus vasoconstriction (release of thromboxane A2) of vessel → Acute decrease in coronary blood flow → lack of O2/blood arriving to myocardium →
- → UNSTABLE ANGINA OR MYOCARDIAL INFARCTION

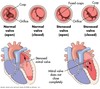
What does this picture show?

Angiography
- Plaque formation at baseline (A)
- Transient total occlusion (mental stress) (B)
- Give CCB or nitrate → allows for vasodilation of constricted vessel (C)
- Opens at the same diameter for blood to go through
*ACUTE OCCULUSION- complete occlusion distal/downstream to plaque upon exercise/stress
If meds don’t work → need stent or bypass placed
Why do you want to avoid phenylephrine in patients with a history of an MI? (pictures of the vessels)
- It can cause coronary artery vasospasm
- Also remember when surgery occurs you are causing stress
- If an occlusion occurs, administration of nitrates and nifedipine can reopen the artery to same diameter as baseline
What is the role of stress in trigerrign cardiac clinical events?
Acute mental stress –> Central and autonomic nervous system activity
-
Physiologic responses
- Increased catecholamines
- Increased HR
- Increased BP
- Decreased plasma volume
- Increased coronary constriction
- Increased platelet activity
-
Cardiac Effects
- Increased electrical instability
- (due to incr catecholamines, HR and BP)
- Increased demand (d/t incr catecholamines, HR and BP)
-
Decreased supply (d/t decr plasma volume and increased coronary constriction)
- S/D = really what leads to ischemia, plaque rupture, and ventricular F/T
- Increased electrical instability
-
Pathologic Result
- VF/VT (d/t electrical instability)
- Ischemia (d/t increased demand and decreased supply)
- Plaque rupture (d/t decreased supply and plaque rupture also leads to decreased supply)
-
Coronary thrombosis (d/t increased plt activity)
- Bottom 3 is what we see in ER → leads to MI
-
Cardiac Event
- Cardiac sudden death ( from VF/VT)
- Myocardial infarction (d/t ischemia, plaque rupture, coronary thrombosis)
-
Background factors Are (has cardiac effects)
- Atherosclerosis
- Prior MI
- Poor LV function

What are some EKG changes that can be indicative of ischemia or infarction
- ST segment depression (chronic/previous MI)
- T wave inversion
- ST segment elevation (ACUTE MI/ischemia)

What is stable angina?
- Baseline CAD, ischemic disease
-
No change in precipitating factors for at least 60 days (2 months)
- Frequency or duration of pain
- Associated with fixed narrowing (usually 75% or greater)
- O2 demand may be normal under basal conditions
-
Tx:
- Vasodilators (Nitrates or CCB)
- Relieved by rest, reducing demand
- Frequency or duration of pain
What is unstable angina?
- Caused by less than normal activity
- Lasts for prolonged period
- Occurring more frequently
- Signals impending myocardial infarction
- Imminent danger of CV event
- Crescendo- starts slow and then becomes unbearable (worse and worse)
- Increased frequency, duration, etc
- New precipitating thing changes → unable to walk up steps acutely
- Can cause irreversible infarction
- Acute plaque changes
- Usually also partial thrombosis (shear forces that dislodged plaque)
- Tx: Medically manage, stent placement, cardiac bypass
What is prinzmetal angina?
- At rest
- Coronary spasm- usually caused by this instead of atherosclerosis
- Occurrence:
- In a plaque area or normal vessel
- Associated with other vasospastic diseases (Raynaud’s Disease)
- Tx: medically manage, Nitrates, CCB
- *avoid phenylephrine (vasospasm)
- Maybe have nitro in the room
- Tx: medically manage, Nitrates, CCB
- Occurrence:
What is myocardial infarction?
- Necrosis caused by ischemia
-
Within 20-30 minutes of ischemia
- Typically begin in the subendocardial regions (in between epi and endocardial layer)
- Full damage seen 3-6 hours after ischemia occurs
- Size depends on:
- Proximity of lesion
- Collateral circulation (if no collateral circ, damage can be very great because heart hasn’t time to develop collateral)
- CKMB/troponin usually increase right away and are even higher at 3-6 hours
- Numbers correspond to size of the infarct
Complications of MI?
-
Papillary muscle dysfunction
- Causes valvular disease
-
External rupture of infarct
- day 4-7 most common – cardiac tamponade → followed by death
- Cardiac Tamponade- pericardium sac filled with blood and heart cant pump properly
- day 4-7 most common – cardiac tamponade → followed by death
- Mural thrombi – lead to stroke
-
Acute pericarditis (acute infection of the necrosed area): day 2-4 most common
- Pericardium filled with blood and leads to infection
- Ventricular aneurysm – fibrous outpouching of the ventricle- anteroapical region most common → cardiomyopathy
- Arrythmias
- LVF +/- pulmonary edema
- Cardiogenic shock (rare ~10%) → MODS
- Rupture of wall, septum, papillary muscle
-
Thromboembolism
- MI: mortality dependent on SIZE and LOCATION of thrombi/plaque
What are various sensitivities of blood tests used to detect MIs?
(Graph)Rate and extent of rise of cardiac troponin and myocardial creatine kinase (CK-MB) levels after a typical acute MI
-
Troponin level: rise QUICLKY and ACUTELY
- GOLD STANDARD→ can determine the presence and extent of injury (degree of myocardium damage)
-
Cardiac microinfarctions: can raise the troponin levels without increasing the CK-MB levels
- *Microinfarction: infarction of smaller areas and vessels
-
CK-MB level: elevated but not as good as troponin rate or rise and extent of rise
- More sensitive to larger vessels of heart

