Canadian Urological Association guideline: Management of ureteral calculi Flashcards
What is the contemporary estimate of the prevalence of nephrolithiasis in men and women globally?
Men: 10–12%
Women: 7–8%
How is renal colic characterized in terms of emergency department (ED) presentations?
It is one of the most frequent and expensive ED presentations.
In a study comparing renal colic management patterns in two Canadian cities, what were the observed admission and surgical intervention rates?
Admission rates: As high as 60%
Surgical intervention rates: Over 50%
How did early intervention for renal colic impact subsequent ED visits, re-admissions, and secondary procedures?
Early intervention led to increased subsequent ED visits, re-admissions, and secondary procedures.
What were the findings regarding costs associated with the management of acute renal colic in terms of non-surgical management?
An initial trial of non-surgical management was associated with lower indirect costs.
What is the primary objective of the Canadian Urological Association (CUA) guideline document on ureteral calculi?
To provide evidence-based consensus recommendations on various aspects relevant to the management of ureteral stones.
List the major topic areas included in the CUA guideline document on the management of ureteral stones.
Conservative management
Medical expulsive therapy
Shockwave lithotripsy (SWL)
Ureteroscopy (URS)
Special clinical scenarios (e.g., pregnancy, pediatrics)
What percentage of symptomatic ureteral stones <4 mm pass spontaneously according to the 2010 meta-analysis?
38–71%
In placebo-controlled RCTs evaluating medical expulsive therapy (MET), what are the spontaneous passage rates for stones <10 mm?
40–80%
What is the recommended approach when faced with a suspected “septic stone”?
Early goal-directed therapy, including blood and urine cultures, broad-spectrum IV antibiotics, resuscitation, and source control. Decompression of obstructed pyelonephritis is critical.
In a prospective trial with patients having a fever >38°C, leukocytosis, and an obstructing stone <15 mm, what were the two methods of decompression compared, and what was the outcome?
Ureteric stent and nephrostomy tube (NT). No differences in clinical outcomes were observed.
After initial treatment for obstructed system decompression and infection treatment, how long is recommended to wait before definitive treatment?
A minimum of seven days.
What percentage of patients with renal colic present with acute kidney injury (AKI)?
Approximately 6%.
According to one RCT, how did early ureteroscopic management compare to delayed intervention in terms of postoperative stenting rates?
Early management led to similar stone-free and complication rates but lower rates of postoperative stenting.
In RCTs comparing early vs. delayed shock wave lithotripsy (SWL), what benefits were observed for early SWL?
Earlier time to stone-free status, fewer required treatments, and possibly lower complications.
What is the general recommendation for managing patients with smaller ureteral stones (<5 mm)?
Many can initially be managed non-operatively due to high spontaneous passage rates, but close follow-up is necessary.
What is the recommended management for obstructive pyelonephritis?
Early goal-directed therapy, with timely decompression in either an antegrade or retrograde fashion, depending on the most expedient method.
What has been the increase in the use of CT scans for diagnosing urolithiasis in the acute setting in recent years?
Over 10-fold.
What percentage of acute urolithiasis diagnoses are performed using CT scans and ultrasonography respectively?
CT scans are used in 90% of the cases, while ultrasonography is used in less than 7%.
How might patient gender affect the initial imaging modality selected for urolithiasis?
There is evidence suggesting that patient gender may impact the initial imaging modality chosen.
Between ultrasonography and non-contrast CT imaging for renal colic presentations in the ED, which is recommended and why?
Ultrasonography is recommended due to the lack of radiation exposure.
What is a drawback of point-of-care ultrasonography (POCUS) compared to ultrasonographies performed by radiologists?
POCUS is more operator-dependent, and consulting teams often don’t have images or a formal report to review.
How does supplementing ultrasonography with KUB X-rays affect the detection of a ureteral stone?
It enhances the sensitivity, with results showing sensitivity ranging from 79–100% and specificity up to 100%.
What advantage does obtaining a KUB X-ray during diagnostic imaging in the ED offer?
It’s useful for determining stone composition and tracking the progress of stone passage in follow-up.
How do reduced-dose NCCT scans perform in terms of sensitivity and specificity?
They maintain sensitivities and specificities from 90–97%.
How does body mass index (BMI) affect the diagnostic accuracy and radiation doses of CT scans when assessing for stones?
BMI has shown to be less of a concern, with >95% diagnostic accuracy and radiation doses <3.7 mGy regardless of BMI.
In the acute setting, what is the added benefit of dual-energy CT scans?
