all Flashcards
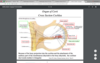
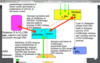
Sensory from a portion of external ear
General Somatic Afferent (GSA) Facial Nerve
Supposed existence carrying information from sublingual and submandibular glands
General Visceral Afferent (GVA)
Inf. Vagal Ganglion
SA and GVA Vagus
Supposed existence carrying information from palatine, pharyngeal
General Visceral Afferent (GVA from CN 7
Taste from the anterior 2/3 of the tongue and palate
SA CN7
Taste from the posterior 1/3 of the tongue
Cranial Nerve IX Glossopharyngeal Nerve
Sensory from a portion of external ear
GSA CN9(GP)
Taste from the epiglottis
SA CN10
GSA and SA fibrs
solitary tract nucleus
facial motor nucleus
CN 7 SVE: motor to muscle of facial expression
SVE: motor to stylopharngeus
CN 9
from nucleus ambiguous
SVE: motor to muscles of palate, pharynx
CN 10
Inf. GP gnaglion
SA and GVA CN9
SVE: motor to muscles of larynx, upper esophagus
CN 10
TF SVE fibers of CN9,10 start from
nucleus ambiguous
spinal tri nucleus
GSA fibers of CN 7 anf CN 9, CN 10 from ext ear
postganglionic parasympathetic fibers innervate thoracic and abdominal viscera
CN 10 GVE
Parasympathetic ganglion cell in the wall of the target organ
GVE of CN 10
Superior Salivatory Nucleus
starts GVE fibers of CN7
Dorsal motor nuc
starts GVE fibers of CN 10
postganglionic parasympathetic fibers to sublingual and submandibular glands
from CN 7 GVE
goes to submandibular gang
postganglionic parasympathetic fibers to lacrimal, nasal palatine and upper pharynx glands
from CN 7 GVE
from Pterygopalatine ganglion
Otic gaglion
GVE fibers of CN 9
parasympathetic fibers(pre and post ganglionic neurons)
postganglionic parasympathetic fibers to parotid gland
GVE fibers of CN 9
solitary nucleus
starts GVE fibers of CN 9
only has GSE
CN 12
hypoglossal
intrinsic tongue ms. • 3 of 4 extrinsic tongue ms.
GSE of CN12
Hypoglossal nucleus
cell bodies for GSE CN12
tf CN12 GSE fibers will
abduct the tongue
F adduct iit
major muscles of int. tongue and ext tongue receive only contralateral input from pre central gyrus
corticobulbar fibes innerve the CN 12 cell body in the hypoglossal nucleus
adduct
toward midline
LMNL of CN 12
tongue to side of lesion
UMNL of coricobulb fibers of CN 12
tongue to contralat of lesion
GVE
PS innerv
The nucleus ambiguus receives —- cortiocobulbar input, with the majority of this input being —–
The nucleus ambiguus receives bilateral cortiocobulbar input, with the majority of this input being contralateral.
CN 9,11
inferior salivatory nucleus receives input from the
hypothalamus.
Glossopharyngeal Nerve(cn11)
dorsal motor nucleus receives input from the
dorsal motor nucleus receives input from the hypothalamus
GVE of CN10
Cranial Nerve XII emerges from the —— and enters into the —— cranial fossa. and exits the posterior cranial fossa through the ——- canal.
Cranial Nerve XII emerges from the brainstem and enters into the posterior cranial fossa. • Cranial Nerve XII exits the posterior cranial fossa through the hypoglossal canal.
Taste receptor cells are also located on the palate and epiglottis.
located in the epithelium not in pappilase
Taste receptor are clustered in taste buds,
which are mainly assoicated with fungiform and circumvallate/vallate papillae
tf Foliate papillae have tons of taste buds in adults.
Foliate papillae have few taste buds in adults.






Taste receptor cells are also located on the palate and epiglottis.
located in the epithelium not in pappilase
tf Foliate papillae have tons of taste buds in adults.
Foliate papillae have few taste buds in adults.
epiglottis
SA from CN 10
posterior 1/3 tongue (including vallate papillae)
SA from CN-IX:
anterior 2/3 tongue, palate
SA from CN-VII:
anterior 2/3 tongue, hard and soft palate
GSA from CN 5
at apical end of taste receptor cell and
extend thru taste pore
microvilli

epiglottis
GVA from CN 10
at apical end of taste receptor cell and
extend thru taste pore
microvilli

tf GVA from CN-IX: ant 1/3 tongue, palatine tonsils,larynx
GVA from CN-IX: posterior 1/3 tongue, palatine tonsils, pharynx
Taste receptor cells are replaced
every 7-10 days
the taste receptor cells release neurotransmitter on afferents
of CN VII, CN IX and CN X
Taste receptor are clustered in taste buds,
which are mainly assoicated with fungiform and circumvallate/vallate papillae
Taste molecule activates the taste receptor cell.
Increase intracellular Ca+2 through voltage gated Ca+2 channels and via release from internal stores.
Depolarizing receptor potential (inside of the taste receptor cell become more positive through several different mechanisms)
Transduction of the signal to the CNS (nucleus solitarius/solitaty nucleus)
Release of transmitter on to peripheral nerve (primary afferent)
Taste molecule activates the taste receptor cell.
- Depolarizing receptor potential (inside of the taste receptor cell become more positive through several different mechanisms)
- Increase intracellular Ca+2 through voltage gated Ca+2 channels and via release from internal stores.
- Release of transmitter on to peripheral nerve (primary afferent)
- Transduction of the signal to the CNS (nucleus solitarius/solitaty nucleus)
Central tegmental tract
carries second order neurons of The taste (SA) pathway (ipsilateral)
tf
when the Taste molecule activates the taste receptor cell. it hyperpolarizes polarizes receptor potential (inside of the taste receptor cell become more negative through several different mechanisms)
Taste molecule activates the taste receptor cell. 2. Depolarizing receptor potential (inside of the taste receptor cell become more positive through several different mechanisms)
Central tegmental tract
carries second order neurons of The taste (SA) pathway (ipsilateral)
voltage gated Ca+2 channels and via release from internal stores
help depol taste receptor cell
by inc intracellular Ca+2
The superior aspect of the nucleus solitarius is also referred to
The superior aspect of the nucleus solitarius is also referred to as the gustatory nucleus
Transduction of the signal to the CNS
from taster receptor cell
insula and the medial surface of the frontal operculum
gustatory cortex
The taste (SA) pathway follows
ips. course
the taste receptor cells release neurotransmitter on afferents
of CN VII, CN IX and CN X
near the base of the central sulcus.
gust cortex
Opercula (singular, operculum):
the regions of frontal, parietal and temporal lobes located adjacent to the lateral sulcus and overlying the insula

—– of olfactory receptor cells extend to the surface of the olfactory epithelium and terminate with a ——–region from which non-motile cilia project.
Dendrites of olfactory receptor cells extend to the surface of the olfactory epithelium and terminate with a rounded knoblike-region from which non-motile cilia project.
Cilia
extend into the mucus layer and possess receptors for odorant molecules
Taste information is also relayed from the solitary nucleus to retic. formation to regulate
salivation and swallowing
Cilia
extend into the mucus layer and possess receptors for odorant molecules

—– of olfactory receptor cells extend to the surface of the olfactory epithelium and terminate with a ——–region from which non-motile cilia project.
Dendrites of olfactory receptor cells extend to the surface of the olfactory epithelium and terminate with a rounded knoblike-region from which non-motile cilia project.


CN 1 SA
smell
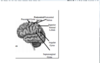
place where the olfactory axons synapse After passing through the cribiform plate
Receptors responsive to different odorant molecules are —– in the olfactory epithelium
Receptors responsive to different odorant molecules are intermingled in the olfactory epithelium

CN 1
The only sensory system with no —– relay to the thalamus, though olfactory information will eventually be —–through the thalamus.
The only sensory system with no precortical relay to the thalamus, though olfactory information will eventually be processed through the thalamus.
Receptors responsive to different odorant molecules are —– in the olfactory epithelium
Receptors responsive to different odorant molecules are intermingled in the olfactory epithelium

At the level of the glomeruli, the axons of olfactory neurons carrying — olfactory information synapse in the — glomerulus.
©At the level of the glomeruli, the axons of olfactory neurons carrying similar olfactory information synapse in the same glomerulus.

place where the olfactory axons synapse After passing through the cribiform plate
At the level of the glomeruli, the axons of olfactory neurons carrying — olfactory information synapse in the — glomerulus.
©At the level of the glomeruli, the axons of olfactory neurons carrying similar olfactory information synapse in the same glomerulus.

