Blood Pressure - Physiology and Pathology Flashcards
What is systolic BP?
- heart contracts
What is diastolic BP?
- heart relaxes
How do we calculate mean BP?
- SBP + 2xDBP / 3
- 120/80 mmHg = normal BP
- (120 + 160) / 3 = 93.3 mmHg
What is the blood flow type in arterial and venous blood vessels?
- arterial = pulsatile
- venous = laminar (continuous smooth blood flow)
What can a BP that is too low cause?
- fainting (vaso-vagal attack) over active parasympathetic
- shock (causes tissue acidosis)
What can a BP that is too high cause?
- tissue damage
What are the 2 main factors that contribute to blood pressure?
- cardiac output
- vascular resistance
How do we calculate blood pressure?
- cardiac output x systemic vascular resistance
Where is blood pressure highest in the body?
- at aorta
Why is the compliance and elastic recoil of arteries important for energy in systole?
- stretch and elastic recoil provide potential energy
- useful in maintaining blood flow in diastole
As we age what happens to the compliance and elastic recoil in our blood vessels?
- both reduce
- ⬆️ systolic pressure
How can an increased blood viscosity increase blood pressure?
- increases resistance
Does blood with a high protein count and cell count have a high or low viscosity?
- high viscosity
What does inotropic mean?
- force of contraction
What does preload mean?
- degree of stretch in heart at the end of diastolic
- specifically left ventricular end diastolic pressure
- degree of stretch is proportional to ventricle filling
How do we calculate cardiac output?
- SV x HR
When trying to apply Starlings law clinically, why do we use end diastolic pressure instead of end diastolic volume?
- end diastolic volume is difficult to measure
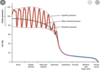
Why does stroke volume plateau in the Starling curves?
- due to heart size
- ventricle can only stretch so much
- only able to pump so much fluid out
In Starlings law the cardiac structure is relatively fixed, however another factor that contributes to cardiac output is preload, why is preload not fixed?
- preload is affected by venous return
- myriad of factors affect preload
What are 2 common causes of a decrease in blood volume that can reduce venous return and therefore preload?
1 - dehydration
2 - major blood loss
How can an over blood transfusion effect cardiac output?
- ⬆️ venous return
- ⬆️ preload
- causes heart to work harder and ⬆️ blood in lungs
How do the 2 sides of the autonomic system affect venous tone and ultimately affect venous return and preload?
- sympathetic ⬆️ venous tone
- para sympathetic ⬇️ venous tone
How does the circulating vasoconstrictors, such as catecholamines of the sympathetic nervous system affect venous tone and ultimately affect venous return and preload?
- adrenalin can ⬆️ venous tone
How can the local vasoactive substance affect venous tone and ultimately affect venous return and preload?
- ⬇️ venous tone due to vasodilation
What are some common vasoactive substances that can act locally?
- nitric oxide
- prostacyclin
- endothelin (most potent vasoconstrictor in the body)
What is blood plasma mainly composed of?
- proteins
- H2O
- salts (Na+, K+, Cl-, HCO3-)
What is aldosterone?
- mineralocorticoid steroid hormone
- produced by the zona glomerulosa of the adrenal cortex in the adrenal gland
How does aldosterone affect blood pressure?
- acts on distal convoluted tubes
- stimulates Na+ retention
- H2O follows Na+
What is anti-diuretic hormone (ADH) and where is it produced and store?
- anti-diuretic
- produced by hypothalamus
- stored and secreted by pituitary gland
- angiotensin II signals its release
What is the role of anti-diuretic hormone (ADH)?
- acts on distal convoluted tubes
- if needs ⬆️ in BP it stimulates H2O retention and thirst
- if needs ⬇️ in BP it stiumulates increased urine passing
- ADH aims to maintain osmolarity
What is the intrinsic control of heart rate?
- sinus node
What is the autonomic control of heart rate?
- sympathetic act on B1 receptors = ⬆️ HR
- para-sympathetic act on M2 receptors = ⬇️ HR

How does a circulating substance such as adrenaline influence HR?
- activation of B1 receptors
- activation of a1 receptors
Roughly what % of blood in the body is fixed in the larger arteries?
- 15%
85% of blood pressure and systemic vascular resistance in the arterioles is controlled by what?
- local and systemic mediators
What is the main role of the renin-angiotensin-aldosterone system (RAAS)?
- regulating blood volume
- regulate systemic vascular resistance
- influence cardiac output
- influence arterial pressure

Does the renin-angiotensin-aldosterone system (RAAS) work locally or systemically to the whole body?
- whole body
What is renin?
- a protease (breaks down protein)
- enzyme that catalyses proteolysis
When is renin released from the kidney?
- when blood flow is low to kidneys
What is the most potent vasoconstrictor in the body?
- endothelin
What is the second most potent vasoconstrictor in the body?
- angiotensin 2
In addition to initiating vasoconstriction, what 2 other functions does angiotensin have?
1 - stimulate aldosterone release from adrenal cortex
2 - stimulates ADH secretion from pituitary gland
How to correctly pronounce renin?
- ree-nuhn
If O2 is low or CO2 is high in the arterioles, what 2 substances can be secreted locally causing dilation in an attempt to increase blood flow and O2?
- nitric oxide
- prostacyclin
What substance is secreted locally at arterioles to initiate vasoconstriction?
- endothelin
In addition to secreting aldosterone, what 2 other catecholamines is the adrenal gland able to produce?
- adrenaline
- noradrenaline
Are the 2 catecholamines (adrenaline and noradrenaline) secreted from the adrenal gland able to initiate an acute or chronic effect on the body?
- acute sustained changes
What alpha and beta receptors to adrenaline and noradrenaline generally act on?
- noradrenaline predominantly an alpha agonist
- adrenaline is an agonist and alpha and beta receptors
What does an agonist of the adrenergic receptors such as adrenaline and noradrenaline do to alpha receptors in relation to systemic arterioles?
- vasoconstriction
- re-directs blood away from unessential organs
- skin and bowels for example
What does an agonist of the adrenergic receptors such as adrenaline do to beta receptors in relation to systemic arterioles?
- vasodilation in skeletal muscles
- ⬆️ blood flow to muscles
What does an agonist of the adrenergic receptors such as adrenaline do to beta receptors in relation to the heart?
- ⬆️ HR
- ⬆️ force of contraction
Where are baroreceptors located?
- aortic arch
- carotid bodies

