1.7 PHYS - Cardiac Electrophys Flashcards
Define the following:
Inotropy:
Dromotropy:
Chronotropy:
Inotropy: contraction of myocardium.
Dromotropy: conduction velocity of atroventricular node.
Chronotropy: firing of sinoatrial node.
Give the flow of the electrical conduction system through the heart.
SA node -> Atrial muscle -> AV node -> held -> Bundle of His -> R + L bundle branches -> Purkinje fibers -> Ventricular muscle
How is the SA node activated? Why is the electrical conduction held when it reaches the AV node?
SA node tissue is automatic (shows automaticity), it activates itself and starts the impulse itself.
The AV node holds the impulse in order to give time to the ventricles to fill with blood from the atria.
Name the location and controlling rate of autorthymic cells in the heart.
SinoAtrial Node (SA node): “Pacemaker” of heart, 60-100bpm, near opening of superior vena cava on Right atrium.
- Atria autorhythmicity cells in atria, 60-80bpm.
AtrioVentricular Node (AV node): base of right atrium, separates atria and ventricles, 40-60, autorhythmic cells located in distal portion of AV node.
Bundle of His/ Purkinje fibers (ventricular portion): Bundle of His is right below AV node and branches into right and left bundle branches, Purkinje fibers are small terminal fibers extending from Bundle of His - spread throughout ventricular myocardium. 20-40bpm.
Give roughly the timeframe for action potentials at the following areas of the heart: SA node, AV node, AV bundle, Ventricular septum, Ventricular myocardium.
SA Node: 0.00sec
AV Node: 0.03sec
AV Bundle: 0.12sec
Ventricular Septum: 0.16sec
Ventricular Myocardium: 0.20 - 0.22sec
What happens to conduction in the heart if the SA node fails? Go sequentially down that list. What is an ectopic focus?
If SA Node fails Atrial autorhythmic cells will take over, AV Node will take over after that, then Ventricular autorhymthic cells will take over.
Ectopic Focus: is a group of excitable cells that are acting outside the pacing of the SA node, this excitement can cause a large increase in heart rate (upwards of 130bpm).
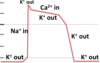
Name the phases and what is occurring in this SinoAtrial Node action potential?

Phase 4: rising depolarization of SA nodal action potential. Due to pacemaker current (If) or “funny” current. Slow inward movement of Na+ is taking place.
Phase 0: depolarization due to increased Ca++ permeability through L-type Ca+ channels. These channels open when membrane is depolarized to ~ -40mV.
Phase 3: voltage-dependent K+ channels open and increased K+ permeability repolarizes cell toward K+ equilibrium potential.

What are the areas of the brainstem invovled in cardivascular regulation? Name them and what they do.
Cardiac center: regulates heart rate and force of contraction.
Vasomotor center: regulates distribution of blood flow.
What is the effect of sympathetic/ parasympathetic input on the pacemaker, dromotropy, chronotropy, inotropy?
Sympathetic: increases activity of pacemaker => increased dromotropy, chronotropy, inotropy.
Parasympathetic: decreases activity of pacemaker => decreased dromotropy, chronotropy, and inotropy.
Broadly, what are the three major types of cardiac muscle?
1) Atrial muscle.
2) Ventricular muscle.
3) Specialized excitatory & conductive muscle fibers (autorhythmicity and conduction via gap junctions).
What are desmosomes, gap junctions, connexons, what resistance do these have and why does that matter in cardiac tissue? How do these contribute to syncytia?
Gap junctions: connections between cardiac muscle cells that allow exchange of chemical information.
Connexons: proteins that make up gap junctions.
Low resistance: 1/400th of cell membrane resistance, low resistance allows for movement of ions from cell to cell.
Desmosomes: connections between cardiac cells that keep them mechanically connected.
Syncytia: atrial and ventricular syncytia, means all their muscle cells work in synchrony together, this is due to these cellular connections mentioned above.
Where are fast acting Na+ channels located: autorhythmic cells or myocardial cells?
Myocardial cells.
Absent in autorhymthic cells, these have the funny current that begins the depolarization.
How does the refractory period differ in skeletal or neural action potentials vs. cardiac myocyte action potentials? Why this difference? What is neccessary for another AP to be regenerated?
refractory period is much longer in cardiac tissue.
Excitable cells can’t have another AP until the voltage-gated Na+ channels are ready.
AP in cardiac tissue last longer therefore refractory period is longer.

Name the phases here, what is happening in each?

Notice the difference between ventricle and atrium action potentials, why this difference?

Atria don’t need plateau phase because the musce is smaller and thinner.
Shorter phase 2.
How is the force of cardiac muscle contraction increased? How does this differ from skeletal muscle?
Cardiomyocytes are stimulated to depolarize and contract in sequence, therefore you cannot just summate or recruite more muscle cells like you can in skeletal muscle.
1) increase the length of the sarcomere (stretch myocytes) Starling’s Law.
2) Increase muscle contractility, involves increasing Ca+ content.
What is Starling’s Law again?
The greater the volume of blood entering the heart during diastole (end-diastolic volume), the greater the volume of blood ejected during systolic contraction (stroke volume).