The olfactory epithelium is a —– columnar
The olfactory epithelium is a pseudostratified columnar
Neurons in the anterior olfactory nucleus cross via the —– commissure, to the —— olfactory bulb
Neurons in the anterior olfactory nucleus cross via the anterior commissure, to the contralateral olfactory bulb
what type of glands are in CN 1 olf ep.
Mucous producing glands are also present (Bowman’s glands)
Neurons in the anterior olfactory nucleus cross via the —– commissure, to the —— olfactory bulb
Neurons in the anterior olfactory nucleus cross via the anterior commissure, to the contralateral olfactory bulb

tf taste receptor cells are neurons
F
olf receptor cells are neurons tho
The relay through the thalamus occurs after afferents reach the —– —– —– but prior to olfactory info traveling to association cortex (eg. —–)
The relay through the thalamus occurs after afferents reach the primary olfactory cortex but prior to olfactory info traveling to association cortex (eg. orbitofrontal cortex
Convergence in the orbitofrontal cortex,
from the gustatory, somatosensory, olfactory and visual cortical areas
Olfactory receptor cells
replaced every 1-2 months by basal cells in the olfactory epithelium
Convergence in the orbitofrontal cortex,
from the gustatory, somatosensory, olfactory and visual cortical areas

The relay through the thalamus occurs after afferents reach the —– —– —– but prior to olfactory info traveling to association cortex (eg. —–)
The relay through the thalamus occurs after afferents reach the primary olfactory cortex but prior to olfactory info traveling to association cortex (eg. orbitofrontal cortex

olfactory epithelium
olfactory receptor cells/neurons, basal cells and support cells
The taste (SA) pathway follows
ips. course
olfactory epithelium
olfactory receptor cells/neurons, basal cells and support cells
Olfactory receptor cells
replaced every 1-2 months by basal cells in the olfactory epithelium
Unmyelinated axons of olfactory receptor cells to
olfactory filia to olfactory nerve
Unmyelinated axons of olfactory receptor cells
pass through the lamina propria
Unmyelinated axons of olfactory receptor cells travel through the —— —–(ethmoid bone) and terminate in the —–
Theses axons travel through the cribiform plate (ethmoid bone) and terminate in the olfactory bulb.
cribiform plate
ethmoid bone
tf CN1 will emerge thru ant cranial fossa
T thru cribiform plate
tf taste receptor cells are neurons
F
olf receptor cells are neurons tho
tf CN1 will emerge thru ant cranial fossa
T thru cribiform plate
Glomeruli respond selectively to — —– that characterize the complex odor.
Glomeruli respond selectively to one or two molecules that characterize the complex odor.
tf Odor information is carried along the olfactory tract (axons of mitral and tufted cells) to one areas
Odor information is carried along the olfactory tract (axons of mitral and tufted cells) to several areas
cribiform plate
ethmoid bone
Mitral Cells and tufted cells
also contribute to the glomerulus)
Primary olfactory cortex
(piriform cortex, periamygdaloid cortex, anterior parahippocampal gyrus)
which of follwowing areas is not where Olfactory tract fibers terminate
Anterior olfactory nucleus
post olfactory nucleus
Olfactory tubercle
Amygdala
olf. bulb
post olfactory nucleus
and olf bulb
tf Odor information is carried along the olfactory tract (axons of mitral and tufted cells) to one areas
Odor information is carried along the olfactory tract (axons of mitral and tufted cells) to several areas
ability to discriminate and identify odors
Primary Olfactory Cortex
Primary Olfactory Cortex
is located in the uncus of the temporal lobe
Anterior parahippocampal gyrus
Primary Olfactory Cortex
which of follwowing areas is not where Olfactory tract fibers terminate
Anterior olfactory nucleus
post olfactory nucleus
Olfactory tubercle
Amygdala
olf. bulb
post olfactory nucleus
and olf bulb
Anterior parahippocampal gyrus
Primary Olfactory Cortex
perception of flavor
integration in orbitofrontal cortex
Taste-responsive cells of primate amygdala and hypothalamus
complex tastemediated behaviors
Hippocampus –
concerned with learning associated with feeding
projections from prim olfactory cortex
concerned with feeding behaviors
Hypothalamus
(has projections from primary olfactory cortex)
Bilateral lesions in the ventral medial hypothalamus
voracious appetite and resulting obesity
Bilateral lesions of the ventral lateral hypothalamus
failing to feed and wasting
Primary Olfactory Cortex
is located in the uncus of the temporal lobe
Bilateral lesions of the ventral lateral hypothalamus
failing to feed and wasting
Bilateral lesions in the ventral medial hypothalamus
voracious appetite and resulting obesity
concerned with feeding behaviors
Hypothalamus
(has projections from primary olfactory cortex)
Hippocampus –
concerned with learning associated with feeding
projections from prim olfactory cortex
Taste-responsive cells of primate amygdala and hypothalamus
complex tastemediated behaviors
perception of flavor
integration in orbitofrontal cortex
ability to discriminate and identify odors
Primary Olfactory Cortex
Primary olfactory cortex
(piriform cortex, periamygdaloid cortex, anterior parahippocampal gyrus)
Mitral Cells and tufted cells
also contribute to the glomerulus)
Glomeruli respond selectively to — —– that characterize the complex odor.
Glomeruli respond selectively to one or two molecules that characterize the complex odor.
Unmyelinated axons of olfactory receptor cells travel through the —— —–(ethmoid bone) and terminate in the —–
Theses axons travel through the cribiform plate (ethmoid bone) and terminate in the olfactory bulb.
Unmyelinated axons of olfactory receptor cells
pass through the lamina propria
Unmyelinated axons of olfactory receptor cells to
olfactory filia to olfactory nerve
what type of glands are in CN 1 olf ep.
Mucous producing glands are also present (Bowman’s glands)
The olfactory epithelium is a —– columnar
The olfactory epithelium is a pseudostratified columnar
CN 1
The only sensory system with no —– relay to the thalamus, though olfactory information will eventually be —–through the thalamus.
The only sensory system with no precortical relay to the thalamus, though olfactory information will eventually be processed through the thalamus.
CN 1 SA
smell
Taste information is also relayed from the solitary nucleus to retic. formation to regulate
salivation and swallowing
Opercula (singular, operculum):
the regions of frontal, parietal and temporal lobes located adjacent to the lateral sulcus and overlying the insula
near the base of the central sulcus.
gust cortex
insula and the medial surface of the frontal operculum
gustatory cortex
Transduction of the signal to the CNS
from taster receptor cell
The superior aspect of the nucleus solitarius is also referred to
The superior aspect of the nucleus solitarius is also referred to as the gustatory nucleus
voltage gated Ca+2 channels and via release from internal stores
help depol taste receptor cell
by inc intracellular Ca+2
tf
when the Taste molecule activates the taste receptor cell. it hyperpolarizes polarizes receptor potential (inside of the taste receptor cell become more negative through several different mechanisms)
Taste molecule activates the taste receptor cell. 2. Depolarizing receptor potential (inside of the taste receptor cell become more positive through several different mechanisms)
Taste molecule activates the taste receptor cell.
Increase intracellular Ca+2 through voltage gated Ca+2 channels and via release from internal stores.
Depolarizing receptor potential (inside of the taste receptor cell become more positive through several different mechanisms)
Transduction of the signal to the CNS (nucleus solitarius/solitaty nucleus)
Release of transmitter on to peripheral nerve (primary afferent)
Taste molecule activates the taste receptor cell.
- Depolarizing receptor potential (inside of the taste receptor cell become more positive through several different mechanisms)
- Increase intracellular Ca+2 through voltage gated Ca+2 channels and via release from internal stores.
- Release of transmitter on to peripheral nerve (primary afferent)
- Transduction of the signal to the CNS (nucleus solitarius/solitaty nucleus)
Taste receptor cells are replaced
every 7-10 days
tf GVA from CN-IX: ant 1/3 tongue, palatine tonsils,larynx
GVA from CN-IX: posterior 1/3 tongue, palatine tonsils, pharynx
epiglottis
GVA from CN 10
anterior 2/3 tongue, hard and soft palate
GSA from CN 5
anterior 2/3 tongue, palate
SA from CN-VII:
posterior 1/3 tongue (including vallate papillae)
SA from CN-IX:
epiglottis
SA from CN 10
The optic nerve is formed by — — — axons
The optic nerve is formed by retinal ganglion cell axons
Light travels through the pupil to the back of the eye where the —- is
Light travels through the pupil to the back of the eye where the retina
bipolar, horizontal & amacrine cells
Inner Nuclear Layer
tf INL is b/n IPL amd OPL
T
Ganglion cell axons
form optic n.
metabolically supports photoreceptors - absorbs stray light particles
RPE
cell bodies of rods and cones
Outer Nuclear Layer