What areas of the heart are infarcted with occlusion of RCA? LCA? LAD? LCX?
- Occlusions of the coronary arteries
- RCA= posterior, inferior MI (small portion of LV)
- LCA= massive anterolateral MI (big portion of LV)
- LAD= anteroseptal MI (portion of LV and RV)
- LCX= Lateral MI
All leads some LV dysfunction → large vessels
Don’t pump properly → poor systemic outcomes

What is defnition of vascular hyertension? Incidence? Categories?
- Defined:
- Sustained diastolic of 90mmHg
-
Sustained systolic of 140mmHg
- Average of three different measurements at 3 different times
- Incidence
- 30% of general public (~1/3)
- Categories
- Normal < 120/80
- Prehypertension 120-139/80-89
- Stage 1 140-159/90-99
- Stage 2 >160/100
Importance of controlling HTN?
- HTN is the most important risk factor in
- CAD
- CVA
- Cardiac Hypertrophy- LV tries to pump against HTN → grows larger, vessels constrict → CAD
- Renal Failure
- Aortic Dissection/Aneurysm
What are some causes of HTN?
- 90-95% of HTN is idiopathic apparently primary (Essential HTN)- don’t know reason why it occurs
-
5-10% : mostly secondary d/t renal disease
- We know what the risk factors are for it (atherosclerosis, stress, pain, life style, smoking, renal, etc) but we don’t actually know what causes it except for organic things like pheochromocytoma
What are some effects of HTN on the heart?
- Hypertension causes increased myocardial wall tension which can lead to:
-
Increased myocardial oxygen demand (need to feed a bigger muscle)
- Leads to coronary insufficiency
- Which can lead to heart failure
-
Left ventricular hypertrophy (which leads to increased o2 demand)
- Which leads to heart failure
- Infarction dysrhythmias can lead to coronary artery insufficiency and heart failure
-
Increased myocardial oxygen demand (need to feed a bigger muscle)

What are types of HTN?
- Systolic and Diastolic
- Essential hypertension – 95%
- Secondary hypertension – 5%
- Renal
- Endocrine
- Cardiovascular
- Neurologic
How is blood pressure normally regulated?
BP= Cardiac Output x Peripheral Resistance
-
Cardiac Output
- Determined by blood volume
- (stroke volume)
- Cardiac factors
- (how well is myocardium functioning → such as HR- frank starling curves)
- CO = SV x HR
- Determined by blood volume
-
Peripheral Resistance
- Humoral Factors (constrictors/dilators)
- Neural Factors (stress response, vagal response)
- Local (released locally, thromboxane vs NO produced)

What is the pathogenesis of essential (primary ) HTN?
Risk factors
-
Genetic
- Polygenic and heterogenous
- Polymorphisms at several gene loci
-
Environmental
- *Stress
- Obesity
- Smoking
- Salt consumption
- Sedentary lifestyle
Pathophys of HTN?
- Increased SNS activity in response to stress
- Overproduction of sodium retaining hormones
- Overproduction of vasoconstrictors
- Underproduction of vasodilators (NO, prostaglandins)
- Increase Na intake
- Inadequate intake of Ca and K
- DM – changes to vasculature that occur
- Obesity- plague formation and vasocontraction that occurs in disease
Effect of sodium retention on BP?
- Salt/Water Retention: The final common pathway in the pathophysiology of essential hypertension
- PROBLEM: BV (going back to pic)
-
TX:
- Sodium restriction lowers BP
- Diuretics - act as effective antihypertensives by promoting sodium excretion/H2O