8.3 Respiratory Physiology (HT) Flashcards
State the body’s resting oxygen consumption and maximum oxygen consumption.
- Resting oxygen consumption = 250ml/min
- Maximum oxygen consumption = 3000ml/min
What are the two main zones of the functional structure of the airways? What are their volumes?
- Conducting zone or Anatomical dead space (150ml)
- Respiratory zone (3000ml)
Describe the idealised model of the functional structure of the airways (i.e. how they branch).
- There are 23 generations of bifurcation:
- 0 is the pharynx, larynx and trachea
- 1 and 2 are the bronchi
- 3 to 15 are the bronchioles
- 16 is the terminal bronchioles
- 17 to 19 are the respiratory bronchioles
- 20 to 22 are the alveolar ducts
- 23 is the alveolar sacs
- Terminal bronchioles mark the transition from the conudcting zone and the respiratory zone

Who produced the idealised model of the functional structure of the airways?
Weibel
What is a primary lobule or acinus?
It is what stems from 1 terminal bronchiole.
What is the boundary between the conducting zone and the respiratory zone?
Terminal bronchioles
How many alveoli are there according to the idealised model of the airways? What is the area of this?
- 223 = 8.4 million alveolar sacs = 300 million alveoli
- 70m2 area
Draw a graph to show how the cross-sectional area of the airways changes as you go further into the lungs.

How and why does the velocity of air in the lungs change as you go further into the lungs and what is the consequence of this?
- The velocity decreases because the cross-sectional increases
- The velocity drops greatly around generation 16/17 (terminal bronchioles), so diffusion becomes dominant instead of convection
- This marks the division between the conudcting zone and respiratory zone
Compare how the oxygen percentage in the conducting zone and respiratory zones of the airways vary.

How do values for the normal alveolar partial pressures of oxygen (PAO2) and carbon dioxide (PACO2) compare with the normal arterial values and why?
- They are very close to each other
- This is because the alveoli are in the respiratory zone of the airways, so the velocity of air is very low, meaning that new air is rapidly mixed up with existing gas by diffusion

Explain the concept of respiratory dead space.
- Dead space of the respiratory system refers to the space in which oxygen and carbon dioxide are not exchanged across the alveolar membrane in the respiratory tract.
- Anatomic dead space specifically refers to the volume of air located in the segments of the respiratory tract that are responsible for conducting air to the alveoli and respiratory bronchioles but do not take part in the process of gas exchange itself. These segments of the respiratory tract include the upper airways, trachea, bronchi, and terminal bronchioles (i.e. the conducting zone).
- Alveolar dead space, on the other hand, refers to the volume of air in alveoli that are ventilated but not perfused, and thus gas exchange does not take place.
Define total ventilation and alveolar ventilation.
- Total ventilation
- The total volume of gas entering (or leaving) the lung per minute. It is equal to the tidal volume (TV) multiplied by the respiratory rate (f).
- VT = TV x f
- Alveolar ventilation
- The total volume of fresh air entering the alveoli per minute.
- VA = (TV – VD) x f
- Where VD is the anatomical dead space
Define partial pressures.
- Partial pressure is the notional pressure of that constituent gas if it alone occupied the entire volume of the original mixture at the same temperature.
- The total pressure of an ideal gas mixture is the sum of the partial pressures of the gases in the mixture.
What are the units for partial pressures?
- mmHg
- kPa
What is the alveolar gas equation?
PAO2 = PIO2 - PACO2/R
Where:
- PAO2 = Partial pressure of oxygen in the alveoli
- PIO2 = Partial pressure of oxygen in inspired air
- PACO2 = Partial pressure of carbon dioxide in alveoli
- R = Respiratory quotient = CO2 production / Oxygen consumption = Approx. 0.8
How are lung volumes and capacities measured?
- Lung volumes measured using a spirometer. Changes in volume of spirometer are equal and opposite to changes in lungs of subjects.
- The absolute volumes (functional residual capacity and residual volume) cannot be measured directly with spirometer since the last part of the gas cannot be breathed out. Instead helium dilation is used.
What is the difference between lung volumes and capacities?
Lung capacities are made up of 2 or more lung volumes.
What are the main lung volumes and capacities you need to know?
- Tidal volume
- Vital capacity
- Functional residual capacity
What are the main lung volumes and lung capacities (including those you don’t need to know)?
Draw these on a graph and highlight the ones you need to know.
There are 4 volumes and 4 capacities.