anatomical and physiologic properties
group ganglion cells
M (or Y) ganglion cells
largest of the ganglion cells
extensive dendritic arbors and large receptive fields
M (or Y) ganglion cells
M or Y ganglion cells are predominantly found in the —– of the retina and mainly receive input from —
M or Y ganglion cells are predominantly found in the periphery of the retina and mainly receive input from rods
P (or X ) ganglion cells
central retina
The optic nerve exits the orbit, traverses the —– canal and emerges into the —- cranial fossa
The optic nerve exits the orbit, traverses the optic canal and emerges into the middle cranial fossa
Optic Nerves
(axons of retinal ganglion cells)
input from cones
P (or X ) ganglion cells
P (or X ) ganglion cells
smaller gang cells
small dendritic arbors and small receptive fields
smaller, P (or X ) ganglion cells
variety of receptive field sizes and physiologic responses.
W cells (gang cells)
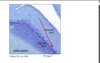
Area of overlap of the two visual fields (purple)
binocular vision

partial crossing
visual information from the left visual field is conveyed in the right optic tract

goes to left temporal eye
nasal right visual field
goes 2 R temporal eye
Left nasal visual field
LGN to V1
optic radiation
tf optic chiasm to only lateral geniculate nucleus (LGN)
f also goes to superior colliculus and pretectum
right visual fields
use the left LGN
Left optic ract
used by right visual field
Area 17
Primary Visual Cortex
6 layers
LGN
large cells;
eceive information about movement and contrast from M-cells
Magnocellular layers
1 and 2 of LGN
•Magnocellular layers
Parvocellular layers
small cells;
receive information about form and color from P-cell
3-6 of LGN
Parvocellular layers
Optic tract fibers are segregated by eye in the
LGN
— LGN layers receive fibers from the —— eye and — layers receive fibers from the —— eye
Three LGN layers receive fibers from the contralateral eye and 3 layers receive fibers from the ipsilateral eye
the upper visual field contribute to the —- optic radiations, and terminate in the —- aspect of V1
the upper visual field contribute to the inferior optic radiations, and terminate in the inferior aspect of V1
calvarian fissure
separates upper and lower visual field of V1
ant; post in primary visual cortex
Peripheral vision; Central vision
expanded cortical representation
Central vision
goes through macula
and has expanded cortical representation
Central vision
most area 17 neurons have a preference for input
from one eye)(monocular)
Axons from LGN course to the primary visual cortex (area 17) and synapse on
layer IV neurons.


monocular; binocular
Layer IV neurons; Layer II/III, V and VI neurons
simple and complex cell
area 17
orientation of a line.
simple cell
may be direction sensitive or respond best to a corner, cross or x.
Complex cells
Cell column that prefer the same line orientation
Orientation Column
Cell clusters that respond to color
Color-Sensitive Region
wavelength sensitive
Color-Sensitive Region
Cell column that respond to input from either the R or L eye OR in the case of binocular cell, have a strong preference for the R or L eye
Ø Ocular Dominance Column
Hypercolumn
refer to a set of orientation and ocular dominance columns that receive input from a given point in the visual field
Primary visual cortex
projects to extrastriate visual areas where neurons require complex stimuli for maximal activation
Primary visual cortex respond to
fundamental aspect of a visual stimulus (orientation, contrast, motion, color, eye of origin)
Dorsal (“M”) Stream
where
perception of motion
posterior parietal association cortex
(from Dorsal (“M”) Stream)
visual information travels to the inferior temporal association cortex
Ventral (“P”) Stream
Ventral (“P”) Stream
what
size, shape, color, orientation
inferior temporal association cortex
(Ventral (“P”) Stream)
inferior temporal cortex
Lesion to V4
Lesion to V1
Scotoma (bind spot)
Lesion to V5
parietal pathway
tf from the pretectal nucleus travel bilaterally to Edinger-Westphal Nucleus
in Pupillary Light Reflex
t

TF in the Pupillary Light Reflex the Temporal optic fibers innervate ipsilateral pretectal area
T

achromatopsia
color recognition
(Lesion to V4 à inferior temporal cortex)
object recognition
(agnosia)
(• Lesion to V4)
face recognition
prosapagnosia
(fusiform face area)
(Lesion to V4)
Projections to the superior colliculus play a role in
visual orientating reflexes
head to visual stimuli
Tectospinal Tract
Tectospinal Tract
contralat
sphincter pupillae
innervated by Postganglionic parasympathetic fibers
Your patient presents with blindness in the right eye. Where is the lesion?
right retina or right optic nerve

bitemporal hemianopia/hemianopsia
Hemianopia/hemianopsia - loss of half of a visual field. Bitemporal hemianopia means that there is loss of vision in both the right and left temporal visual fields

Preganglionic parasympathetic fibers (travel with CN III)
to ciliary ganglion
Edinger-Westphal Nucleus
Pupillary Light Reflex
right homonymous hemianopsia
Lesion to the left optic tract Lesion to the left LGN Lesion to the left optic radiations Complete lesion to the left primary visual cortex (area 17, V1)

papillary light reflex, you shine a light in your patient’s right eye. You note that the right pupil constricts, but the left pupil remains unchanged.
left Edinger Westphal nucleus
left CN-III
left ciliary ganglion

Ø Pretectal area bilaterally innervates
Edinger-Westphal nucleus (EWN)
Pupillary Light Reflex
Fibers from EWN travel to the ipsilateral ciliary ganglion via
CN 3
Pupillary Light Reflex
short ciliary nerves
Fibers from the ciliary ganglion travel to the ipsilateral eye
Pupillary Light Reflex
pupillary constrictor
Pupillary Light Reflex
direct pupillary light reflex
Illuminated eye—
—consensual pupillary light reflex
ØNon-illuminated eye
Light directed to either eye causes
bilateral constriction of the pupils
in Pupillary Light Reflex
Damage to the midline fibers of the optic chiasm may be caused by a
pituitary tumor.
right homonymous hemianopia means that there is
loss of vision in the right visual field
Vestibular Division on CN 8
Responds to movement of the head and the position of the head
Responds to sound
Cochlear Division of CN 8
The inner ear structures are embedded within the
temporal bone
bony labyrinth and membranous labyrinth
inner ear structures
hair cells
membranous labyrinth
correct The bone labyrinth follows most of the contours of the membranous labyrinth
The membranous labyrinth follows most of the contours of the bony labyrinth
Consists of interconnected bony cavities and filled with perilymph
Bony Labyrinth
perilymph
high na
low in K
membranous ducts within the bony labyrinth
Membranous Labyrinth
endolymph
(low in Na+ , high in K+ )
endolymph
Membranous Labyrinth
eventually reabsorbed
endolymph
made by specialized cells in several locations in the membranous labyrinth.
endolymph
leaves through a duct, to reach a sac to get to venous systme
endolymph
[vertigo, nausea, hearing loss, ringing in the ears
obstruction of endolymph flow
rank from ant to post
Vestibule:
Semicircular Canals: 3 on each side: )
Ampullae
vestibule ampullla semicircular canal

central enlarged region of bony labrynth
vestibule
dilation at one end of the each semicircular canals
ampulla
function in complimentary pairing
L post+ r ant
left horizontal and r. horizontal
function in complimentary paring
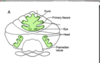
Saccule:
Oriented vertically
located in the bony vestibule
utricule sacule

Oriented horizontally (when upright)
Utricle:
linear (horizontal) acceleration
Utricle
Detect angular acceleration
Activated with most head movements
Semicircular canals
Detects linear (vertical) acceleration (example?)
saccule
static head position
utricle saccule
Adjacent to the tallest stereocilia
the single kinocilium (
project into endolymphatic interior of the membranous labyrinth
stereocilia
endolymph
surrrounds stereocilia
High intracellular K+ opens
voltage gated Ca+2 channels
Neurotransmitter is released (glutamate)

glutamate trigger and triggering CN 8 by
steeocilia
moveing toward highest stereocilia
Opens the mechanically gated K+ ion channels •
K+ enters the cell •
cupula
gelatinous mass hair cells are embedded in

tf cupula only half ways across wall of ampulla
f entire way through ampulla wall

neutral position of stereocilia
gate partially open
Bending of the stereocilia toward the utricle (—–l canals) activates CN—-axons
Bending of the stereocilia toward the utricle (horizontal canals) activates CN-VIII axons
angular acceleration

in ampulla , located within cristae
hair cells
hair cells supporting cells
crista
moving head to right
will make stereocilia move to Kinocilium on the right b/c endolymph moves to left

constant ang velocity when head is moving right
endolymph will stay in that direction and activate stereocilia in the other side of the head
when initial angular accel occurs; channels open on the side of hed turn because endolymp in opposit direction of head turn
when on the deceleration the direction changes and points toward Kinocilium on other side of head because it is now traveling indirection of head turn

angular accelration
relative difference in movement between head and the endolymph; endolymp pushes against cupula
bending its hair cells
left rotation
left left horizontal semicircular canal excited
Increase contraction of the L medial rectus and R lateral rectus

