B5.046 - Pathology of Kidney Glomerular Disease Pt 2 Flashcards
clinical indications for biopsy
nephrotic syndrome
nephritis
asymptomatic hematuria
acute renal failure
chronic renal failure
what is nephritis
hematuria, mild-mod proteinuria, HTN, increased SCr, active urine sediment
RBCs dysmorphic RBC casts in urine

dysmorphic RBCs in nephritic syndrome

RBC casts
what is RPGN
a type of nephritis
characterized by rapid loss of renal fxn, typically 50% loss of GFR within days up to 3 months
may be a/w nephrotic proteinuria
morphologic correlate of RPGN
glomerular crescent formation
3 types of RPGN
type 1 - anti GBM
2 - immune complex GN
3 - anti neutrophil cytoplasmic antibody (ANCA associated)
causes of nephritis
- post infectious glomerulonephritis
- IgA nephrophathy
- lupus nephritis
- membranoproliferative glomerulonephritis
- goodpastures
- ANCA associated glomerulonephritis
- hereditary nephritis (alports)
PIGN features
hypocomplementemia, hematuria, proteinuria, decline in GFR
infxn with GAS is classic
most common in kids/YA
delay in symptoms 1-4 wks, (1-2 wk throat, 3-6 wk skin)
light, IF, EM of PIGN
light - variable, usually diffuse endocapillary hypercellularity, including PMNs; crecents
IF: IgG, C3 (granular, starry sky) GBM pattern; mesangial later in course
EM: subepithelial humps

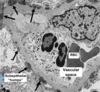
PIGN note the hypercellularity

PIGN, IgG, C3 GBM pattern
PIGN
subepithelial humps
clinical presentation of IgA nephropathy
recurrent hematuris, often associated with simultaneous URI, may progress to chronic renal failure; most common in young white males in US v common among asians
pathology of IgA nephropathy
mesangial expansion/cellular proliferation
immunoflorescence: classically mesangial IgA, C3
EM: mesangial/paramesangial deposits

IgA nephropathy

IgA nephropathy

IgA nephropathy
causes of 2nd degree IgA nephropathy
GI dz: celica, UC, crohns, liver dz
autoimmune: AS, RA, psoriasis, Reiters, behcets
Infx: HIV, TB, campylobacter
neoplastic
HSP presentation
nephritis
rash
arthritis
abdominal pain
most common in children
HSP pathology
glomeruli: mesangial expansion/proliferation, often with necrosis; crescents are common but rarely exceed 50% of gloms; can have endocapillary proliferation
IF: diffuse granular IgA dominant deposits
EM: mesangial, subendothelial deposits
how do you distinguish HSP from IgAN
clinical history required
HS usually has crescents and subendothelial deposits by EM

HSP
crescent, matrix expansion, hypercellularity

HSP




















