ANATOMY: RESPIRATORY SYSTEM Flashcards
Identify


Identify

Identify

Identify


Identify


Identify


Identify


Identify


Identify


Identify


Identify


Identify


Identify


Identify
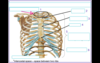

Identify


Identify


Identify

Identify


Identify


Identify

Identify


What are functions of the nasal cavity?
Olfaction
Respiration
Filtration
Humidification
What drains into the meati?
What is the epithelium lining in the nasopharynx?
Pseudostratified ciliated columnar epithelum
What is the epithelium lining in the oropharynx?
nonkerantinized stratified squamous epithelium
What are the characteristics of the nasopharynx?
- Posterior to nasal cavity
- Pharyngeal tonsil on posterior wall
- Auditory tubes open into nasopharynx to equalize air pressure in the middle ear
What are the characteristics of the oropharynx?
- Posterior to oral cavity
- Paired palatine tonsils on lateral walls
- Lingual tonsils on base of tongue (and thus in anterior region of oropharynx)
- Extends between soft palate and the level of the hyoid bone
What are the characteristics of the laryngopharynx?
Extends from level of hyoid bone to beginning of esophagus (posterior to level of croid cartilage in larynx)
Name two mucus membrands of the larynx that form two folds.
- Vestibular fold (false vocal cords). Lined by respiratory epithelium.
- Vocal fold (true vocal cords).

Describe Rima glottidis
The space between the vocal cords
The space below the vestibular fold is called the _________________.
Ventricle
What are the muslces that contract the vocal cords and how do they move?
Contraction of muscles:
- Post cricoarytenoids -moves vocal cords apart-opens rima glottidis
- Lateral cricoarytenoids – moves the vocal folds together-closes the rima glottidis
How is pitch of voice controlled?
Pitch of voice is controlled by the tension on vocal folds.
- Vocal folds pulled taut –high pitched voice
- Decreased tension on vocal folds
– low pitched voice
• Whispering-closing all but the posterior portion of rima glottidis.
What type of cells line the alveolus?
Alveolus lined by simple squamous epithelium (pneumocytes)
What are Type I cells in the aveolus?
Type I & II pneumocytes
- Type I - blood air (gas) barrier along with capillary (extremely thinned out-squamous)
- Type II - produces surfactant
- stem cell (cuboidal- shape)
What are aveolar macrophages?
Alveolar macrophages are dust cells
What is Aveolar Pores of Kohn?
• Alveolar Pores of Kohn – alveoli communicate with each other
What is the inter alveolar septum?
- Inter alveolar septum – elastic and reticular fibers & capillaries
- Elastic fibers help in passive recoiling of lungs
Regarding thoracic aperture, what is the function of the super thoracic opening?
The superior thoracic opening (thoracic inlet) communicates with the neck and upper extremities and is bounded by:
- 1st Body of thoracic vertebra
- 1st pair of ribs and their costal cartilages
- jugular notch of the sternum
Describe the inferior thoracic opening.
The inferior thoracic opening (thoracic outlet) is closed by the diaphragm and is bounded by:
- 12th thoracic vertebra
- 11th and 12th pair of ribs
- Costal cartilages of ribs 7th – 10th
- Xiphisternal joint
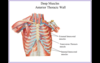
What are the muscles of the thoracic wall?
I. Superficial
• External intercostal muscles
II. Middle
• Internal intercostal muscles
III. Deep
- Innermost intercostal muscles
- Transversus thoracic muscles
What is the direction of the external intercostal muscles?
Direction of the fibers of the external intercostals – medial and
downward (like hands in the front pockets)
Contract synchronously with the diaphragm during normal inhalation.
Increases A-P and lateral diameter.
Describe the diaphragm.
- Closes inferior thoracic aperture – septum between thoracic andabdominal cavity
- Major muscle of respiration
- Innervated by phrenic nerve – C3,4,5
- Multinucleated fibers
* C3,4,5 – keeps the diaphragm alive
What does the thoracic cavity contain?
Thoracic cavity contains:
- Two pulmonary cavities (right and left lung)
- Mediastinum (between pulmonary cavities – all other structures)
What is the pleura?
Pleura is a serous membrane which surrounds the lung (Bursa like fluid bags)
- continuous closed system
- has two layers
- visceral pleura – invests the lungs (adherent to organ)
- parietal pleura – covers the internal surface of thoracic wall (away from organ)
What is the pleural cavity?
Pleural Cavity
• Potential space between visceral and parietal pleura
• Normally contents only a thin film of serous fluid
Pleural recess – is a potential space where two adjacent parietal pleura are in contact (during expiration) and fill with lungs during deep inspiration.
Pleural recess are :
- Costodiaphragamtic
- Costomediastinal
Explain the pleural recess and name them.
Pleural recess – is a potential space where two adjacent parietal pleura are in contact (during expiration) and fill with lungs during deep inspiration.
Pleural recess are :
- Costodiaphragamtic
- Costomediastinal
Describe the relationship between the pulmonary artery and the bronchus at the left vs. right lung hilum
The relation of the pulmonary artery and the bronchus at the left vs. right lung hilum can be remembered with the mnemonic RALS:
Right lung: pulmonary artery is Anterior to the bronchus
Left lung: pulmonary artery is Superior to the bronchus
What are the hila of the lungs? What anatomical structures do they contain?
The hila are the “roots” of the lungs. They contain:
Major bronchi (and associated adventitial bronchial vessels)
Pulmonary veins and arteries, and Hilar lymph nodes
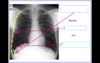
The right lung is composed of which lobes? Which fissures divide these lobes?
The right lung is divided into 3 lobes: upper, middle and lower, which are divided by the horizontal and oblique fissures, respectively.
The right upper lobe lies above costal cartilage 4.
The right middle lobe lies between costal cartilages 4 and 6 in an anterior position.
The right lower lobe lies beneath costal cartilage 6 in a inferior-posterior position. The right lower lobe abuts the diaphragm below.
When a patient is in the sitting or standing position, aspirated material most commonly lodges in the posterobasal segment of the right lower lobe.
When supine, aspiration most commonly localizes to the superior segment of the right lower lobe.

