2. Anatomy and Physiology 2 Flashcards
Neuromuscular junction This is the 2nd synapse in which spinal tract?
Lateral corticospinal tract
Lower vs. Upper motor neuron lesion
Lower MN lesion = everything lowered (less muscle mass, decr muscle tone, decr reflexes, downgoing toes) Upper MN = everythinig up (tone, DTRs, toes)
Spinal tract: UMN vs. LMN lesion: Weakness
Both
What motor neuron sign is present in both UMN and LMN lesions?
Weakness
Spinal tract: UMN vs. LMN lesion: Atrophy
Atrophy in LMN only
Spinal tract: UMN vs. LMN lesion: Fasciculations (muscle twitching)
Present in LMN lesions only
What motor neuron signs are only present in LMN lesions?
Atrophy and fasciculations/fibrillations
Spinal tract: UMN vs. LMN lesion: Reflexes
Increased in UMN Decreased in LMN
Does UMN/LMN lesions lead to increased, decreased or the same reflex?
UMN vs. LMN lesion: Reflexes
Spinal tract: UMN vs. LMN lesion: Tone
Increased in UMN, decreased in LMN
What is increased in UMN lesion but decreased in LMN?
UMN vs. LMN lesion: Tone
Spinal tract: UMN vs. LMN lesion: Babinski sign (upgoing toes – normal in infants)
(+) in UMN, (-) in LMN
What does Babinski sign suggest about lesion?
UMN
Spinal tract: UMN vs. LMN lesion: Spastic paralysis
(+) in UMN (-) in LMN
What lesion does clasp knife spasticity suggest?
UMN
Spinal cord lesions: Poliomyelitis and Werdnig-Hoffmann disease What areas are affected? What are the Sx?
Lower motor neuron lesion only, due to destruction of anterior horns; flaccid paralysis

Lower motor neuron lesion only, due to destruction of anterior horns; flaccid paralysis What diseases (2) are associated with this?
Poliomyelitis and Werdnig-Hoffmann disease
Spinal cord lesions: Multiple sclerosis What areas are affected? What are the Sx?
Mostly white matter of cervical region; random and asymmetric lesions, due to demyelination; scanning speech, intention tremor, nystagmus

Mostly white matter of cervical region; random and asymmetric lesions, due to demyelination; scanning speech, intention tremor, nystagmus What disease is associated with this?
Multiple sclerosis
Spinal cord lesions: ALS What areas are affected? What are the Sx?
Combined upper and lower motor neuron deficits with no sensory deficit; both upper and lower motor neuron signs.

Combined upper and lower motor neuron deficits with no sensory deficit; both upper and lower motor neuron signs. What disease is associated with this?
ALS
Spinal cord lesions: Complete occlusion of the anterior spinal artery What areas are affected? What are the Sx?
Spares dorsal columns and tract of Lissauer; upper throacic ASA territory is a watershed area, as artery of Adamkiewicz supplies ASA below ~T8
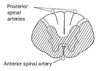
Spares dorsal columns and tract of Lissauer; upper throacic ASA territory is a watershed area, as artery of Adamkiewicz supplies ASA below ~T8 What disease is associated with this?
Complete occlusion of the anterior spinal artery
Spinal cord lesions: Tabes dorsalis (tertiary syphilis) What areas are affected? What are the Sx?
Degeneration of dorsal roots and dorsal columns; impaired proprioception, locomotor ataxia

Degeneration of dorsal roots and dorsal columns; impaired proprioception, locomotor ataxia What disease is associated with this?
Tabes dorsalis (tertiary syphilis)
Spinal cord lesions: Syringomyelia What areas are affected? What are the Sx?
Crossing fibers of spinothalamic tract damaged (2nd order neuron); bilateral loss of pain and temperature sensation. (usually C8-T1); seen with Chiari I types 1 and 2; can expand and affect other tracts

Crossing fibers of spinothalamic tract damaged; bilateral loss of pain and temperature sensation. What disease is associated with this?
Syringomyelia
Spinal cord lesions: Vitamin B12 neuropathy, Vitamin E deficiency and Friedrich’s ataxia What areas are affected? What are the Sx?
Demyelination of dorsal columns, lateral corticospinal tracts, and spinocerebellar tracts; ataxic gait, hyporeflexia, impaired position and vibration sense.