Which 2 nerves are generally responsible for sending signals to the brain about blood pressure?
- vagus nerve
- glossopharyngeal nerve

What are the 3 control centres in the medualla of the brainstem that act in response to blood pressure requirements?
1 - cardio-accelerator centre
2 - cardio-inhibitor centre
3 - vasomotor centre (peripheral blood vessels)
What is the overall arching aim of the control centres in the medulla of the brainstem, cardio-accelerator centre, cardio-inhibitor centre and vasomotor centre (peripheral blood vessels)?
- integrate sympathetic and parasympathetic responses to blood pressure
What is one of the most common medical cause of high BP?
- chronic kidney disease
What are 2 structural causes in the body that can affect kidney function and thus increase blood pressure?
- renal artery stenosis
- aortic coarctation (narrowing of abdominal aorta)

If a patient has renal artery stenosis or aortic coarctation what will the kidney increase the production of in an attempt to increase blood flow?
- renin
What are some common endocrine causes of high blood pressure?
- ⬆️ aldosterone (retains salts)
- ⬆️ catecholamines (⬆️ HR and BP)
- ⬆️ cortisol (stress hormone)
- ⬆️ growth hormones
What is essential hypertension?
- no specific known cause - majority of people have this
What are some of the factors that contribute to essential hypertension?
- genetics (poly)
- ⬆️ salt intake
- obesity
- ⬆️ alcohol intake
- ethnicity
How does chronic hypertension cause heart failure?
- ⬆️ afterload (SVR)
- heart chronically working heart
What is an aneurysm?
- stretching and rupture of a blood vessel

How can chronic hypertension cause an aortic aneurysm?
- ⬆️ pressure on weakened on blood vessels
- blood vessels compliance may decline with disease and age
- eventually cause rupture
What is a cerebrovascular disease, commonly called a stoke?
1 - ischaemic (narrowing of blood vessels)
2 - ruptute of blood vessels
- both cause a lack of blood to the brain and tissue dies

How can cerebrovascular disease, commonly called a stoke be caused by chronic hypertension?
- ⬆️ narrowing of blood vessels
- ⬆️ risk of becoming blocked or ⬇️ blood flow
How can chronic hypertension cause coronary artery disease?
- ⬆️ pressure damages coronary arteries
- plaque can block coronary arteries
How can chronic hypertension cause peripheral vascular disease?
- ⬆️ pressure damages peripheral arteries
- plaque can build up and block arteries
What are some common problems caused by kidney dysfunction in patients with chronic hypertension?
- brain dysfunction
- exacerbations of other co-morbidities such as eyes, diabetes and peripheral nerves
Severe hypertension can present and can cause damage to tissues. Acute dissection can occur, what is this?
- tear in the aorta
- causes severe chest pain
- often misdiagnosed

Severe hypertension can present and can cause damage tissues. Acute heart failure can occur, what is this?
- ⬆️ resistance placed on heart
- ⬆️ afterload
- heart unable to manage and fails to maintain cardiac output
Severe hypertension can present and can cause damage tissues. Encephalopathy (confusion) and cerebral haemorrhage can occur, what is this?
- swelling on the brain
- may cause a rupture and bleed on the brain
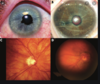
Severe hypertension can present and can cause damage tissues. Retinal haemorrhage can occur, what is this?
- bleeding in the eyes
What is a vaso-vagal episode, also referred to as fainting?
- abnormal response to shock
- parasympathetic system is over activate
- ⬇️ in BP and HR
What does syncope mean?
- black out
Shock can cause a significant reduction in BP that is persistently low, generally <90 mmHg for systolic BP. What are come common causes of this?
- cardiogenic shock (inability to pump blood - MI)
- sepsis
- anaphylaxis
- ⬇️ blood volume (bleeding)
During a shock that causes a significant reduction in BP that is persistently low, generally <90 mmHg for systolic BP what does the sympathetic system do, and what are the consequences of this on other organs/tissues?
- redistributes blood to heart/brain
- other organs become hypoxic
- acidosis
Most circulation in the body receive blood during systole. However, the coronary arteries receive their blood during diastole, how?
- during systole heart compresses coronary arteries
- compressed coronary arteries means no blood flow
- during diastole coronary arteries are able to fill
The lungs have a different response to the general system circulation in response to low O2 and high CO2. What is the normal response to low O2 and high CO2 in the systemic arterioles?
- vasodilation to ⬆️ blood flow
- ⬆️ blood flow brings O2 and removes CO2
The lungs have a different response to the general system circulation in response to low O2 and high CO2. What is the response to low O2 and high CO2 in the pulmonary arterioles?
- vasoconstriction
- minimise blood flow to non perfusing lung tissue
- maximise blood flow to perfusing blood tissue
The lungs are extremely sensitive to vasoactive stimuli in relation to systemic arterioles. What are 2 vasoactive chemicals that are classed as vasoactive?
- endothelin
- prostacyclin


