Burns Flashcards
Incidence statistics for burns?
- 1.25 million burns annually worldwide
- 486,000/year in US required ER visits
- 40,000 hospitalized
- 30,000 admitted to specialized burn center
- incidence of burns has decreased secondary to education on prevention and safety regulations
- survival rate 96.8%
Where they occur
- 73% home
- 8% occupational
- 5% traffic accidence
- 5% recreational sport
- 9% other causes
Etiology of burns?
- Electricla burn 4%
- Chemical burn 3%
- Inhalational burn (burn in a closed space is suspicious for inhalational)
- no percent on chart
- Thermal burn 43%
- (same as flame/fire on pie chart provided)
Mortality of burns?
-
INCREASED MORTALITY
- Older age >60 yo
- >40% TBSA
- inhalational injury
- age of patient + %TBSA burned if > 115, then mortality of patient >80%
- mortality doubled if burn + inhalational injury
- Burn size with LD 50 *lethal dose 50%* >90% TBSA (total body surface area)
- Approx. 3240 die from fire/smoke inhalation injury
- 2855 from residential fires
- 300 motor vehicle/aircraft
- 75% dies at scene or during transport
- 35% burn victims <17 yo
-
Decreased mortality in burns due to:
- increased access emergenyc care
- better airway mgmt
- better infection contorl
- better nutritional support
- early burn excision/grafting
- treatment of hypermetabolic response with EBP
*
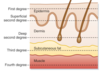
Anatomy of integumentary system
- Largest organ
- layers
- epidermis- protective outer surface
- avascular. nourished by dermis
- dermis
- vascular
- heavily innervated
- collagen and elastic fibers
- deep layer dermis- hair follicles, sebaceous gland. afferent nerve endings
- most nerve terminals at dermis and a few penetrate the epidermis
- deep fascia- deepest layer, dense organized connective tissue layer, seats skin into sq tissue
- subcutaneous
- epidermis- protective outer surface
Function
- protection
- immune function
- fluid/electrolyte homeostasis
- containment
- heat regulation
- sweating/vasomotor regulation of superficial blood flow
- blood vessels dilate in heat, constrict in cold
- sweating/vasomotor regulation of superficial blood flow
- sensation
- vitamin D

Burn categorization?
- Basis: depth and body surface area
- 1st degree- epidermis
- heals spontaneously
- 2nd degree- important to know if basement membrane is intact/not intact
- superficial partial thickness (basement membrane intact)
- if basement membrane intact- skin will generate and grafting not needed
- deep dermal burn (basement membrane not intact)
- need grafting
- superficial partial thickness (basement membrane intact)
- 3rd degree- full thickness burns
- subcutaneous extension
- will need grafting
- 4th degree
- muscle, fascia, bone

What is a first degree burn?
depth? how the wound looks? causes? levelof pain? healing time? scarring?
- Depth- epithelium
- How the wound looks- no blisters; dry, pink
- Causes- sunburn, scald, flash flame
- Level of pain- painful, tender and sore
- Healing time- two to five days; peeling
- Scarring- no scarring, may have discoloration
What is a second degree burn?
depth? how the wound looks? causes? level of pain? healing time? scarring?
- Depth- epithelium and top aspect of dermis
- How it looks- moist, oozing, blisters,
- moist, white, pink to red
- Causes
- scalds
- flash burns
- chemicals
- Level of pain
- very painful
- Healing time
- superficial- five to 21 days- no grafting needed
- deep 21-35 days- needs grafting
- Scarring
- minimal to no scarring
- may have discoloration
Characteristics of third degree burn?
depth? how the wound looks? causes? level of pain? healing time? scarring?
aka full thickness
- Depth- epithelium and dermis
- how it looks-
- leathery, dry
- no elasticity
- charred
- Causes
- contact with flame, hot surface
- hot liquids
- chemical
- electrical
- Level fo pain
- very little pain or no pain
- Healing time
- small areas may take months to heal
- large areas to be grafted
- Scarring present
Summary of burns?
- 1st degree
- involves epidermis
- erythema
- spontaneous healing
- 2nd degree
- superficial burn
- spontaneous healing 7-10 days
- painful
- deep dermal
- requires excision/grafting
- 2-8 weeks to heal
- scarring
- superficial burn
- 3rd degree- complete dermal loss
- no pain d/t nerve damage
- 4th degree- expect to lose limb
- muscle/bone/tnedon involved
What is the rule of nines?
- How we estimate burns
- Head and neck 9% (total)
- Ant 4.5%
- Post 4.5%
- RUE 9%
- Ant 4.5%
- Post 4.5%
- LUE 9%
- Ant 4.5%
- Post 4.5%
- RLE 18%
- Ant- 9%
- Post 9%
- LLE 18%
- Ant- 9%
- Post 9%
- Anterior tunk 18%
- Post trunk 18%
- Perineum 1%