Kinocilium of hair cells are oriented —— utricle in the horizontal canals the (opposite in anterior and posterior canals)
Kinocilium of hair cells are oriented toward utricle in the horizontal canals the (opposite in anterior and posterior canals)
if head moves to right then
endolymph move to left in Semicircular Canals
inc firing in right semicirculat canals
Angular acc.
Allow fixation on an object even though the head is moving
Vestibulo-ocular Reflex
eyes move the direction opposite of the rotation)
Vestibulo ocular reflex
connections between the vestibular nucleus
and CN III, IV and VI in Vestibulo-ocular Reflex
decrease contraction of the L lateral rectus and R medial rectus
With L rotation of head
Oriented horizontally when upright
utricle
Oriented vertically when upright
sacule
forward - back motions [eg. car] and side-to-side
linear (horizontal) acceleration
by urticle
elevator)
Detects linear (vertical) acceleration
by saccule
Provides information about static head position
saccule and utricle
maculae(Hair cells (vestibular receptor cells)) on
utricle and saccule
within the membranous labyrinth
hair cells and supporting cells
maculae of utricle and saccule
embather in otolithic membrane and bathed in endolymph
hair cells of the macula
(utricle and saccule)
carbonate crystals called otoconia or otoliths
make the otoconial membrane denser than the endolymph
moves with even subtle head movements
otolithic membrane
Linear movements
induces movement of the otolithic membrane
Input to CNS via cranial nerve VIII
Bending of the stereocilia toward the kinocilium
causes depolarization and an increase in firing
in utricle and saccule
Hair cells are aligned within the macula
along the striola
(utricle and saccule)
within internal auditory meatus
Vestibular Ganglion
Superior, Inferior, Medial and Lateral Vestibular Nuclei
bilaterally to Medial (neck) and Lateral Vestibulospinal Tract(SC)
Vestibular Nuclei and their Efferents
bilat to To other cranial nerve nuclei
Superior, Inferior, Medial and Lateral Vestibular Nuclei
Vestibular Nuclei and their Efferents
Superior, Inferior, Medial and Lateral Vestibular Nuclei
ips to cerebellum
Vestibular Nuclei and their Efferents
Vestibulo ThalamoCortical Pathway
lateral and superior vestibular nuclei project to the VPL
from the thalamus,
the vestibular neurons project to parietal cortex
Vestibulo ThalamoCortical Pathway
Cochlear Division of CN 8
responds to sounds
Vestibular Division of CN 8
Responds to position and movement of the head
auricle and external auditory canal
Structure and Function External Ear

conducts sound to the tympanic membrane.
ext ear
medial boundary of the external ear
tympanic membrane
Lateral border of middle ear
tympanic membrane
Medial border of middle ear
oval & round windows
petrous part of the temporal bone
malleus, incus, stapes
Bones of middle ear
tensor tympani, stapedius
muscles of middle ear
Sound induced ——— of the tympanic membrane are transferred along a chain of 3 small bones (——-) to the —–window
Middle ear
Sound induced vibrations of the tympanic membrane are transferred along a chain of 3 small bones (ossicles) to the oval window
attached to tympanic membrane; attached to oval window
malleus vs. stapes
types of joints between ossicle bones
synovial joints
tf tensor tympani
increases the vibration of tympanic membrane via attachment to the incus(CN -V)
Middle Ear
tensor tympani
decreases the vibration of tympanic membrane via attachment to the malleus (CN -V)
Stapedius
increases the vibration of the stapes via attachment to the malleus
Stapedius
decreases the vibration of the stapes via attachment to the stapes
protect the ear from excessive vibration
tensor tympani and stapedius
area of the tympanic membrane is — greater than the stapes attachment at the oval window.
area of the tympanic membrane is 15x greater than the stapes attachment at the oval window.
attached at oval window
stapes
differences magnifies the ——- per unit —– of the stapes at the oval window, which is sufficient to move —— within the cochlea.
differences magnifies the force per unit area of the stapes at the oval window, which is sufficient to move perilymph within the cochlea.
The perilymph within the cochlea moves from the —- window toward the—-window, in the bony cochlea.
The perilymph within the cochlea moves from the oval window toward the round window, in the bony cochlea.
membranous component of the cochlea
auditory receptor cells
deformed by Perilymph movement
organ of corti.
auditory receptor cells
cochlea
cochlear duct
Membranous Cochlea
has endolymph
Membranous Cochlea
Filled with perilymph
Bony Cochlea
Consists of interconnected bony cavities
Bony Cochlea
(high in Na + , low in K + ); (low in Na + , high in K + )
perilymph; endolymph
label the blanks

location of the auditory receptor cells … Hair Cells
Membranous Cochlea

Movement of the stapes deflects the membrane at the oval window
Perilymph movement deforms the membranous cochlea duct which contains the organ of corti with its auditory hair cells
This causes displacement of the perilymph within the bony cochlea
Movement of the stapes deflects the membrane at the oval window
This causes displacement of the perilymph within the bony cochlea
Perilymph movement deforms the membranous cochlea duct which contains the organ of corti with its auditory hair cells
scala media
cochlear duct
tf cochlear duct is square
f
triangular
tips of the stereocilia are embedded in the —– membrane (outer hair cells)
tips of the stereocilia are embedded in the tectorial membrane (outer hair cells)
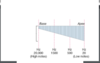
cochlear apex
Relatively flexible , low notes
Movement of the —— membrane influences movement of the —— and thus, impacts ——- release
Movement of the basilar membrane influences movement of the sterocilia and thus, impacts neurotransmitter (NT) releas
release of — will excites CN —–
release of NT will excites CN-VIII
(occurs from basilar membrane when stereocilia is moved )
cochlear base
high notes
Stiff
“Tonotopically” organized.
Basilar Membrane
number of nerve fibers responding
frequency of neuronal firing
Coding of Intensity of the sound
(decibals)
location of sound
Coded within the CNS
CNS compares the timing of sounds reaching the two ears
Auditory Pathway
majoraity fibers cross to contralateral superior olive
cochlear nerve
goes to spiral ganglion and then to cochlear nucleus
Superior olive is important in localization of sound
via the timing and intensity of input
lat lemiscus
path through which fibers cross to inf colliculus in auditory path
Medial Geniculate Nucleus
last nucelus in audiotry pathway before goin to area 41
auditory pathway crosings
trapezoid bodies
inferior colliculus,
medial geniculate nucleus
and cerebral cortex
The trapezoid body (the ventral acoustic stria) is
part of the auditory pathway where some of the axons coming from the cochlear nucleus(specifically, the anterior cochlear nucleus) decussate (cross over) to the other side before traveling on to the superior olivary nucleus
Auditory Cortex
(41/42)
antiobiotic
destroy hair cells(ototoxic effects)
tf Cerebellum give rise to descending motor pathways.
Cerebellum does not give rise to descending motor pathways. Ø
tf Damage to the cerebellum or its pathways DOES cause paralysis
Damage to the cerebellum or its pathways DOES NOT cause paralysis
Input to cerebellum is
sensory
Output of cerebllum
travels to motor structures
rate, range, direction or accuracy of motor movements.
is disturbed by damage to the cerebellum
cerebellum
modulates motor output
in addition to motor output cerebllum
modulates complex behavioral and cognitive functions
receives and processes vestibular information
flocculonodular lobe
nodulus is
medial flocculonodular
flocculus is
flocculus is lateral part of flocculonodular lobe
tf flocculonodular lobe is post to post lobe
f
ant to it

posterior lateral fissure
sep flocculonodular lobe and posterior lobe

Lateral Hemisphere
forms the bulk of the cerebellum

Paravermis:
Paravermis: R and L zones adjacent to the vermis

Molecular layer
contains local circuit neurons and abundant axons and dendrites.