What is a normal FEV1/FVC ratio?
FEV1/FVC is the ratio of the volume of air exhaled in the 1st second of a forceful exhalation to the functional vital capacity. A normal FEV1/FVC ratio is 80%.
In obstructive lung diseases, the FEV1/FVC ratio is typically less than 80%.
In restrictive lung disease, the FEV1/FVC ratio is greater than 80%.
What is the difference between a lung “capacity” and “volume”?
A lung “capacity” is made up of two or more lung “volumes”
ex: Inspiratory Capacity = Tidal Volume + Inspiratory Reserve Volume
Total lung capacity (TLC) = IRV +TV + ERV + RV
- IRV = Inspiratory Reserve Volume
- TV = Tidal Volume
- ERV = Expiratory Reserve Volume
- RV = Residual Volume
Inspiratory capacity (IC) is the maximum amount of air one can inhale after a normal exhalation. It can be calculated with the following equation: IC = IRV + TV
The vital capacity (VC) is the maximum amount of air that one can exhale after a maximum inhalation. It can be calculated with the following equation: VC = TV + IRV + ERV
Vital Capacity is normally between 3-5 L.
The functional residual capacity (FRC) is the volume of gas remaining in the lungs after a normal expiration. It can be calculated with the following equation: FRC= RV + ERV
FRC is normally around 40% of the vital capacity.
What is tidal volume?
Tidal volume is the volume of air inspired (and then expired) during normal respiration.
Inspiratory reserve volume is the volume of air that can be inspired after tidal volume with maximal inspiration.
Residual volume is the volume of air that is left in the lungs after a forceful exhalation.
Expiratory reserve volume is the amount of air that can be forcefully exhaled after normal tidal volume expiration.
Inspiratory capacity is the sum of tidal volume and inspiratory reserve volume (TV+IRV).
Functional reserve capacity is the sum of expiratory reserve volume and residual volume (ERV+RV).
Functional vital capacity is the total sum of expiratory reserve volume, tidal volume, and inspiratory reserve volume (TV+ERV+IRV). It is the maximum amount of air that can be inhaled after completely exhaling forcefully.
Total lung capacity is functional the sum of vital capacity plus residual volume (VC+RV). It is the total lung volume.
related topic: Tests of Pulmonary Function
What areas of the respiratory tract participate in gas exchange?
The alveolar ducts, alveoli, and respiratory bronchioles are part of the respiratory zone and participate in gas exchange.
Type I pneumocytes: long, thin cells with minimal cytoplasm → designed to maximize gas exchange by minimizing diffusion distance. Comprise 90-95% of lung surface area. Poorly replicative.
Type II pneumocytes: cuboidal cells that produce surfactant → maintains airway patency. Comprise 5% of surface area. Contain lamellar bodies containing surfactant. Capable of cell division → produce type I pneumocytes when lung is damaged.
Clinical Correlate
In idiopathic pulmonary fibrosis (IPF), repeated cycles of epithelial injury → abnormal epithelial repair at these sites → fibrosis → reduced diffusion → hypoxemia and hypo or normocapnia.
In a restrictive lung disease, how is inspiration affected? Expiration?
In restrictive lung diseases inspiration is impaired by restriction of lung expansion, andexpiration can be normal or impaired depending on the nature of the restrictive disease.
The following spirometry changes are seen in restrictive lung disease:
- Decreased FEV1
- Decreased FVC (in a roughly equal proportion to the decrease in FEV1)
- Normal or slightly increased FEV1/FVC ratio
- Decreased Residual Volume (RV)
- Decreased Total Lung Capacity (TLC)
Restrictive lung disease can be caused by a compromise in extra pulmonary mechanics, or limited structural expansion of the lungs. As such, restrictive lung diseases can be categorized as either being caused by:
- Disorders of the chest wall, or
