Acute and Emergency Dermatology Flashcards
What are the consequences of failure of the skin?
–Sepsis
–Hypo- and Hyper- thermia
–Protein and fluid loss
–Renal impairment
–Peripheral vasodilation
•Can occasionally lead to cardiac failure
What is erythroderma?
Any inflammatory disease affecting over 90% of the total skin surface
What are the causes of erythroderma?
Psoriasis
Eczema
Drugs
Cutaneous lymphoma
Hereditary disorders
What are the principles of management of erythroderma?
Remove offending drugs
Maintain fluid balance
Good nutrition
Ensure patient remains at suitable temperature
Emollients - 50:50 liquid paraffin: white soft paraffin
Oral and eye care
Anticipate and treat infection
Manage itch
Disease specific therapy; treat underlying cause (e.g - eczema, psoriasis, cutaneous lymphoma)
When do drug reactions resulting in skin symptoms often occur?
Commonly 1-2 weeks after drug - within 72 hours if re-challenged
What are the mild and severe forms of drug reactions?
Mild - morbilliform exanthem
Severe - Erythroderma, stevens johnson syndrome/toxic epidermal necrolysis, DRESS
What causes the onset of Stevens johnson syndrome and toxic epidermal necrolysis?
Secondary to drugs -
–Antibiotics
–Anticonvulsants
–Allopurinol
–NSAIDs
What are the clinical features of SJS?
•Fever, malaise, arthralgia
•Rash
–Maculopapular, target lesions, blisters
–Erosions covering <10% of skin surface
•Mouth ulceration
–Greyish white membrane
–Haemorrhagic crusting
•Ulceration of other mucous membranes
What is the prodrome of TENS?
Febrile illness
What is the clinical presentation of toxic epidermal necrolysis?
Ulceration of mucous membranes
Rash:
–May start as macular, purpuric or blistering
–Rapidly becomes confluent
–Sloughing off of large areas of epidermis – ‘desquamation’ > 30% BSA
–Nikolsky’s sign may be positive
Nikolsky sign is a skin finding in which the top layers of the skin slip away from the lower layers when slightly rubbed
What is the management for TEN?
Identify and stop culprit drug as soon as possible
Supportive therapy
- ?High dose steroids
- ?IV immunoglobulins
- ?Anti-TNF therapy
- ?Ciclosporin
What score is used to determine the prognosis of TEN?
SCORTEN
What are the long term complications of TEN?
–Pigmentary skin changes
–Scarring
–Eye disease and blindness
–Nail and hair loss
–Joint contactures
What is erythema multiform?
Abrupt onset of 100s of lesions over 24 hours - hypersensitivty reaction usually triggered by infection (HSV and mycoplasma pneumonia)
Where are the lesions located in erythema multiforme?
Go from distal to proximal
Start at the palms and the soles
Includes mucosal surfaces
What happens to the lesions over time?
They evolve over 72 hours - pink macules become elevated and may blister in the centre
Resolves over 2 weeks
What does dress stand for?
Drug reaction with eosinophilia and systemic symptoms
What is the onset of dress?
2-8 weeks after drug exposure
What are the clinical featrures of DRESS?
Fever and widespread rash
Eosiniphilia and deranged liver function
Lymphadenopathy
Possible involvement of other organs
What is the management for dress?
Stop causative drug
Treat symptoms
Systemic steroids
Possible immunosuppressants or immunoglobulins
What causes pemphigus?
Antibodies targeted at desmosomes
What are the clinical features of pemphigus?
Flaccid blisters which rupture very easily
Common sites for the blisters include the face, axillae, groins
Nikolsky’s sign may be positive
Commonly affects the mucous membranes, ill defined erosions in the mouth
Can also affect the eyes, nose and genital areas
Where are antibodies directed in pemphigoid?
•Antibodies directed at dermo-epidermal junction
Describe the blisters in pemphigoid
- Intact epidermis forms roof of blister
- Blisters are usually tense and intact
What are the differences between pehigus and pemphigoid?

What are the causes of erythrodermic psoriasis and pustular psoriasis?
Infection
Sudden withdrawal of oral steroids or potent topical steroid
What are the clinical features of Erythrodermic psoriais and Pustular Psoriasis?
- Rapid development of generalised erythema, +/- clusters of pustules
- Fever, elevated WCC
What is the management of erythrodermic psoriasis and pustular psoriasis?
Exclude underlying infection, blsnd emollient and avoid steriods
Often requires initiation of systemic therapy
What causes eczema herpeticum?
•Disseminated herpes virus infection on a background of poorly controlled eczema
What are the clinical features of eczema herpeticum?
•Monomorphic blisters and “punched out” erosions
–Generally painful, not itchy
•Fever and lethargy
What is the treatment for eczema herpeticum?
Treatment dose aciclovir
Mild topical steroid if required to treat eczema
Treat secondary infection
Ophthalmology input if peri-occular disease
In adults consider underlying immunocompromise
What is staphylococcal scalded skin syndrome?
Initial staph infection, may be subclinical (common in children, but can occur in immunocompromised adults)
Diffuse erythematous rash with skin tenderness
Prominent in flexures
Blistering and desquamation follows
What is the disease process of staphylococcal scalded skin syndrome?
Staphylococcus produces a toxin which targets desmoglein 1
Despite the rash and the blistering, what other symptoms does the patient have?
Fever and irritability
What is the treatment for staphylococcal scalded skin syndrome?
Admission for IV antibiotics initially and supportive care
Generally resolves over 507 days with treatment
What is urticaria?
–Central swelling of variable size, surrounded by erythema. Dermal oedema
What causes the itching / brining feeling of urticaria?
Histamine release into the dermis
What is the disease progression of urticaria?
–fleeting nature, duration: 1- 24 hours
What is angioedema?
–Deeper swelling of the skin or mucous membranes
What are the causes of acute urticaria?
Idiopathic
Infection (viral)
Drugs, IgE mediated
Food. IgE mediated
What is the treatment for acute urticaria?
•Oral antihistamine
–Taken continuously
–Up to 4 x dose
- Short course of oral steroid may be of benefit if clear cause and this is removed
- Avoid opiates and NSAIDs if possible (exacerbate urticaria)
What is the definition of chronic urticaria?
History of over 6 weeks
What are the causes of chronic urticaria?
Autoimmune / idiopathic (60%)
Physical (35%)
Vasculitic (5%)
Rarely a type 1 hypersensitvity reaction
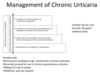
What is the management of chronic urticaria?