.Purkinje cell layer (middle layer):
formed by a single layer of large neurons called Purkinje cells(PCs)
Granular layer (deep layer):
composed mainly of small granule cells, but also contains other cell types.

t The white matter core of the cerebellum is t
he location of the deep white matter cerebellar nuclei (DCN).

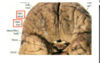
most medial of deep cerebellar nuclei (DCN)
receives projections from vermis
Fastigial nucleus •

lateral to fastigial n.
receives projections from paravermis
Globose nucleus

Emboliform nucleus
lateral to globose n
receives projections from paravermis

Dentate nucleus
• most lateral •
receives projections from lateral hemisphere

trunk is represented in
the midline region (vermis) of cereblar cortex

Label wat is missing on cerebllar cortex

Inferior Cerebellar Peduncle
afferents to cerebellum from spinal cord & medulla.

Middle Cerebellar Peduncle
o Mainly afferents to cerebellum from pontine nuclei

Superior Cerebellar Peduncle
Mainly efferents from the cerebellum.

highly convoluted, forming the cerebellar folia
cerebellum




(1.) cerebellar cortical region (2.) cerebellar nucleus/nuclei
Functional systems associated with the cerebellum

Buried within the white matter of the cerebellum
deep cerebellar nuclei (DCN)
primary vestibular afferents and axons of 2nd order neurons from the vestibular nucleus.
FN lobe and vermis

Purkinje cells in the FN lobe mainly project
directly to the vestibular nuclei
vermis project to the
fastigial nucleus (most) which serves as a relay to the vestibular nucleus.
Vestibulocerebellar System
tf body parts are epresented continuously in the cerebllar cortex
body parts are not represented continuouslyin the cerebllar cortex
fractured somatotopy
body part is represented in several locations on cerebellar cortexx
The cerebellum is attached to the brainstem by – pairs of —– bundles comprised of — and —- axons —– the cerebellum
The cerebellum is attached to the brainstem by 3 pairs of fiber bundles comprised of afferent and efferent axons to/from the cerebellum
These regions are involved in processing vestibular information
Vestibulocerebellum
These regions are involved in processing cerebral cortical inputs
Cerebrocerebellum
These regions are involved in processing proprioceptive inputs
Spinocerebellum
Axons travel superiorly within the
posterior spinocerebellar tract

lateral hemisphere and dentate nucleus
Cerebrocerebellum
flocculonodular lobe,
fastigial nucleus
vermis
Vestibulocerebellum
vermis, paravermis
globose and emboliform nuclei
Spinocerebellum
maintaining equilibrium, posture and head position
Vestibulocerebellar System
uses vestibulospinal tracts
Vestibulocerebellar System
primary vestibular afferents and axons of 2nd order neurons from the vestibular nucleus.
go thru Inferior cerebellar peduncle
Vestibulocerebellar System Assists in coordinating eye movements with head movements via
connections with the motor nuclei of CN-III, -IV and -VI
coordinating eye movements with head movements
of Vestibulocerebellar System
Vestibular apparatus (position of head in space) –>
vestibular nucleus –> cerebellum à vestibular nucleus
–> CN III, IV, VI via medial longitudinal fasiculus (MLF)
medial longitudinal fasiculus (MLF)
vestibular nucleus sends axons thru MLF to CN III, IV, VI
nuclei
axons sent thru MLF to CN III, IV, VI
nuclei
bilateral in
Vestibulocerebellar System
mooth pursuit
allows the eyes to follow a moving stimulus (maintains the stimulus on the fovea)
needs the cerebllum
smooth pursuit
Cortical eye fields –>vest nuclei–> Cb –> vestibular nucleus –> CN III, IV, VI nuclei via the MLF
Cortical eye fields –> pontine nuclei –> Cb –> vestibular nucleus –> CN III, IV, VI nuclei via the MLF
The cerebellum compares the—– ——with the intended movement and ——– the required corrections to maintain —— and proper eye position .
The cerebellum compares the vestibular input with the intended movement and “computes” the required corrections to maintain equilibrium and proper eye position .
Generalized loss of equilibrium
Lesion of the Vestibulocerebellum
Impaired ability to coordinating eye movements with head movements
Lesion of the Vestibulocerebellum
Altered output along medial vestibulospinal tract – Altered output along MLF
Lesion of the Vestibulocerebellum
Carries proprioceptive information trunk & LEs (T1 and below)
tPosterior Spinocerebellar Tract
tCuneocerebellar Tract
Carries proprioceptive information neck & UEs (rostral to T1)
Anterior Spinocerebellar Tract
proprioceptive information and cutaneous information
from receptors with large receptive fields from LEs
Carries proprioceptive information from the oral cavity
Trigeminocerebellar Tract
Propriceptive afferents travel in dorsal column
of Posterior Spinocerebellar Tract and travel to
Clarke’ s Column T1 - L2
Posterior spinocerebellar tract travels thru
Inferior cerebellar peduncle
tf Posterior Spinocerebellar Tract only travel to vermis
F vermis and paravermis
TF Cuneocerebellar Tract
Axons travel in the dorsal column (fasciculus cuneatus) to med/ internal/ accessory cuneate nucleus
Cuneocerebellar Tract
Axons travel in the dorsal column (fasciculus cuneatus) to Lateral/ external/ accessory cuneate nucleus
TF Cuneocerebellar Tract uses Clarke’s Column T1 - L2
F
propriceptive afferents from C1-C8
Cuneocerebellar Tract
Ipsilateral
Cuneocerebellar Tract
Posterior Spinocerebellar Tract
travels contralat then contralat back to same side
(after ascending)
Anterior Spinocerebellar Tract
Superior cerebellar peduncle
Anterior Spinocerebellar Tract
fibers
both use Inferior cerebellar peduncle
Cuneocerebellar Tract
Posterior Spinocerebellar Tract
Primary afferents synapse on spinal border cells (T2-L5)
Anterior Spinocerebellar Tract
Trigeminocerebellar Tract
Proprioceptive info carried along branches of CN-V (ie. muscles of mastication, periodontal ligament)
Proprioceptive info carried along branches of CN-V (ie. muscles of mastication, periodontal ligament) carried to
trigerm. cerebellar tract
spinal trigeminal nucleus.
Axons from the spinal trigeminal nucleus project to the cerebellum
trigem cereblar tract
via the inferior cerebellar peduncle.
trigeminoceebellar tract
cerebellum influences motor output by projecting to the
trigeminal motor nucleus.
This circuit allow the oral motor system to receive —— ——— during mastication
trgemcerebellar tract
This circuit allow the oral motor system to receive continual feedback during mastication
The cerebellum monitors the —— ——- on muscles of mastication and influences —— output accordingly.
trigem. cerebllar tract
The cerebellum monitors the changing demands on muscles of mastication and influences motor output accordingly.
(ant post)Spinocerebellar and Trigeminocerebellar Tract
functions
After processing proprioceptive information in cerebellum , cerebellar efferents project to motor regions, either directly or indirectly via the thalamus.
allows for adjustment of movement during ongoing movement
Functions Spinocerebellar and Trigeminocerebellar Tracts
The cerebellum compares the intended movement with the actual movement and “computes” the required corrections.
Efferent projections from the cerebellum corrects the movement
Corticospinal tract and Rubrospinal tract
act modulate motor output in the Spinocerebellar System in the Proprioceptive afferents responce
synapse in red nucleus
Rubrospinal tract efferent responce
contralateral to the skeletal muscle
Corticospinal tract and Rubrospinal tract
(Spinocerebellar System afferent responce)
Impaired ability to control axial muscles/ impaired trunk control
Lesion of the Spinocerebellum
Altered rate, range, accuracy of limb movements
Lesion of the Spinocerebellum
Dysmetria (overshooting a target)
lead to Intention Tremor
in Lesion of the Spinocerebellum
and inLesion to the Cerebrocerebellum
Dysmetria
Rely on the feed-back
inf olive role in cerebrocellebellar tract
recieves input from dentate(from cerebellar hemisphere)
then has to correct and send climbing fibers to lat hemisphere of cerebellum
Receives extensive input from the cerebral cortex (via pontine nuclei)
cerebellum in the
Cerebrocerebellar System
Involved in the planning, initiation, timing and control of motor movements.
cerebellum
VA/VL
recieves neurons from dentate
and sends neurons to motor cortex to modulate activity
Pontine nuclei
recieves infor fromcerebral cortex and sends info to lateral hemishphere of Cerebelum
climbing fibers
goes thru Inferior cerebellar peduncle to cerebellum(lat hemisphere)
Middle cerebellar peduncle
carries axons from pontne nucleus to lat cerebellum
contralat
Corticospinal and Rubrospinal Tracts
The cerebellar hemisphere compares the —- movement with the —– movement and “computes” the required corrections for the next time the task is performed.
The cerebellar hemisphere compares the intended movement with the actual movement and “computes” the required corrections for the next time the task is performed.
—— projections from the cerebellum corrects the movement via the —– tract.
Efferent projections from the cerebellum corrects the movement via the corticospinal tract.
Studies on non-human primates
reversible cooling in the —– nucleus resulted in delayed —– of movement.
reversible cooling in the dentate nucleus resulted in delayed onset/initiation of movement.
Lesion to the Cerebrocerebellum
Movement takes place —– rather than being coordinated smoothly
Lesion to the Cerebrocerebellum
Impaired ability to plan motor movement
seen with inactivating the interposed [globos/emboliform] in monkeys
Lesion to the Cerebrocerebellum
The basal ganglia (basal nuclei) are a group of —– ——nuclei.
The basal ganglia (basal nuclei) are a group of functionally related nuclei.
Subthalamic Nucleus (STN)
located in diencephalon

