Bronchial Carcinoma Flashcards
When talking about “lung cancer” what does this usually refer to?
it generally refers to a tumour of the bronchus
95% of lung cancers are carcinoma of the bronchus
2% are alveolar tumours
3% are benign or less invasive malignant tumours
What is the prognosis like for bronchial carcinoma?
What is 1 year and 5 year survival like?
prognosis is extremely poor
1 year survival is about 20%
5 year survival is about 5%
these values vary depending on the type of tumour that is present
How common is bronchial carcinoma?
In what groups is the incidence increasing?
it is the most common cancer worldwide
it causes 32,000 deaths in the UK annually with 40,000 new cases each year
incidence is increasing in women, particularly in northern Europe
it causes more deaths in women than any other malignant tumour
What is the male:female ratio in bronchial carcinoma?
What is mortality like in England?
the male to female ratio is 3 : 1
it accounts for 19% of all cancers and 27% of all cancer deaths in the UK
it is the third most common cause of death in the UK, following heart disease and pneumonia
What is the major risk factor for bronchial carcinoma?
SMOKING
it causes 90% of cases
the strength of association between cigarette smoking and bronchial carcinoma overshadows any other aetiological factors
How can place of living influence chance of developing bronchial carcinoma?
What other habit has a large influence?
there is a higher incidence of BC in urban, as opposed to rural areas
passive smoking increases the risk of bronchial carcinoma by 1.5 times
What is the major occupational factor that is linked to bronchial carcinoma?
ASBESTOS EXPOSURE
there are 3 types of asbestos - white, blue and brown
blue is the worst
you are only at risk when the asbestos is broken up as this releases the fibres
this usually causes a specific type of tumour - mesothelioma
What other occupational factors can increase risk of bronchial carcinoma?
What type of tumours usually are these?
- arsenic (in paint, batteries & fertilisers)
- iron oxide
- chromium
- petroleum products
- oil
- radiation / radon
- coal tar and products of coal combustion
tumours associated with occupational factors tend to be adenocarcinomas
What is the relative risk of a non-smoker and a smoker contracting bronchial carcinoma?
How does risk change if someone stops smoking?
- someone who has never smoked has a relative risk of 1%
- a smoker has a relative risk of 43%
- after 10 years of stopping smoking, risk is greatly reduced, but it never reaches that of non-smokers

How are bronchial carcinomas divided?
they are divided based on the characteristics of the disease and its response to treatment
it is divided into small cell carcinoma and non-small cell carcinoma
What are the subcategories of non-small cell carcinoma?
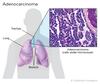
- adenocarcinoma
- squamous cell carcinoma
- large cell carcinoma
What is the development time, survival and common location for small cell carcinoma?
- development time from initial malignant change to presentation is about 3 years
- doubles in 30 days
- survival is around 5%
- common location is around the hilum / central
What is the development time and common location of adenocarcinoma?
- development time from initial malignant change to presentation is 15 years
- doubles every 200 days
- more often found in the periphery
- more likely to present late as it is less likely to cause obstruction symptoms
What is the development time for squamous cell carcinoma?
8 years
What is meant by large cell carcinoma?
Where do they tend to be found?
large cell carcinomas are less differentiated forms of squamous cell carcinoma and adenocarcinoma
they are commonly found more centrally
What % of tumours are in the lobar bronchi?
Tumours in which type of bronchi will present earlier?
80% of tumours are in lobar bronchi - the rest are in larger bronchi
tumours arising in a main bronchus tend to present earlier than those arising in a small bronchus
this is because they cause far greater symptoms at an early stage
How can a squamous cell carcinoma that has cavitated by identified through imaging?
- on X-ray, it tends to have the appearance of an abscess or TB cavity
- on CT, you can clearly see the jagged edge of the cavity and possible infiltration of other structures (such as the pleura)
- the jagged edge seen on CT tells you that it is definitely cancer, and not just an abscess

How common is squamous cell carcinoma and how does it usually present?
it is the most common type of bronchial carcinoma, accounting for 40% of cases
most present as obstructive lesions of the bronchus, leading to infection
it tends to arise more centrally than in the peripheral lung

What % of squamous cell carcinomas will cavitate?
What does this mean?
SCCs will occasionally cavitate - around 10% at presentation
this occurs when the central part of the tumour undergoes necrosis
How can CT be used to tell apart cavities caused by cancer and infection?
How about an abscess?
- cancer is likely to have a thicker wall than a cavity caused by infection
- cavities are more likely to be infective if the cavity has appeared quickly
- a smooth border and the presence of fluid makes it more likely to be an abscess
How does squamous cell carcinoma tend to spread?
local spread is common but widespread metastases tend to occur relatively late
What do the cells look like in squamous cell carcinoma?
the cells are usually well differentiated but occasionally anaplastic
it develops from squamous cells - the flat cells that cover the surface of the airways

What does squamous cell carcinoma usually cause systemically?
HYPERCALCAEMIA
this is either due to bone destruction or production of PTH analogues