Anna - Canadian Board Written Exam 2017 Flashcards
(6 cards)
What is the difference in maxillary and mandibular resorption rates?
Tallgren reported 2.5-3 mm resorption in maxillary anterior ridge height and 9-10 mm in mandibular anterior ridge height over 25 years.
He reported that the pattern of mandibular anterior resorption was 4 times that of the maxilla.
The amount of bone loss of both ridges was significant during the first year following complete tooth loss. Bone loss continued but the amount of change was only about 1/10 of the amount observed during the first year.
Atwood reported, 0.1 mm per year of residual ridge resorption for maxillary anterior ridge and 0.4 mm of RRR for mandibular anterior ridge.
He also observed that RRR in mandible was 4 times greater than in maxilla.
Reference:
1. Tallgren A. The Continuing Reduction of the Residual Alveolar Ridges in Complete Denture
Wearers: A Mixed-Longitudinal Study Covering 25 years. J Prosthet Dent. 1972; 27: 120-32
2. Atwood DA, Coy WA. Clinical Cephalometric and Densitometric Study of Reduction of Residual Ridges. J Prosthet Dent. 1971;26: 280-95
- List the components of PRDP
• Major connector
• Minor connectors
• Rests
• Direct retainers/clasps
• Indirect retainers
• One or more denture bases in conjunction with
prosthetic teeth
Reference:
McCracken’s RPD 13th Edition
How do you attach a wrought wire to a PRDP?
Wrought-wire direct retainer arms may be attached to the restoration
1) by embedding a portion of the wire in a resin denture base,
2) by soldering to the fabricated framework, or
3) by casting the framework to a wire embedded in the wax pattern
Reference:
McCracken’s RPD 13th Edition p.186-187

The physical/mechanical properties of available wrought wires are the most important considerations when a proper wire for the desired method of attachment is selected.
These properties include yield strength, percentage elongation, tensile strength, and fusion temperature. After the wire is selected, the procedures to which the wire is subjected in fabricating the restoration become critical. Improper lab procedures can compromise certain desirable physical properties of the wrought structure. For example, when wrought wire is heated (such as in a cast-to or soldering procedure), its physical properties and microstructure may be considerably altered, depending on temp, heating time, and cooling operation.
Most manufacturers designate wires that may be used in a casting procedure.
Regardless of the method of attaching the wrought wire, tapering the wrought wire seems rational. Tapering to 0.8 mm permits more uniform distribution of service stresses throughout the length of the arm, being readily demonstrated by photoelastic stress analysis.
Round, 18 gauge wrought wire for direct retainer assembly is uniformly tapered to 0.8 mm from its full diameter to its terminus. Tapering should precede contouring of the wire for the retainer arm.
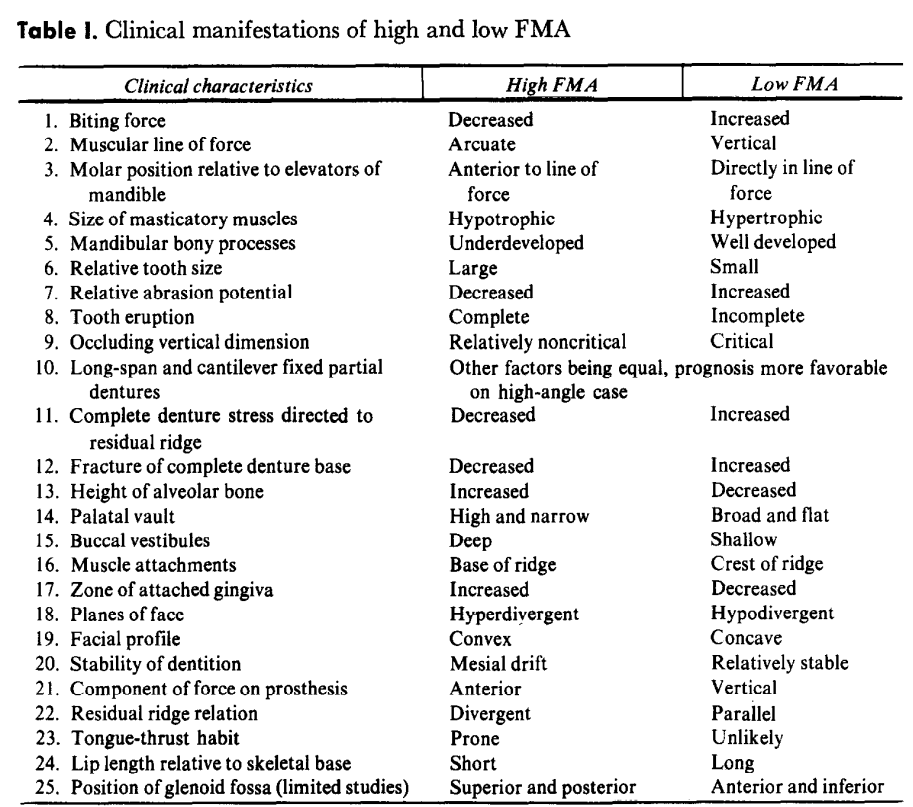
How is the FMA angle used in prosthodontics?