Dopaminergic neurons
are located in dorsal part of the substantia nigra
(cmpact part

also located medially in ventral tegmental area.
Dopaminergic neurons

Substantia Nigra (SN)
Compact Part (SNc) and Reticular Part (SNr)
in midbrain


dopamine
“reward system

The substantia nigra (reticular part) functions with the
—–as the output from the —-.
The substantia nigra (reticular part) functions with the GPi as the output from the BG.
ventral region of continuity btwn caudate and putamen
striatum
lenticular nucleus
putamen
gpe
gpi
cognition processes and control of movements.
dopamine
dopamine
enjoyment and pleasure, which reinforces and motivates
extrapyramidal system”
describes the nuclei and pathways of the BG
termed in 1900 by early 1900s Kinnier Wilson
influences motor and non motor sysem
basal ganglia
A lesion to —- —— of the BG will disrupt movement
A lesion to one or more of the BG will disrupt movement
Absence of spontaneous movement/ slowness of movement
Inability to inhibit unwanted movements
A lesion to one or more of the BG
TF BG directly innervate LMNs in the spinal cord or cranial nerve nuclei;
F BG do NOT directly innervate LMNs in the spinal cord or cranial nerve nuclei;
TF lesion to one or more of the BG produce paralysis
lesion to one or more of the BG does not produce paralysis
tf BG only influence motor actions
t BG only influence motor actions
Hypokinetic Disorder
Parkinson’s Disease
loss of dopaminergic neurons in the SNc
Parkinson’s Disease a hypokinetic disease
Akinesia/Bradykinesia: without (difficulty initiating) movement/ slowness of movement
Hypokinetic Disorder
Parkinson’s Disease
Rigidity: increase in muscle tone
Resting tremor:
rhythmic involuntary movement at rest
in Parkinson’s Disease
Hypokinetic Disorder like parkinsons dispkay
Postural instability
Chorea:
rapid, abrupt and random movements (limbs, face)
Hyperkinetic Disorders
Putamen
input from motor and somatosensory cortices
influences motor output.

info from limbic cortex, hippocampus and amygdala
N. Accumben

emotional and behavioral functions.
N. Accumbens

Athetosis:
slow, writhing movements
Hyperkinetic Disorders
Hyperkinetic Disorders
Types of abnormal involuntary movements
Ballism(“ballistic movement ”)
:violent, large-amplitude mvmts
hyperkinetic disease
Huntington’s Disease (HD
progressive degeneration of projection neurons and local circuit neurons in the caudate and putamen.
TF in huntington;s disease a Hyperkinetic Disorders;
Neurons that give rise to the indirect pathway are preferentially lost.
F Neurons that give rise to the indirect pathway are preferentially lost.
extensive —– projections to the striatum;
extensive cortical projections to the striatum;
recivees info from cortical association areas and has a role in cognitive functions
Caudate
cognitive functions
Dorsolateral prefrontal Loop:
motor output.
motor loop
Orbitofrontal loop:
planning and initiating socially appropriate actions
Limbic loop
emotional and behavioral functions.
Oculomotor loop:
control of orientation and gaze.
general loop structure
Cortex 2 BG 2 Thalamus 2 Cortex
Motor Loop
putamen of BG(step 2)
ventral caudate (C) and n. accumbens(step 2)
Orbitofrontal loop
nucleus accumbens (A) and other BG nuclei
Limbic loop:
caudate (C) and other BG
Oculomotor loop and Dorsolateral prefrontal Loop:
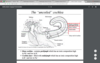
cortical neurons project to the —– where glutamate is released.
cortical neurons project to the striatum where glutamate is released.
—— neurons in the substantia nigra, ——- project to the striatum
Dopaminergic neurons in the substantia nigra, pars compacta (SNc) project to the striatum
—– projections provide an important pathway for the modulation of the —– and —— pathways
nigrostriatal projections provide an important pathway for the modulation of the direct and indirect pathways
Di +
Direct pathway: facilitates motor (or cognitive) programs
D2, –
Indirect pathway: inhibits the execution of competing motor programs
Direct pathway by D1 +
GPi/ SNr
Indirect pathway
D2-
–>GPe
excited by dopamine and project to Gpi
(direct pathway)
Striatal neurons with D1 receptors are excited by
Striatal neurons with D1 receptors are excited by dopamine
(direct pathway)
Striatal neurons with D2 receptors are inhibited
Striatal neurons with D2 receptors are inhibited by dopamine
(indirect pathway)
project to Gpe
Striatal neurons with D2 receptors
dopaminergic projections
lost in Parkinson’s disease.
Increased Activity of the Direct Pathway Occurs in the Presence of
Direct Pathway
Glutamate and Dopamine
inc GABA in GPi/ SNr from striatum
decreased GABA release in the thalamus
Direct path
low GABA put in from (GPi/SNr) ; more Glu excreted from
thalamus
more glu neurons from thalamus
more glu neurons from motor cortex(CC)
Direct pathway
1.Dopamine released from SN leads to —– of GABAergic neurons projecting from striatum to GPe.
Direct path
1.Dopamine released from SN leads to inhibition of GABAergic neurons projecting from striatum to GPe.
STN in direct pathwya
inc GABA
decrease firing of glutamatergic neurons projecting from STN to Gpi/ SNr
caused from 3. Increased GABA levels in STN
(Direct pathway)
decreased GABA release into thalamus
b/c of Reduced excitation of GPi /SNr-GABAergic neurons
tf in the direct path
STN has inc firing of glutamatergic neurons projecting from STN to Gpi/ SNr
STN has decrease firing of glutamatergic neurons projecting from STN to Gpi/ SNr
tf dopaminergic neurons only relased from
Snc
leff; more ;less
direct path
GABAergic neurons projecting from striatum to GPe.;
GPe neurons are disinhibited, leading to increased GABA levels in STN
Increased GABA levels in STN causes decrease firing of glutamatergic neurons projecting from STN to Gpi/ SNr
Glutamate released from corticostriatal fibers leads to ——–activity of—– neurons projecting from striatum to GPe
indirect path
Glutamate released from corticostriatal fibers leads to increased activity of GABAergic neurons projecting from striatum to GPe
less Glu from STN and less GABA from GBI
hyperkinesia