Demyelination of dorsal columns, lateral corticospinal tracts, and spinocerebellar tracts; ataxic gait, hyperreflexia, impaired position and vibration sense. What diseases (3) are associated with this?
Vitamin B12 neuropathy, Vitamin E deficiency and Friedrich’s ataxia
Poliomyelitis: Cause and Transmission?
Cause: poliovirus (fecal-oral) and replicates in oropharynx and small intestines -> spreads through bloodstream to CNS -> destruction of cells in anterior horn of spinal cord, leading in turn to LMN destruction.
Poliomyelitis: Sx?
Malaise, hedache, fever, nausea, abdominal pain, sore throat. Signs of LMN lesions – muscle weakness and atrophy, fasciculations, fibrillation, and hyporeflexia.
Poliomyelitis: Findings?
CSF w/ lymphocytic pleocytosis w/ slight elevation of protein (w/ no change in CSF glucose). Virus recovered from stool or throat.
Werdnig-Hoffman dz. Genetics, Presentations and Prognosis
Infantile spinal muscular atrophy; Autosomal-recessive inheritance; presents at birth as a “floppy baby,” tongue fasciculations; median age of death 7 months. Associated w/ degeneration of anterior horns. LMN involvement only.
Amyotrophic lateral sclerosis (commonly known as Lou Gehrig’s dz). Clinical presentation, genetics, treatment.
Associated with LMN and UMN signs; no sensory, cognitive or oculomotor deficits. Can be caused by superoxide dismutase 1 (SOD1). Commonly presents as fasciculations and eventual atrophy; progressive and fatal. Riluzole treatment modestly lengthens survival by decreasing presynaptic glutamate release; associated with betel nut ingestion.
Tabes dorsalis. Etiology and Clinical presentations.
Degeneration of dorsal columns and dorsal roots due to tertiary syphilis, resulting in impaired proprioception and locomotor ataxia. Argyll Robertson pupils
Associated with Tabes dorsalis
Charcot’s joints (neuropathic arthropathy), Shooting (lightning) pain, Argyll Robertson pupils (accomodate, but do not react), Absence of deep tendon reflexes, positive Romberg, sensory ataxia at night.
Friedrich’s ataxia: Genetics, Etiology, and Presentation
Autosomal-recessive trinucleotide repeat disorder (GAA) in frataxin gene -> impairment in mitochondrial functioning; staggering gait, frequent falling, nystagmus, dysarthria, pes cavus (high arch), hammer toes, hypertrophic cardiomyopathy (cause of death). Presents in childhood with kyphoscoliosis.
Brown-Séquard Syndrome: What is it?
Hemisection of the spinal cord

Brown-Séquard Syndrome: Findings?
1.) Ipsilateral UMN signs (corticospinal tract) below lesion 2.) Ipsilateral loss of tactile, vibration, proprioception sense (dorsal column) below lesion 3.) Contralateral pain and temperature loss (spinothalamic tract) below lesion 4.) Ipsilateral loss of all sensation at level of lesion 5.) LMN signs (e.g., flaccid paralysis) at level of lesion
If lesion occurs above T1, presents w/ Horner’s syndrome

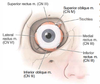
Horner’s syndrome. Symptoms and Etiology.
Sympathectomy of face: 1.) P tosis (slight drooping of eyelid) 2.) A nhidrosis (absence of sweating) and flushing (rubor) of affected side of face 3.) M iosis (pupil constriction)
Associated w/ lesion of spinal cord above T1 (e.g., Pancoast (pulmonary sulcus) tumor, Brown-Séquard syndrome (cord hemisection), late-stage syringomyelia)
3-Neuron oculosympathetic pathway involved in Horner’s syndrome
- Hypothalamus -> intermediolateral column of spinal cord; synapse in lateral horn (T1)
- Second neuron projects to up sympathetic trunk to superior cervical ganglion (C2)
- Third neuron sends projects along external carotid artery to sweat glands of face, along opthalmic division of trigeminal nerve to smooth muscles of eyelids and pupillary dilator.
Interruption of any of these pathways result in Horner’s syndrome.

