Anatomy of the Thorax Flashcards
Describe the right main bronchis
- Shorter
- Wider
- 2.5cm in length
- Passes directly to the root of the lung at T5
- Before joining the hilum, gives off upper lobe bronchus (this is not the case with the left main bronchus)
- It then passes below the pulmonary artery to enter the hilum
Describe the left main bronchis
- Longer
- More oblique
- 5cm in length (hence twice the length of the right main bronchus)
- Passes BELOW the Arch of the Aorta
- Passes IN FRONT of the Oesophagus and descending aorta
- Does not give off left upper lobe bronchus prior to the hilum, unlike the rigth main bronchus
- Reaches hilum at T6 (left at T5)
- Pulmonary artery spirals over left main bronchus: first lying anteriorly, then above it superiorly
Views during bronchoscopy
Can visualise:
- Trachea
- Main bronchi
- Lobar bronchi
- Commencement of 1st segmental divisions
Widening of the Trachea on CXR
Suggests enlargement of tracheobronchial lymph nodes
In the context of malignancy is a poor prognostic marker as lymph node involvement
Origin of bronchial arteries
- Bronchial arteries are branches ofteh descending thoracic aorta
- They are of great clinical importance as they perfuse the lung parenchyma, hence during a PE the lung parenchyma is perfused despite pulmonary vessels being occluded
- Supply each lobe of the lung parenchyma
Drainage of the lung parenchyma
Bronchial veins drian the lung parenchyma
Bronchial veins drian into the azygous vein
Drainages of the lung alveolar spaces
Oxygenated blood drains from the lung via the pulmonary veins
Superior and inferior pulmonary veins on each side
i.e. there are 4 pulmonary veins
Drains oxygenatedblood into theleft atrium
Lymphatic drainage of the lungs
- Lymphatics of the lung drain centrapedally from the pleura to the hilum
- Bronchopulmonary lymph noes in the hilum drain to the tracheobronchial lymph nodes at the carina (enalrhgement causes splaying of the carina)
- Tracheobronchial lymph nodes then drain into the paratracheal lymph nodes
- Paratracheal lymph nodes drain into the mediastinal lymph nodes
- These mediastinal lymph nodes drain directly into the brachiocephalic veins or directly into the thoracic duct / right lymphatic duct
Nerve supply to the lung
Innervation of the lungs is via the pulmonary plexus at the hilum
- converys sympathetic fribres T2 - T5 (T6)
- conveys parasympathetic fibres from the vagus nerve
Constituents of a bronchopulmonary plexus
Consist of:
- A segmental artery
- A segmental vein
- A segmental bronchus
Wedge-shaped
Apices situated at the hilum and base at lung surface
If resected carefully –> little bleeding or air leak from raw surface
Lingular segment
Left upper lobe has lingular segment
(= right middle lobe)
Right upper lobe bronchopulmonary segements
Right upper lobe bronchopulmonary segements
- Apical bronchis
- Posterior bronchus
- Anterior bronchus
Right middle lobe bronchopulmonary segements
Right middle lobe bronchopulmonary segements
- Lateral bronchus
- Medial bronchus
Right lower lobe bronchopulmonary segements
Right lower lobe bronchopulmonary segements
- Apical bronchus
- Medial basal (cardial) bronchus
- Anterior basal bronchus
- Lateral basal bronchus
- Posterior basal bronchus
Right bronchopulmonary segments
Upper
APA
Apical
Posterior
Anterior
Middle
LM
Lateral
Medial
Lower
AMALP
Apical
Medial basal
Anterior basal
Lateral basal
Posterior basal
Left upper lobe bronchopulmonary segments
Left upper lobe bronchopulmonary segments
- Apicoposterior bronchus
- Apicoposterior bronchus
- Anterior bronchus
Left middle lobe bronchopulmonary segments
Left middle lobe bronchopulmonary segments
- Superior bronchus
- Inferior bronchus
Left lower lobe bronchopulmonary segments
Left lower lobe bronchopulmonary segments
- Apical bronchus
7.
- Anterior basal bronchus
- Lateral basal bronchus
- Posterior basal bronchus
Left bronchopulmonary segments
Upper lobe
AA
Apicoposterior bronchus
Anterior bronchus
Lingula / middle
SI
Superior bronchus
Inferior bronchus
Lower lobe
AALP
Apical bronchus
Anterior basal bronchus
Lateral basal bronchus
Posterior basal bronchus
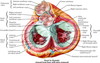
Defining the mediastinum
Cross-sectional midline of the mediastinum defined from the sternal angle anteriorly to the T4 vertebrae posteriorly
Above this is the superior mediastinum
Below this is the inferior mediastinum
The inferior mediastinum is divided into the anterior, middle and posterior divisions
Anterior: in front of fibrous pericardium
Middle: pericardium and great vessels
Posterior: from posterior surface of pericardium to T5 - T12 vertebral bodies
Divisions of the inferior mediastinum
The inferior mediastinum is divided into the anterior, middle and posterior divisions
Anterior: in front of fibrous pericardium
Middle: pericardium and great vessels
Posterior: from posterior surface of pericardium to T5 - T12 vertebral bodies
Fusions of the pericardium
Conical fibrous sace containing the heart and roots of the great vessels
Apex is fused with the adventitia of the great vessels
Base is fused with the central tendon of the diaphragm
Anterior relations of the pericardium
(4)
Body of the sternum
Attached by the sternocardial ligaments
3rd - 6th costal cartilages
Anterior borders of the lungs
Posterior relations of the pericardium
(6)
- Oesophagus
- Descending aorta
- T5 - T8 verebrae
- Roots of the lungs
- Mediastinal pleural
- Phrenic nerve