more GABA from striatum and GPI/SNR
indirect pathway and hyperkinesia
inhibition of GPe neurons
indirect path
occurs from Activation of GABAergic projections from striatum to GPe
disinhibition of glutamatergic neurons projecting from STN to Gpi/ SNr
indirect pathway
from Inhibition of GPe neurons
Gpi/SNr - GABAergic neurons excited
in indirect pathway3
inc GABA release in indirect pathway from
Striatum
and (GPi/SNr)
inhibited glutamatergic projections in indirect path
Thalamus (VA,VL)
and motor cortex
Increased Activity of the Indirect Pathway
presense Glutamate (absence of dopamine)
degeneration of dopaminergic neurons in SNc
Parkinson’s Disease
Dopamine inhibits
GABAergic neurons projecting from striatum to GPe
Dopamine excites
GABAergic neurons projecting from striatum to GPi
lesion of the subthalamic nucleus
resulting hyperkinesia
Degeneration of neurons in caudate and putamen
(indirect pathway)
Huntington’s Disease/ Huntington’s Chorea
excess movement
GABA D2 not stimulated much
Huntington’s Chorea
vertebral arteries (R and L)
ascend through the transverse foramina of the cervical vertebra and enter the cranial cavity via the foramen magnum.
internal carotid arteries
ascend through the neck to the base of the skull and enter the cranial cavity through the carotid canal.
The vertebral arteries contribute to the ——-
circulation
The vertebral arteries contribute to the posterior circulation
Vertebral arteries
, ascend through the transverse foramina of the cervical vertebra and enter the cranial cavity via the foramen magnum.
pontomedullary junction,
the right and left vertebral arteries unite to form the basilar artery.
The anterior and posterior spinal arteries
arise from the vertebral arteries
supply the spinal cord
anterior and posterior spinal arteries
travel midline spinal cord (
Anterior Spinal Artery
travel just posterior to the dorsal horn of the spinal cord (bilateral)
Posterior Spinal Arteries
spinal arteries braches from the vertebral artery provide
sufficient blood supply to the upper cervical spinal cord levels only.
one anterior and two posterior spinal arteries extend —–to supply the spinal cord
one anterior and two posterior spinal arteries extend caudally to supply the spinal cord
radicular arteries.
reinforce anterior and posterior spinal arteries
radicular arteries
branches off of the posterior intercostal arteries.
radicular artery at ~T12 spinal cord level
called the great radicular artery
may provide the entire arterial supply for the lumbosacral spinal cord.
vertigo and ipsilateral deafness
occlusion of internal auditory or labyrinthine artery
basilar artery terminates by bifurcating
into the two posterior cerebral arteries
which of the following isnt a branch of the basilar art
Anterior inferior cerebellar artery
pontine arteries
Superior cerebellar artery
internal auditory or labyrinthine artery
Posterior inferior cerebellar artery
t Posterior inferior cerebellar artery
anterior spinal artery, vertebral artery, PICA supply
Caudal medulla
posterior spinal artery
Caudal medulla :
pons is mainly supplied by branches of the —–
artery
pons is mainly supplied by branches of the basilar artery
caudal pontine
anterior inferior cerebellar artery and
basilar artery
rostral pontine levels
basilar artery and superior cerebellar artery
Most of the midbrain is supplied by the —— —– —- and their branches
Most of the midbrain is supplied by the posterior cerebral arteries and their branches
Blood supply to the most dorsal aspect of the midbrain arises from the ——- ——- ——-
Blood supply to the most dorsal aspect of the midbrain arises from the superior cerebellar artery.
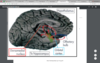
Supplies the occipital lobe and medial and inferior surface of the temporal lobe
Posterior cerebral artery (PCA) territory

lesion to post column
vibration and position sense
lesion to anterolateral pathways
pain and temp sense
motor loss
lateral medullary syndrome
Wallenberg’ s Syndrome

ischemia in the territory of the vertebral artery and/or PICA.
Wallenberg’s syndrome
spinal trigeminal nucleus and tract of wallensurg syndrome
contralat body dec. pain and temp sense
Spinothalamic tract of wallenburg syndrome
contralat body dec pain and temp sense
hoarsenss and dysphagia
nucleus ambiguous of wallenburg syndrome
ipsilateral dec taste
nucleus solitary of Wallenburg syndrome
descending symp. fibers of wallenburg syndrome
ipsilateral horners syndrome
inf cerebral peduncle, vestibular nuceli
ips ataxia, vertigo, nausea, nystagmus
bilateral ventral pons ischemia
Locked-in Syndrome
narrowing of basilar artery
Wallenburg syndrome
he/she is only capable of eye movements.
Locked-in Syndrome
pontomesencephalic reticular formation
spared in Locked-in Syndrome
Locked-in Syndrome
consciousness is spared.
only capable of eye movements
Locked-in Syndrome
by bilateral ventral midbrain ischemia (cerebral peduncles)
Locked-in Syndrome
secondary to lack of blood flow in the rostral basilar artery
Locked-in Syndrome
The “Circle of Willis” connects the —– and —–
arterial cerebral circulation
The “Circle of Willis” connects the anterior and posterior arterial cerebral circulation
©Both ICAs terminate by giving rise to
a middle cerebral artery (MCA) and anterior cerebral artery (ACA).
Prior to terminating, however, each ICA gives off a .
posterior communicating artery
posterior communicating arteries project posteriorly to communicate with the
posterior cerebral artery (PCA).
two ant cerebral art are connected by an anastomosing branch called the
anterior communicating artery.
not part of circle of willis
middle cerebral artery
hip and down provided by
Anterior cerebral artery (ACA)
middle cerebral artery
supply rest of body other than LE
lenticulostriate arteries
given off by middle cerebral arteries as they course lateral
frequent site of stroke
lenticulostriate arteries
internal capsule and deep gray matter
lenticulostriate arteries
formed by tight junctions between the endothelial cells lining CNS capillaries
Blood Brain Barrier
limit the flow of substances from capillaries into the CNS
tight junctions of Blood brain barrier
hydrophilic substances such as amino acids and glucose and medications
cant cross bbb alone
need carrier
Lipid soluble molecules, such as ethanol, nicotine and caffeine
cross the BBB,
Intermediate meningeal layer
Arachnoid
Conforms to shape of brain …
does not dip into sulci
Delicate membrane
Arachnoid
Pia mater
Adheres to the brain, following all of its contours
Dura mater
External Periosteal Layer
Internal Meningeal Layer
Internal Meningeal Layer of dura mater
Dense fibrous connective tissue
invaginates along the longitudinal fissure, between the two cerebral hemispheres
Falx cerebri
positioned between the occipital and temporal lobes - and- cerebellum
Tentorium cerebelli:
External Periosteal Layer
Formed by the periosteum which adheres to the internal surface of skull
two largest dural reflections are
Falx cerebri
©Tentorium cerebelli
dural venous sinuses
Dural reflections
receive deoxygenated blood
conveys deoxygenated blood from cerebral veins to the internal jugular vein
dural venous sinus system
arrange
venous sinuses –> cerebral arteries capillaries –>internal jugular vein–> cerebral veins
cerebral arteries capillaries –> cerebral veins –> venous sinuses –> internal jugular vein
diff b/n Cerebral veins and dural venous sinuses
typical venous histology vs. dural spaces lined with endothelial cells
Potential space between cranium & periosteal layer of dura
Epidural space
Epidural hemorrhage/ hematoma
Most frequently occurs with trauma/skull fracture
Epidural hemorrhage/ hematoma
Laceration/ tearing of the meningeal artery and
Bleeding into the potential space between the cranium and periosteal layer of dura
the periosteal dura encloses the
meningeal vessels.
subdural space
Potential space between the dura and arachnoid
Subdural Hemorrhage/ Hematoma
secondary to rapid acceleration/deceleration which pulls the brain away from the skull
Interventricular Foramen (Foramen of Monroe)
communicates Lateral Ventricles (2) Right Left
to 3rd ventricle

communication between 3rd and 4th ventricle
Cerebral Aqueduct (Aqueduct of Sylvius)