FMA is an angle formed by the intersection of Frankfort horizontal plane and mandibular plane.
A rule of thumb used by orthodontitists is that FMA of 25 +/- 5 degrees is within normal range.
A “high angle” patient is when FMA > 30 degrees. A high FMA is characterized by open-bite skeletal patterns.
A “low angle” patient is when FMA < 20 degrees. A low FMA shows closed-bite skeletal patterns.
<Biting>
A high FMA is associated with decreased biting force and a low FMA with increased biting force.
<Prosthodontic>
Natural teeth - In a low FMA patient, the teeth are infraerupted or intruded. They are more susceptible to abrasion, and the dentition is characterized by small teeth. These factors couple to predispose the patient to a decrease in OVD.
Fixed partial dentures - A low FMA patient has more tendency to return to his former occlusion if OVD is increased during treatment. Increased biting forces in a low FMA patients make the prognosis for long span and cantilever bridges less favorable. These patients require more rigid prostheses. Small teeth and short clinical crowns can cause problems with gaining sufficient retention and require additional internal retention, double abutting, or full coverage. Lack of space can cause difficulties in pontic form and structure as well as in solder joint form and rigidity. Increased abrasion of occluding surfaces of the fixed partial denture is likely.
Complete and removable partial dentures - increased biting forces in low-FMA patients result in more stress to the ridge. The possibility of fracture of the denture base increases, and the occlusal surfaces of the denture teeth wear more rapidly as a result of increase in biting foces. Retention of RPD can be more difficult to achieve because of infraerupted teeth. Determination of OVD is critical. These patients don't tolerate an increase in OVD.
Low FMA patients tend to have flat, broad palatal vaults, shallow buccal vestibules, and high muscle attachments. They also show narrow band of attached gingiva. Thus, stability and retention may become serious problem in low FMA patients. In addition, support is critical in them as a result of increased biting force, and a narrow band of attached gingiva may become a problem in the fabrication and the patient's maintenance of bridges.
A high FMA patient will have less favorable tongue condition than a low FMA patient. According to Sassouni, the pharyngeal space is constricted in a high FMA patient so the tongue tends to thrust and protrude. -> Prosthetically, retention of mandibular dentures may have problem in patients with retracted tongue position. In contrast, patients with tongue thrusting habits may have damage to the teeth or the residual ridge.
Reference:
Di Pietro and Moeregeli. Significance of the FMA to prosthodontics.
https://sci-hub.ru/10.1016/0022-3913(76)90026-3
## Footnote
Look at Lukasz Lassman articles
</Prosthodontic></Biting>
What is pink esthetic score?
PES was first introduced by Furhauser et al. in 2005.
The purpose of PES is to evaluate implant supported restorations and objectify the soft tissue esthetic outcome of different surgical or prosthodontic protocols.
<Variables>
1. 2. Mesial and distal papilla
- shape vs. reference tooth
0: absent
1: incomplete
2: complete
3. Curvature of facial mucosa
- natural, matching reference tooth
0: unnatural
1: fairly natural
2: Natural
4. Level of facial mucosa
- level vs reference tooth
0: major discrepancy >2mm
1: minor discrepancy 1-2 mm
2: no discrepancy <1mm
5. Alveolar process
- alveolar process deficiency
0: obvious
1: slight
3: none
6. 7. Soft tissue color and texture
- vs. reference tooth
0: obvious difference
1: moderate difference
2: no difference
Reference:
Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005 Dec;16(6):639-44. doi: 10.1111/j.1600-0501.2005.01193.x. PMID: 16307569.
https://sci-hub.se/10.1111/j.1600-0501.2005.01193.x
</Variables>
What would make an ideal implant material?


