Acute Infectious Diarrhea Flashcards
What are the five high risk groups in the US for acute infectious diarrhea?
- Travelers
- Immunodeficient
- Daycare workers/attendees and their family
- Institutionalized persons (ex. nursing home)
- Consumers of certain foods
What is the pathogenesis of acute infectious diarrhea?
a. Bacterial toxins, enterotoxin producing bacteria
b. entero-adherent pathogens
c. cytotoxin producing and invasive microorganisms
- –> small bowel hypersecretion
- profuse, watery diarrhea
- marked vomiting
- minimal or no fever
- abruptly (within a few hours of ingestion)
- –> small bowel hypersecretion
- vomiting usually less
- abdominal cramping/bloating is greater
- fever is higher
- High fever, abdominal pain
What in the history would be a high risk factor for diarrhea?
- Recent antibiotics?
- Ill contacts?
- Travel?
- Risk factors like unclean drinking water?
- Daycare/Nursing home?
- Animal exposure?
- Immunosuppression/immunocompromised?
- Unpasteurized dairy?
- Consume raw/undercooked meat, fish, or shellfish?
- Pregnancy (listeriosis)?
Pt. presents with thirst, difficulty swallowing food due to a dry mouth, and has only urinated a few times in the past 24 hours. What is the classification of their diarrhea?
Mild
thirst, dry mouth, decreased, axillary sweat, decreased urine output, sligh weight loss
What signs would imply moderate dehydration? severe?
moderate - orthostatic fall in blood pressure, skin tenting, sunken eyes (infants = sunken fontanelle)
severe - lethargy, obtundation, feeble pulse, hypotension, frank shock
What do you typically hear on ausculation for diarrhea? ileus or toxic megacolon?
a. increased bowel sounds
b. decreased bowel sounds
What is the transmission of acute infectious diarrhea?
fecal-oral transmission
typically self-limited
Flow chart of acute diarrhea work up
38.5oC = 101.3oF

What is the standard workup for acute diarrhea?
nothing - typically it is self limited
What signs make you do a full evaluation of acute diarrhea?
- profuse diarrhea (6 or more stools/day) with dehydration
-
hypotension and tachycardia
- not responsive to initial volume repletion
- Dysentery? (bloody diarrhea with leukocytes [mucoid])
- fever ≥38.5°C
- duration >48 h without improvement
- recent antibiotic use (check for C. Diff)
- new community outbreaks
- associated severe abdominal pain
- in patients >50 years
- peritoneal signs
- elderly (≥70 years)
- immunocompromised patients
- creatinine level greater than 1.5 times the baseline value
- peripheral leukocytes ≥ 15,000 cell/uL
What tests might be included in the work up of acute diarrhea?
CBC
electrolytes
BUN
Cr
Blood culture
What is the key to diagnosis of acute diarrhea?
microbiologic analysis of the stool
What organisms are included in a routine stool culture?
- Salmonella
- Shigella (Shiga toxin)
- E. Coli
- Most detect campylobacter (although may need to be requested)
*Takes 24-48 hours for results
If you want to check for enterohemorrhagic or othertypes of E. coli, vibrio species, or yersinia, you have to do what?
ask the lab (not included on standard culture)
same goes for:
- stool immunoassay for C. diff
- Ova and parasites (need 3 samples)
- Stool protozoal antigen (giardia, cryptosporidium, E. histolytica)
- Stool viral PCR/antigen (rotovirus, norovirus)
If your stool studies are unrevealing, what’s the next step?
endoscopy:
flexible sigmoidoscopy with biopsies
upper endoscopy with duodenal aspirates and biosopies
What do you see here?

ileus or toxic megacolon
radiology can also detect free intraperitoneal air
What is a benefit of abdominal CT?
more sensitive for free air
identify colitis
If pt reports food poisoning from bad chicken, you might suspect:
salmonella, campylobacter, shigella
If pt reports food poisoning from undercooked hamburger, you might suspect:
enterohemorrhagic E. coli (O157:H7)
If pt reports food poisoning from fried rice, you might suspect:
bacillus cereus
If pt reports food poisoning from eggs, you might suspect:
salmonella
If pt reports food poisoning after eating a turkey sandwich with american cheese, you might suspect:
listeria
due to uncooked foods like lunch meat or soft cheeses
If pt reports food poisoning from seafood, you might suspect:
vibrio species, salmonella, acute hepatitis A, norwalk, campylobacter
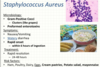
- Staphylococcus Aureus*
a. microbiology
b. sx
c. tx
d. risk factors