tears cerebral veins as they enter the dural sinus
Subdural Hemorrhage/ Hematoma
subarachnoid space
true space that contains blood vessels and CSF
Subarachnoid Hemorrhage/ Hematoma
arterial hemorrhage
Subarachnoid Hemorrhage/ Hematoma
~70% are 2° aneurysm
Foramen of Magendie
Midline opening in the 4th ventricle
Foramen of Luschka
Paired openings in the 4th ventricle
CSF is made in the —— ——-, it circulates through the ——— and exits the —- ventricle
CSF is made in the choroid plexus, it circulates through the ventricles and exits the 4th ventricle
As CSF leaves the 4th ventricle, it enters the
subarachnoid space.
CSF travel to subarachnoid space into the dural venous sinuses
via arachnoid granulations
Frontal and Parietal lobes
• Attention
Parietal Lobes
Visuospatial
Frontal and Temporal Lobes
Language
• Executive function
Frontal Lobes
Temporal and Frontal lobes
Memory
• Area of cortex between frontal and occipital lobes
parietal lobe
Principle regions of parietal lobe
• post-central gyrus • superior parietal lobule • supramarginal gyrus • angular gyrus
Processes and integrates somatosensory and visual information
parietal lobe
parietal lobes
Processes sensations
and guidance of movement
“Gerstmann’s Syndrome.”
• Lesion usually in angular and supramarginal gyri
Left parietal lobe damage
• right-left confusion, dysgraphia, dyscalculia
“Gerstmann’s Syndrome.”
finger agnosia.
“Gerstmann’s Syndrome.”
Right parietal lobe damage
Neglect of contralateral side of body or space
Difficulty making things (constructional apraxia)
Denial of deficits (anosagnosia)
Right parietal lobe damage
• Sensory Thresholds • Prosopagnosia•
other symptoms of parietal lobes damage
• Inability to locate and recognize parts of the body or self
other symptoms of parietal lobes damage
• Neglect of visual, auditory and somatosensory stimuli on the side of the body opposite to the lesion
Contralateral Neglect
defective sensation and perception and
defective attention
cause Contralateral Neglect
Temporal Lobe
below the Sylvian fissure and anterior to occipital cortex
Temporal lobe
amgydala, limbic cortex, and hippocampus
Temporal Lobe
auditory and gustatory areas
• Inputs from all sensory modalities, parietal and frontal lobes,
Temporal Lobe
input from ventral visual stream, limbic structures and basal ganglia
Temporal Lobe
Wernicke’s area
Temporal Lobe
Comprehension of language
Wernicke’s area of temporal lobe
Processing of auditory input
Primary auditory cortex of temporal lobe
Learning and memory
Hippocampus and Amygdala of Temporal lobe
• Lesion in superior temporal gyrus
Wernicke’s Aphasia
• Comprehension of speech is impaired
• Comprehension of speech is impaired
Wernicke’s Aphasia
Speech is: –
fluent but meaningless (word salad) –
devoid of any content –
neologisms
Wernicke’s Aphasia
Content ranges from mildly inappropriate to complete nonsense
Wernicke’s Aphasia
The ability to encode, store, retain, recall and recognize information
Memory
Memory
duration of memories and formation and retrieval of information
Four types of memory based on
duration of retention
Sensory memory •
200-500 ms after input is perceived
– Working memory •
Focuses on the processing of briefly stored information
– Short-term memory •
Holds a few items briefly before the information is stored or forgotten
Long-term memory •
Relatively permanent and limitless storehouse
Three stages in the formation and retrieval of memory:
Encoding storage retrieval
• Processing and combining received information
encoding
• Creation of a permanent record of the encoded information
storage
• Calling back stored information in response to some cue for use in a process or activity
Recognition
Recall
Hippocampus
Consolidates memories
• Critical structure for explicit memory
hippocampus
Hippocampus
Made permanent before stored elsewhere
Hippocampus
curved sheet of cortex in the medial temporal lobe
Hippocampus
Dentate gyrus
Subiculum
CA (cornu ammonis) subfields

Entorhinal Cortex (EC)
Main input to HC and a target of hippocampal output
Hipocampus
amygdala to the splenium of the corpus callosum
A collection of nuclei located at the anterior end of the hippocampus
Amygdala

severe anterograde amnesia
Bilateral removal of the hippocampus; patient was unable to form new memories of facts or events
Bilateral removal of the hippocampus
• Past, early memories were intact
• Mirror Drawing Task with Case of Patient HM
H.M.ʼs performance does improve on this task
BUT Doesnʼt remember ever completing the task
Amygdala Sends impulses to hypothalamus for activation of the —- —– —–
sympathetic nervous system
associating sensory stimuli with appropriate emotion response
and Also involved in sense of smell
amygdala
Efferents of amygdala
project to the cerebral cortex and hypothalamus
Visceral inputs, particularly olfactory inputs, are especially prominent
to amygdala
• Involved in memories of emotional, olfactory and visceral events
Amygdala
Frontal Lobe; All cortical tissue anterior to
central sulcus
Stroke in Hippocampus and/or Amygdala
• Profound memory impairments
Impaired ability to determine and identify emotional significance of stimuli or events
Stroke in Hippocampus and/or Amygdala
• Decreased emotional responses
Decreased responsiveness, aggression, fear, dominance and social interest
All neural roads lead to the
frontal lobes”
motor • premotor • prefrontal
functional distinct regions of frontal lobe
Motor Movements Speech Production
Frontlal Lobe
Planning Organizing Problem solving
Frontal Lobe
Personality Behavior Emotions
Frontal Lobe
Selective attention
Frontal Lobe
• Primary motor cortex
Controls contralateral side of body • ‘motor homunculus’ •
Primary motor cortex
voluntary, skilled movements
• Premotor cortex
• sequencing, timing, and initiation of voluntary movements
Brocha’s area of Frontal Lobe
speech production
Motor and pre-motor cortices of frontal lobe
direct control of movements through projections to spinal motor neurons and cranial nerve motor neurons
Motor and pre-motor cortices of frontal lobe
also projects to basal ganglia
lesion to Broca’s Aphasia
Inability to speak fluently
Non-fluent speech
Few words, short sentences, many pauses
lesion to
Broca’s Aphasia
Words produced with effort and sound distorted • Repetition is impaired
lesion to Broca’s Aphasia
Repetition is impaired •
Comprehension is relatively intact • Awareness of mistakes
Prefrontal Cortex: Executive Functions of Frontal Lobe
effective and efficient goal-directed behavior; organization of behavior & cognition
Prefrontal Cortex of Frontal Lobe
Initiating - Inhibiting and Judgment
- Planning and organizing
and problem solving
Prefrontal Cortex
Selective attention
- Self-monitoring
Prefrontal Cortex
Abstract thinking and mental flexibility
Prefrontal Cortex:
frontal lobe lesion
Short-term memory impairment
• Loss of flexible thinking
Poor response inhibition
Damage to the Frontal Lobe
Inappropriate social & sexual behavior
Damage to the Frontal Lobe
Impaired judgment, abstract thinking, hypothesis testing and planning
Damage to the Frontal Lobe
• Difficulties using cues and information from the environment to direct, control, or change behavior
Damage to the Frontal Lobe
Occiptal lobe Separated from parietal and temporal lobes
by parieto-occiptal sulcus
Primary visual cortex is Brodmann area 17,
Occipital lobe
Posterior pole of cerebral hemispheres
Occipital Lobe
Dorsal stream of occipital lobe
visual information to posterior parietal cortex
Dorsal stream of occipital lobe
“where”
Ventral stream of occipital lobe
visual information to inferotemporal cortex
Ventral stream of occipital lobe
what
Can only perceive movement through a compilation of still images as if watching the world through a strobe light
Akinetopsia
Akinetopsia
inability to perceive motion
brain damage disrupting input to the dorsal pathway (V5/MT).
Akinetopsia
Occipital Lobe Dysfunction
Visual agnosia, Prosopagnosia,Akinetopsia
inability recognize an object
Visual agnosia
Prosopagnosia
inability to recognize faces including their own
Agnosia?
• Inability of the brain to process or make use of sensory stimuli
Sensory perception of the stimulus is disconnected from memories associated with the stimulus
Agnosia
strokes, dementia, carbon monoxide poisoning cause
Agnosia
agnosia not same as
blind or deaf
Auditory Agnosia
Inability to recognize sounds
Inability to perceive objects through tactile stimulation
Somatosensory Agnosia
Difficultly recognizing objects, faces and words
Visual agnosia
occipital disfunction
Cannot sort pictures or objects into categories and – Cannot name objects
Visual agnosia
Visual agnosia
Prosopagnosia
Akinetopsia
Occipital Lobe Dysfunction
Prosopagnosia
Severe disturbance in the ability to recognize faces
Lesions of inferior and medial occipital lobe
Prosopagnosia
Recognition of facial parts is intact
Prosopagnosia
Prosopagnosia
• Accurate judgments about gender, age and emotion are still intact and can recall detailed information about a specific individual
Language is
any system for representing and communicating ideas
speech
particular audible manner of communicating language
Broca’s area –
production of area
Wernicke’s area –
Comprehension of language
Wernicke-Geschwind Model
Neural Basis of Language
Wernicke-Geschwind Model
Comprehension – Production – Reading
When we listen to speech, words are send via pathways to primary auditory cortex (Heschl’s gyrus);
relayed to Wernicke’s area(Comprehension)
Broca’s area
holds representations for articulating words –
broca’s area(language production)
Instructions are sent to facial area of motor cortex -> facial motor neurons in brain stem
Reading;Information is sent to visual areas 17, 18 and 19
– Goes to angular gyrus -> Wernicke’s area
Wada Test
Sodium amytal, an anesthetic, is injected into the right or left carotid artery
Wada test
If the left hemisphere is put to sleep in people who have language ability in the left hemisphere
person cannot speak
if right hemisphere is put to sleep, then will be able to speak
with anestiic in left hemisphere
person can still talk
Identifying Language Areas;
Electrical stimulation of the cerebral cortex on left side
left side dominance language will be disrupted with electrode stimulation