What is the tidal volume, what is the symbol and what is the normal value?
- The lung volume representing the normal volume of air displaced between normal inhalation and exhalation when extra effort is not applied.
- Symbol: VT or TV
- Typical value: 0.5L

How is tidal volume measured?
- Spirometry
- The height of normal breathing waves is measured
What is the vital capacity, what is the symbol and what is the normal value?
- The maximum amount of air a person can expel from the lungs after a maximum inhalation. It is equal to the sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume.
- Symbol: VC
- Normal value: 5L

How is vital capacity measured?
- Spirometry
- The height of the peak and trough that is created by a full inspiration followed by a full expiration
What is the functional residual capacity, what is the symbol and what is the normal value?
- The volume of air present in the lungs at the end of passive expiration. At FRC, the opposing elastic recoil forces of the lungs and chest wall are in equilibrium and there is no exertion by the diaphragm or other respiratory muscles.
- Symbol: FRC
- Normal value: 3L

How is functional residual capacity measured?
- Helium dilution
- It is based on the repeated breathing in and out of an oxygen and helium mixture in a closed system (spirometer) until equilibrium throughout the system is reached.
- The concentrations of the helium before and after are used to calculate the FRC.

What is the sign of intrapleural pressure and how does this arise at FRC? Give an average value.
- The pressure within the pleural cavity is slightly less than the atmospheric pressure, in what is known as negative pressure.
- At FRC, the force of the ribcage springing outwards is balanced by tendency of the lungs to collapse, which generates a negative intrapleural pressure
- Taking the pressure in the lungs (atmospheric pressure) to be 0 cmH2O, the intrapleural pressure is on average -6 cmH2O

Describe the intrapleural pressure when the lungs are inflated 1L above FRC.
- The intrapleural pressure becomes more negative, at -11 cmH2O
- This is because the effect of breathing in lifts rib cage and lowers diaphragm.
- The more negative pressure in the pleural space holds the lung in a more stretched position.

What is pneumothorax?
- A collapsed lung.
- A pneumothorax occurs when air leaks into the space between your lung and chest wall.
- This air pushes on the outside of your lung and makes it collapse.
Describe the pressure gradients in the intrapleural space and explain the consequences of this.
- Pressure gradient occur in pleural space, due to weight of lungs.
- At FRC lungs ca 32 cm tall and have a density of ca ¼ that of water, and so the pressure change from top to bottom (gh) = ¼ x 32 = 8 cmH2O.
- Consequence of above is that the bottom of the lung is more squashed than top and so inflates unevenly.
Describe the concept of regional ventilation.

What is compliance equal to?
C = V/P (ml/cmH20)
Describe the graph of % vital capacity against airway pressure for:
- Isolated lung
- Chest only
- Lung + chest wall

Derive the relationship between compliance for isolated lung (CL), chest wall (CCW) and total compliance (CT).

Give typical values for compliance of isolated lung (CL), chest wall (CCW) and total compliance (CT).
Values vary over inflation. Typically:
- CT = 200 ml/cmH2O
- CL = 400 ml/cmH2O
- CCW = 400 ml/cmH2O
What is surface tension?
The tension of the surface film of a liquid caused by the attraction of the particles in the surface layer by the bulk of the liquid, which tends to minimize surface area.
Compare the pressure-volume graphs for the inflation of lungs using air and saline. What does this suggest?
- Lungs can be inflated much more easily with liquid than with gas.
- Suggests surface tension is important part of elasticity of the lung.

Describe Laplace’s equaion with relation to the lungs.

What is the importance of surfactant?
- At a water-air surface, T = 70mN/m
- In order not to collapse, the lungs need a lower T of around 20mN/m.
- Surfactant is important in lowering surface tension, but it is not clear whether acts as a traditional surfactant, or whether helps maintain a mostly dry epithelium (like teflon saucepan).
What is a surfactant?
Surfactants are compounds that lower the surface tension (or interfacial tension) between two liquids, between a gas and a liquid, or between a liquid and a solid.
What is the surfactant in the lungs?
Dipalmitoyl lecithin
Give some clinical relevance of surfactant in the lungs.
Premature babies can lack surfactant, and their lungs become damaged (hyaline membrane disease) by high pressures used to ventilate them (not strong enough to ventilate these stiff lungs by themselves).
What are the two types of air flow in the lungs?
- Laminar
- Turbulent
What determines whether flow will be laminar or turbulent?
- Reynolds number
- This is a quantity that depends on multiple factors, including the diameter of the tube, density, viscosity and velocity
Draw laminar and turbulent flow in the airways and what their corresponding Reynolds numbers are.