Criteria of major burn?
2nd degree burn >20% TBSA in adult, or 10% in extremes of age
or
3rd degree burn >10% TBSA in adult
or
any electrical burn
or
any burn associated with smoke inhalational
or
any burn involving face, airway, or genitals of any percent
What determines initial resuscitation in burn
TBSA
How is TBSA estimated in children?
- Lund and Browder chart
- not expected to memorize
- Rules of nine inaccurate in children
- head and trunk proportionally larger in children
Pathophysiology of burns?
- 2 distinct phases
- burn/shock phase
- hypermetabolic phase
- SIRS response
- every system affected
- necrotic and ischemic area
- potential viability of ischemic area with adequate resuscitation
- no potential for viability with necrotic area
- Minutes to hours: burned tissues release inflammatory and vasocative mediators
- All lead to increased capillary permeability,
- histamine
- prostaglandin
- kinin
- leukotrienese
- thomboxane
- nitric oxide
- All lead to increased capillary permeability,
- Later
- reperfusion injury
- tissue produces ROS and toxic cell metabolites
- leads to further cell membrane dysfunction
- worsening of immune response, cascade of responses
- reperfusion injury
What should we keep in mind in regards to burn zones?
- Burn
- zone of coagulation- area dead
- zone of stasis
- zone of hyperemia
- with adequate resuscitation, zone of stasis and zone of hyperemia blood flow can be restored and maintain viabiilty
- without adequate resus, the zone of coagulation will grow and zone of stasis will become infarcted and won’t be able to regenerate

Electrical burns?
- Devastating injury to bones, BV, muscle, and nerves
- tissue damage based on voltage and duration
- entry and exit are where most energy (damage) are concentrated
- 10-46% with concurrent cardiac arrhythmias; may have damage to the myocardium
- massive muscle damage leads to renal failure secondary to myoglobinemia (from rhabdo)
Chemical burns?
- Occupational injury
- reaction with tissue proteins and cellular components leads to tissue destruction
- chemical burn: must neutralize; copious irrigation
Thermal burns?
- Scaled inuries account for 70% burns in <4 yo
- >5 yo: flame associated
- burns in young children 15-20% is non-acciedental burn (d/t abuse/neglect)
Symptoms Inhalational injury?
- hoarseness
- sore throat
- dysphagia
- hemoptysis
- tachypnea
- accessory muscle usage
- wheezing
- carbonaceous sputum
- increased CO levles
Types of inhalational burns?
- Most commonly associated with thermal burns
- likely in closed space burn; suspect in pt unconscious at scene
3 types
- 1) Upper airway injuries- inhalation of superheated air/steam
- may spare lower airway d/t reflexive VC closure
- 2) Lower airway/parenchymal
- soot particle/chemical inhalation
- acute phase will have significant bronchopasms
- bronchodilator therapy always required
- may need epi b/c refractory to other treatment
- bronchodilator therapy always required
- 3) metabolic asphyxiation- carbon monoxide, etc.
Pathophys of inhalational injury?
- microvascular changes
- heat denatures proteins, activates complements
- causes release of histamine
- histamine causes release of xanthin oxidase
- enzyme involved in breakdown of purine–> uric acid
- ROS released
- ROS combine with NO–> reactive nitrogen species formed
- causes edema in burned area
- increases microvascular pressure and permeability to protein
- ROS combine with NO–> reactive nitrogen species formed
- release proinflammatory cytokine and oxygen free radical/interleukin
- attract polymorphonuclear cells to area and neutrophils applify release of oxygen radicals, proteases and other materials
- becomes vicious cycle

Consequence of inhalational injury?
- Coagulopathy
- Bronchospasm
- mucus secretion–> airway obstruction
- airway epithelial exfoliation because of neutrophil migration
- increased airway blood flow
- causes airway wall edema
- upregulation of adhesion molecules, ROS, superoxide
- end up with lots of cellular dysfunction, pulmonary edema, V/Q mismatch, loss of hypoxic vasoconstriction
All major burns are going to have change in pulmonary physio even with no direct inhalational injury