- Chronic interstitial/infiltrative causes
Restrictive lung disease caused by a chest wall disorder is characterized by decreasedpulmonary compliance. Disorders of the chest wall that cause restrictive lung disease include:
- Myasthenia gravis
- Scoliosis, which can limit the expansion of the lungs depending on the severity
- Obesity, which can compress the lungs
Restrictive lung disease caused by an interstitial/infiltrative process is characterized by decreased pulmonary compliance and depending on the severity of the disease, decreased diffusion capacity. The following are disease states categorized as insterstial/infiltrative causes of restrictive lung disease:
- Acute Respiratory Distress Syndrome (ARDS)
- Sarcoidosis
- Neonatal Respiratory Distress Syndrome
- Wegener Granulomatosis
- Histiocytosis X Syndrome
- Goodpasture Syndrome
- Asbestosis
- Idiopathic Pulmonary Fibrosis, and
- Iatrogenic causes (Drugs)
Drugs can cause pulmonary toxicity with restrictive characteristics. The following are some commonly implicated drugs:
- Bleomycin
- Busulfan
- Amiodarone
- Methotrexate
- Nitrofurantoin
What histologic feature distinguishes bronchioles from bronchi? What feature marks the end of the bronchioles?
The absence of cartilage distinguishes bronchioles from bronchi.
The bronchioles end distally when the epithelium is no longer ciliated, which marks the start of the alveolar ducts.
Bronchioles also have a prominent layer of smooth muscle.
The bronchioles are lined by ciliated cells that vary in shape from simple columnar in primary bronchioles to simple cuboidal in terminal bronchioles, in addition to Club cells(formerly Clara cells).
Goblet cells are present above the level of the terminal bronchioles, and are responsible for mucous secretion.
Clinical Correlate: In chronic bronchitis there is goblet cell hyperplasia, which causes increased mucus secretion. This results in the obstructive pattern and the characteristic “blue bloater” patient, who cannot get air out of their lungs past thick mucus plugs.
What is the pleura? What is the visceral pleura? The parietal pleura?
The pleura is a thin, transparent, serous membrane enveloping the lungs and lining the thoracic cavity.
Visceral pleura: pleura surrounding all surfaces of the lung, merges with the parietal pleura at the root of the lung.
Parietal pleura: pleura lining the chest wall, diaphragm, and pericardial sac.
Clinical Correlate
Only the parietal pleura receives innervation by general sensory nerve fibers → only inflammation (pleuritis) of the parietal pleura will result in pain. The parietal pleura is innervated by the intercostal nerves and the phrenic nerve → pain referred to chest wall and root of the neck. Visceral pleuritis is clinically silent.

What is the only lung volume that cannot be measured with spirometry? What does this lung volume represent?
Lung volumes (with one exception) are measured with spirometry, and measure the volume of gas entering and leaving the lungs under varying circumstances.
The only lung volume that is not measured with a spirometer is the residual volume (RV), which is the volume of air remaining in the lungs after a maximal (forceful) expiration (~ 20% of the total lung volume).
The expiratory reserve volume (ERV) is the volume of gas that can still be forcefully exhaled after a normal expiration.
The inspiratory reserve volume (IRV) is the volume of gas that can be forcefully inhaled after a normal inspiration.
The tidal volume (TV) is the volume of gas that moves in and out of lungs during typical quiet respiration. The tidal volume is normally around 500 mL.
The RV is increased in obstructive lung diseases.
The RV is decreased in restrictive lung diseases.
The Lung volumes can be remembered with the mnemonic “LITER”:
Inspiratory reserve volume
Tidal volume
Expiratory reserve volume
Residual volume