Compare how flow in the airways varies with the pressure gradient in laminar and turbulent flow.
Laminar:
- Flow is proportional to the pressure gradient
- This is via Poiseuille’s Law (see below)
Turbulent:
- Flow is proportional to the square root of the pressure gradient

In the lungs, is most flow laminar or turbulent?
- In lung, conditions are almost always for laminar flow (Re < 2,000), but the lungs complicated branching pattern means there may be eddies and that the flow is non-steady.
- Turbulent flow leads to wheeze.
What is the equation for airway resistance?

Describe how airway resistance may be measured.

Draw the graph of the resistance of the airways along the different generations of the airway.

Explain why the airway resistance falls beyond approximately the 5th generation.
Although airway resistance is very much larger in smaller tubes, this factor is more than countered by the increasing total cross-sectional area at each generation of the airways.
Draw a graph to show how resistance and conductance vary with lung volume.

What is peak expiratory flow, what is the symbol and units? How is it measured?
- The maximal flow achieved during maximally forced expiration initiated at full inspiration
- Symbol: PEF
- Units: L/min
- Measured using a handheld meter (peak flow meter) or spirometry
What is forced expiratory volume in one second, what is the symbol and units? How is it measured?
- It is the volume breathed out in the first second in forced expiration following deep inhalation
- Symbol: FEV1
- Units: L
- Meausured using spirometry
Draw a graph to show how flow varies during expiration with maximal effort and submaximal effort.

Explain why flow during the second part of expiration occurs at the same rate with maximal effort and submaximal effort.

Distniguish between obstructive and restrictive lung disease. Include how these may be differentiated clinically.
Restrictive disease:
- Characterised by either intrinsic or extrinsic factors that prevent full expansion of the lungs, so that their capacity is reduced.
- e.g. Pulmonary fibrosis
- Clinically show reduced capacities (e.g. FVC), which tend to be normal in obstructive diseases
Obstructive disease:
- Characterised by airway obstruction
- e.g. Asthma
- Clinically FEV1/FVC ratios are used to classify the severity of obstructive pulmonary diseases -> This ratio is relatively unchanged in restrictive diseases since both FEV1 and FVC reduce roughly proportionally
Characterise restrictive and obstructive lung diseases by the changes to lung properties.
- Restrictive = Low lung elasticity (general)
- Obstructive = High lung resistance
What is COPD?
Chronic obstructive pulmonary disease (COPD) is the name for a group of lung conditions that cause breathing difficulties. It includes:
- Emphysema -> Damage to the air sacs in the lungs
- Chronic bronchitis -> Long-term inflammation of the airways
Describe airway closure.

Derive the two definitions of work done in breathing.

Draw a pressure-volume graph for breathing, marking the areas of elastic work and viscous work.

With stiff lungs, how does the patient tend to breathe? How does this manifest on the pressure-volume loop?

With increased airway resistance, how does the patient tend to breathe? How does this manifest in the pressure-volume loop?

Does diffusion occur due to any pressures?
No, it is all due to the random motion of particles (i.e. due to chance).
State Fick’s law of diffusion.

What is Henry’s Law?
C = αP
Where:
- C = Concentration of gas in a liquid
- α = Solubility
- P = Partial pressure of gas above liquid
In other words, the amount of dissolved gas in a liquid is proportional to its partial pressure above the liquid
Using Fick’s law and Henry’s law, derive an equation for the flux of gas across the lungs.

What is diffusing capacity?
- Diffusing capacity is a measure of how well oxygen and carbon dioxide are transferred (diffused) between the lungs and the blood.
- In equations, it often represents:

What are DO2 and DCO2 and what are the typical values?
- They are the diffusing capacities for oxygen and carbon dioxide in the lungs

What is perfusion and diffusion limited gas transfer in the lungs? [EXTRA]
- Perfusion limited
- When the blood oxygen comes into equilibrium with the alveolar gas.
- The amount of gas exchange can be increased by increasing the blood flow, but not the diffusing capacity
- Diffusion limited
- When the blood oxygen does not come into equilibrium with the alveolar gas.
- The amount of gas exchange can be increased by increasing the diffusing capacity, but not the blood flow
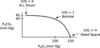
Draw a graph to show the difference between diffusion limited and perfusion limited gas exchange in the lungs.