There’s little additional benefit as obstructing stones are not typically treated with dissolution therapy, even though dual-energy CT scans can identify uric acid stone composition.
What factors should be considered when ordering imaging for non-life-threatening indications?
The patient’s age, pregnancy status, stone history, and preceding exposure to ionizing radiation.
What is the CUA’s recommendation for the initial modality of choice for acute ureteral stones?
Ultrasonography with KUB X-ray should be considered the initial modality of choice. Judicious use of CT scans, preferably low-dose, is also valuable for management decisions. The utility of a KUB X-ray at the time of presentation is crucial for future follow-up and decision-making regarding treatment options.
What is the outcome of recent RCTs regarding the use of alpha-blockers for MET in terms of stone passage rates or reduced analgesic requirements?
Recent RCTs failed to show improved stone passage rates or reduced analgesic requirements when using alpha-blockers for MET.
What subgroup of ureteral stones might benefit from MET according to subgroup analysis data?
The benefit might be mainly for larger (5–10 mm), distal ureteral stones.
What did higher-quality, placebo-controlled studies in the Cochrane review indicate about MET?
They showed a benefit with MET, a decrease in hospitalizations, and no significant changes in the need for intervention.
What is the shift in analgesic preference for patients with renal colic?
There’s a move away from opioids towards non-opiate analgesia for these patients.
How did NSAIDs compare to morphine in reducing pain for acute care patients in one study?
NSAIDs were more effective in reducing pain by 50% compared to morphine after 30 minutes, with no adverse events.
What was the outcome of using non-opioid analgesia regarding opioid requirements during initial presentation?
Protocolled non-opioid analgesia could reduce opioid requirements if first- and second-line interventions included NSAIDS and intravenous lidocaine. However, opioid-sparing approaches were associated with higher rates of repeat visits to the ED.
Why should forced IV hydration solely for the purpose of stone passage be avoided?
It’s not supported by the literature and should be avoided.
What does the recommendation state about the role of MET for ureteral stones?
The role of MET in promoting spontaneous passage is controversial. If there’s any benefit, it is for larger (5–10 mm) ureteral (distal) stones. The advantages and disadvantages of MET should be discussed with the patient in a shared decision-making process.
What is the recommendation regarding analgesic regimens for renal colic?
The use of opioid-sparing analgesic regimens has been shown to be efficacious. Opioids for the management of renal colic should be minimized, and patient education is paramount.
What is the recommendation regarding forced IV hydration for stone expulsion?
Forced IV hydration for the purposes of stone expulsion is not recommended.
What percentage of patients reported passage of a symptomatic ureteral stone but still had persistent obstruction on follow-up CT scan imaging?
6.2%
How sensitive and specific was the resolution of pain for successful passage of a ureteral stone based on follow-up US and KUB X-ray imaging?
79.7% sensitive and 55.8% specific
Why is follow-up imaging suggested after reports of successful passage of obstructing ureteral stones?
Because neither resolution of symptoms nor patient reports always confirm the successful passage of obstructing ureteral stones.
How many patients with a persistent ureteral stone confirmed on ultra-low-dose CT lacked hydronephrosis on CT and a visible stone on the CT scout image?
38%
Approximately how long will the majority of patients take to spontaneously pass ureteral stones after presentation?
One month
List factors associated with an increased risk of chronic kidney disease.
List factors associated with an increased risk of chronic kidney disease.
True or False: Resolution of symptoms and patient-reported stone passage always confirm the passage of an obstructing ureteral stone.
False
What is the recommendation regarding the duration of conservative management for a ureteral stone?
The recommended duration of conservative management is unique to each patient, considering multiple factors. Surgical intervention should likely be considered if a patient hasn’t passed an obstructing ureteral stone after 4–6 weeks.
What remains a first-line treatment option for ureteral calculi despite advances in ureteroscopes and laser technologies?
Shockwave lithotripsy (SWL)
True or False: The majority of the data for SWL outcomes comes from patients with ureteric stones.
False. Most data comes from patients with renal calculi.
Which stone location is most similar to renal calculi when considering the shockwave path during SWL?
Upper ureter.
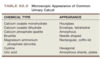
Which stone compositions are most resistant to SWL?
Cystine, pure calcium oxalate monohydrate, and brushite.
What is the significance of uric acid stones in the context of SWL?
While they are fragile in the face of SWL, they require either the use of ultrasound or pyelography (intravenous or retrograde) for targeting during SWL.
How does stone density, measured in Hounsfield units (HU), relate to SWL outcomes?