Clinically important landmarks for a pudendal nerve block (to relieve pain of pregnancy)
Ischial spine
Clinically important landmarks for Appendix
2/3 of the way from the umbilicus to the anterior superior iliac spine (McBurney’s point)
Clinically important landmarks for lumbar puncture
Iliac crest.
Landmark dermatomes: C2
Posterior half of a skull “cap”

Landmark dermatomes: C3
High turtleneck shirt
Landmark dermatomes: C4
Low-collar shirt
Landmark dermatomes: T4
At the nipple. (T4 at the teat pore )
Landmark dermatomes: T7
Xiphoid process
Landmark dermatomes: T10
At the umbilicus (important for early appendicitis pain referral) (T10 at the belly butTEN )
Landmark dermatomes: L1
At the inguinal ligament (“L1 is IL [I nguinal L igament])
Landmark dermatomes: L4
Includes kneecaps
Landmark dermatomes: S2, S3, S4
Erection and sensation of penile and anal zones (“S2, 3, 4, keep the penis off the floor”)
Muscle spindles vs. Golgi tendon organs
Muscle spindles monitor muscle length (help you pick up a heavy suitcase when you didnt know how heavy it was). Golgi T endon organs monitor muscle T ension (make you drop a heavy suitcase you’ve been holding too long).
Muscle spindle: pathway?
In parallel with muscle fibers. Muscle stretch –> intrafusal stretch –> stimulates Ia afferent –> stimulate alpha motor neuron –> reflex muscle (extrafusal) contraction
Spindle muscle control: the Gamma loop
CNS stimulates gamma motor neuron –> contracts intrafusal fiber –> increased sensitivity of reflex arc
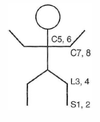
Clinical reflexes and their respective nerve roots: Achilles? Patella? Biceps? Triceps?
Achilles = S1 nerve root; Patella = L4 nerve root; Biceps = C5 nerve root; Triceps = C7 nerve root
*Note that they count up in order: S1,2 L3,4 C5,6 C7,8
Babinski sign
Dorsiflexion of the big toe and fanning of other toes; sign of UMN lesion, but normal reflex in 1st year of life.
Primitive reflexes. When do they disappear or reappear? What are they (6)
Normally disappear within 1st year of life. May reemerge following frontal lobe lesion.
Include: Moro reflex (3-6 months), rooting reflex (most immediate survival), suckling reflex, palmar and plantar reflexes (1-2 months), Babinski reflex (1 year), Galant reflex.
Moro reflex
“hang on for life” reflex - abduct/extend limbs when startled, and then draw together; 3-6 months disappear
Rooting reflex
Movement of head toward one side if cheek or mouth is stroked (nipple seeking)
Sucking reflex
Sucking response when roof of mouth is touched
Palmar and palantar reflexes
Curling of fingers/toes if palms of hands/feet are stroked (1-2 months)
Galant reflex
Stroking along one side of the spine while newborn is in ventral suspension (face down) causes lateral flexion of lower body toward stimulated side.
Cranial nerves that lie medially at the brainstem
III, VI, XII Remember: 3 (x2) = 6 (x2) = 12

Which cranial nerve arises dorsally and emerges ventrally?
CN IV
Dorsal brainstem structures: Pineal gland
Melatonin secretion, circadian rhythms.
Dorsal brainstem structures: superior colliculi
Conjugate vertical gaze center. (“you have your eyes above your ears, and the superior colliculus (visual) is above the inferior colliculus (auditory).”)
Dorsal brainstem structures: inferior colliculi
Auditory (“you have your eyes above your ears, and the superior colliculus (visual) is above the inferior colliculus (auditory).”)