3-22 Infections in the CNS II Flashcards
What is Subacute sclerosing panencephalitis?
Subacute sclerosing panencephalitis (SSPE) is a rare condition that occurs in children and adolescents several years after an acute episode of measles, usually that occurred before two years of age.
What is the course of SSPE?
5-15 years after an acute episode of measles, usually that occurred before two years of age, the child typically begins having problems in school and behavioral changes.
Several months after this, seizures and motor problems appear. In almost all cases the disease progresses to coma and death.
CSF shows increased IgG most of which is directed against the measles virus
What is present in brains of kids who have had SSPE?

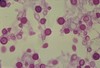
In patients with subacute sclerosing panencephalitis (SSPE) the brain demonstrates diffuse chronic encephalitis (black arrow) within both the grey and white matter. In this microscopic picture there is gliosis (red arrow) in the brain parenchyma and perivascular inflammation
What does SSPE show microscopically?

: This higher power shows the intranuclear inclusions (arrow) in subacute sclerosing panencephalitis (SSPE). Note that one inclusion has a clear halo around it and the other inclusion appears to fill the entire nucleus. Both nuclei demonstrate margination of the chromatin, which is characteristic of intranuclear viral inclusions
What is present in images of SSPE on EM?

This electron micrograph demonstrates the elongated nucleocapsids of measles (arrow), a paramyxovirus. This was from a patient with subacute sclerosing panencephalitis (SSPE).
How is the CNS involved in the sequelae of AIDS? Is it all due to the HIV virus, or related problems?
- Direct: HIV encephalitis.
- Indirect:
- Infectious: Toxoplasmosis, Cryptococcus, PML.
- Neoplastic: Lymphoma.
What 5 diseases can cause altered mental status in AIDS patients?
Toxoplasmosis
Cryptococcus
Primary Lymphoma
PML
HIV dementia
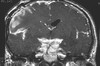
What is the pathology, presentation and Dx of toxoplasmosis in AIDS patients with altered mental status?
Pathology - CD4+ count < 100 /mL, abscess forming
Presentation - Highly variable, typically subacute with focal loss
Imaging (multiple ring-enhancing lesions), CSF PCR for T. gondi DNA
What is the pathology, presentation and Dx of Cryptococcus in AIDS patients with altered mental status?
Pathology - CD4+ count < 50 /mL, hematogenous from lungs, meningoencephalitis
Presentation - Chronic, headache, fever, malaise
Dx - CSF: ↑ICP, culture or antigen (+)
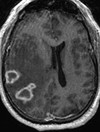
What is the pathology, presentation and Dx of Primary Lymphoma in AIDS patients with altered mental status?
Pathology - CD4+ count < 100 /mL, EBV transformation, DLBCL
Presentation - Chronic ↓mental status, headache, no fever, localizing signs
Dx - Single solid mass; biopsy
What is the pathology, presentation and Dx of PML in AIDS patients with altered mental status?
Pathology - CD4+ count <200 /mL , re-activation polyoma virus (JC) in oligodendrocytes, demyelination
Presentation - Progression of multifocal symptoms over weeks
Dx - CT non-enhancing white matter lesions, no mass effect
What is the pathology, presentation and Dx of HIV dementia in AIDS patients with altered mental status?
Pathology - CD4+ count <200 /mL, infection of neural cells with direct and immune damage
Presentation - Broad neuropsychiatric and motor deterioration to dementia over months
Dx - Clinical diagnosis, imaging is supportive (atrophy)
What’s this?

Microscopically in HIV dementia there are perivascular multinucleated cells (black arrows). These cells can be infected by HIV. There are very few lymphocytes present due to the disease, which markedly reduces CD4 (helper) lymphocytes
What are some fungal and mycobacterial organisms that can cause meningitis or meningoencephalitis?
•Fungal organisms
–Cryptococcal meningitis
•Mycobacteria
–M. tuberculosis or M. avium-intracellulare
–Common in patients with miliary TB
–Tends to involve the base of the brain