There’s a linear relationship between increased stone density and poor stone fragmentation. Stones with a density above 1000 HU are less likely to be successfully fragmented.
What novel predictor of SWL success has been reported that may outperform HU?
Variation coefficient of stone density (VCSD).
What has a longer Skin-to-stone distance (SSD) been associated with in the context of SWL?
Reduced treatment success for both renal and ureteral stones.
What SSD value is often associated with decreased stone-free rates (SFRs)?
Greater than 10 cm.
Which stones are likely best treated with URS instead of SWL?
Known uric acid, cystine, and brushite stones.
What characteristics of ureteral stones indicate lower SFRs with SWL?
A density greater than 1000 HU or an SSD greater than 10 cm.
What is the recommendation level for treating uric acid, cystine, and brushite stones with URS?
Level 4, moderate recommendation.
What is the recommendation level for shared decision-making with patients regarding stones with a density greater than 1000 HU or an SSD greater than 10 cm?
Level 2, strong recommendation.
What is the primary composition of brushite stones?
Brushite (calcium monohydrogen phosphate dihydrate).
In what pH range is urine typically when brushite stones form?
Acidic to neutral.
How do the hardness and treatability of brushite stones with SWL compare to most other urinary stones?
Brushite stones are harder and more resistant to treatment with SWL.
Why are brushite stones clinically significant in the realm of urology?
They are harder, leading to challenges in treatment, and patients with brushite stones have a higher rate of stone recurrence.
What medical condition can sometimes be associated with brushite stone formation?
Primary hyperparathyroidism.
What factors in the urine can lead to the formation of brushite stones?
Typically acidic to neutral pH, high urinary supersaturation with respect to calcium and phosphate, and reduced levels of urinary inhibitors like citrate.
Given their characteristics, which treatment modality might be preferred for brushite stones over SWL?
Ureteroscopic management.
What is the primary purpose of gradually increasing SWL energy up to the optimal dose?
Gradual increase in SWL energy allows for better patient accommodation to the sensation of treatment and, for upper ureteral stones, reduces renal injury by inducing renal vasoconstriction.
What is an alternative strategy to dose escalation in SWL?
Pre-treating with a series of low-energy shocks, then pausing treatment for a short period of time before resuming at higher-energy levels.
After how many unsuccessful SWL treatments is the incremental benefit considered small for the same ureteric stone?
The incremental benefit of more than two treatments for the same ureteric stone is small.
What is the unclear optimal time interval between SWL treatments for mid and distal ureteral stones?
2–3 days.
For stones larger than 1 cm, what shock rate has been suggested to improve stone fragmentation?
SWL at 60–90 shocks/minute leads to better fragmentation than 120 shocks/minute.
What is the recommended shock rate range for upper ureteral stones?
The recommended shock rate range is 2000–3500, but manufacturer’s guidelines should be closely considered.
What is the safe shock rate for mid to distal ureteric stones?
For mid to distal ureteric stones, treatment can safely be carried out up to 4000 or more shocks.
What are the recommendations for patients with upper ureteric stones in terms of energy, repetition, shock rate, and number of shocks?
Initially receive low-energy shocks with gradual voltage escalation up to maximum energy.
If unsuccessful, repeat SWL can be considered but more than two treatments to the same ureteric stone has little incremental benefit and URS should then be considered.
For stones >1 cm or those selected for retreatment after initial failed SWL, treat at a rate <120 shocks/minute for optimal fragmentation.
Administer an adequate number of shocks (2000–4000 for most lithotripters) to ensure adequate treatment of ureteric stones. A higher number of shocks may result in improved SFRs, but data is limited for a routine practice recommendation.
What medication class, most commonly represented by tamsulosin, has been studied for its impact on SWL outcomes?
Alpha-blockers.
What are the benefits of alpha-blockers in relation to SWL outcomes based on meta-analyses?
Improved SWL success rates, reduced time to stone passage, decreased risk of steinstrasse, and reduced need for auxiliary procedures.
What did the Cochrane systematic review conclude about routine alpha-blocker therapy concerning SWL?
Routine alpha-blocker therapy may result in improved stone clearance, fewer major adverse events, reduced stone clearance time, less need for auxiliary treatments, and potential benefits related to pain and analgesic use.
Is routine pre-SWL stenting necessary to improve the success rate or passage of fragments?
No, routine pre-SWL stenting is not necessary and does not improve the success rate or passage of fragments.
How might having a stent impact the passage of fragments following SWL?
Having a stent may impede the passage of fragments following SWL.